Neurologist (algologist)
Vasilenko
Marina Gennadievna
25 years of experience
Head of the Pain Treatment Center, neurologist-algologist, member of the Society of Neurologists and Neurosurgeons, Russian Society for the Study of Pain, Association of Interdisciplinary Medicine, International Association for the Study of Pain (IASP)
Make an appointment
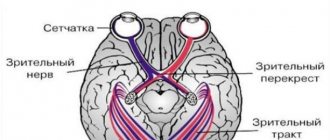
The trigeminal nerve is the largest of the 12 cranial nerves, specifically their fifth pair. It belongs to the nerves of a mixed type and includes very sensitive fibers. This name is due to the fact that the nerve is divided into three branches, providing mobility and sensitivity of the face, mucous membranes of the mouth and teeth. These are the ophthalmic, maxillary and mandibular branches.
Inflammation of the trigeminal nerve is a serious pathology that causes severe pain in the facial area. Otherwise it is called neuritis. In turn, neuralgia is pain along the trigeminal nerve. It can act as an independent sensitivity disorder, but it often accompanies inflammation, i.e. neuritis.
Symptoms and signs
Acute trigeminal neuralgia causes sudden and very severe pain along the nerve fiber. It manifests itself in attacks and is shooting and burning in nature. On average, the duration of an attack is up to 3 minutes; in approximately 7% of patients it lasts up to 3 days. Their number can reach 200 per day.
Pain from trigeminal neuralgia can be observed in different parts of the face. It all depends on which branch of the nerve was affected:
- if maxillary - in the area of the facial muscles, upper jaw and nose.
- mandibular – the pain will resemble a toothache.
- ophthalmic – in the area of the temples, forehead and above the eyebrows.
Against the background of pain, the patient develops increased anxiety and even phobias. A person strives to avoid those poses and movements that provoke unpleasant sensations in him. Other characteristic symptoms of inflammation of the trigeminal nerve:
- facial muscle spasms;
- increased salivation;
- increased or decreased sensitivity of facial skin;
- moderate increase in temperature;
- weakness and muscle pain.
Are you experiencing symptoms of trigeminal neuralgia?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Treatment at the Energy of Health clinic
If you or your relative are bothered by severe pain in one or another part of the face, the neurologists of the Health Energy clinic will come to the rescue. We will conduct a full diagnosis to identify the causes of the pathology and prescribe comprehensive treatment. At your service:
- modern drug regimens to reduce the frequency and intensity of attacks;
- physiotherapeutic procedures: magnetotherapy, laser therapy, electrophoresis, phonophoresis, etc.;
- delicate therapeutic massage;
- acupuncture;
- help from a psychologist if necessary.
Causes and risk factors
Neuralgia of the trigeminal nerve branch is a disease with many possible causes. First of all, this is compression by vessels: displaced arteries or veins. Inflammation can also be provoked by metabolic disorders and diseases that are associated with them. These are diabetes mellitus, gout and other similar pathologies.
There are other possible causes of trigeminal neuralgia:
- inflammations that occur during dental treatment;
- hypothermia (general or facial area);
- mental disorders;
- purulent diseases of the jaw bones or skull;
- infection of the body with worms;
- chronic caries or sinusitis;
- infectious and viral diseases (herpes, adenoviruses, mumps, pulmonary tuberculosis, herpes zoster);
- very severe allergies;
- brain tumors;
- inflammation of the outer, middle or inner ear;
- multiple sclerosis;
- too narrow canal of the facial nerve from birth;
- injuries or operations on the temporal bone.
Post-traumatic sensory nerve damage. Terminology.
The Association for the Study of Pain has standardized a nomenclature system that defines the most commonly used neurosensory descriptive terms Classification of Chronic Pain, Second Edition: International Association for the Study of Pain Task Force on Taxonomy, ed.: H Merskey and N. Bogduk. IASP Press IASP Council in Kyoto, November 29-30-2007.
- Paresthesia is a non-painful altered sensation. May be described by patients as a pins and needles, slight burning or tingling sensation. NEW sensations - stretching, pulling sensations.
- Dysesthesia is perverted sensations. Abnormal, sometimes unpleasant sensations experienced by a person with partial damage to sensory nerve fibers when touching the skin. - Unpleasant abnormal sensation, spontaneous or provoked. Note : Dysesthesia is not pain when it hurts or paresthesia. Special cases of dysesthesia are hyperalgesia and allodynia. Dysesthesia should always be unpleasant , and paresthesia should not be unpleasant, although it is recognized that the boundary can create some difficulties when it comes to whether these sensations are pleasant or unpleasant. It should always be stated whether the sensations are spontaneous or provoked.
- Neuropathic pain (IASP) is pain caused by damage or disease of the somatosensory nervous system.
- Neuropathy (IASP) is a dysfunction or pathological change in a nerve: in one nerve - mononeuropathy; in several nerves - mononeuropathic multiplex; if diffuse and bilateral - polyneuropathy. Note : Neuritis is a special case of neuropathy and is currently a term reserved for inflammatory processes affecting the nerves. - sensitive (touch, heat, pain) - motor (movement).
- Allodynia is pain from non-noxious stimuli (pain with light touch/cold/heat). The appearance of pain in response to a stimulus that does not cause pain in healthy people. Thermal allodynia, especially cold allodynia, is a feature of the extraoral dermatome in patients with IANIs. Some patients report decreased taste and heat sensitivity. Perversion of sensitivity is characterized by an increased threshold of sensitivity and increased duration of perception, lack of precise localization of sensations of an unpleasant nature, and a tendency to irradiate. The pain continues when the stimulus is removed.
- Hyperalgesia - increased sensitivity to painful stimuli
- Anesthesia - numbness
- Hyperesthesia and Hypostesthesia are terms that are often used to describe changes in sensitivity that increase or decrease, respectively.
Rice. 5 Anatomy of the II (maxillary) and III (mandibular) branches of the trigeminal nerve. It is important to note that the branches of the superior alveolar nerve retrogradely “merge” into the infraorbital nerve, which explains the symptoms of swelling and pain in the infraorbital region when the superior dental plexus is damaged.
Post-traumatic sensory neuropathy is pain that develops after medical intervention (surgery, treatment, anesthesia), with a minimum duration of 2 months, while other causes of pain are excluded (infection, persistent malignancy, misdiagnosis, etc.), preoperative pain from others must also be excluded reasons.
It is important to add that the neuropathic area does not have to be clearly indicated by the patient, however, about 80% of patients can localize and indicate the neuropathic area.
HERE you can read more about the incidence of “phantom toothache” (atypical odontalgia) after endodontic treatment, which is classified as persistent dentoalveolar pain (PDAP type 2) and occurs in up to 3% of cases.
Possible complications
Over time, symptoms of inflammation of the trigeminal nerve can give rise to neuropathic complications and lead to the development of secondary pain syndrome in the head. In the chronic form of the disease, the auditory and facial nerves are irritated. Without treatment, trigeminal neuralgia can lead to more serious complications:
- dystrophy of masticatory muscles;
- decreased sensitivity of the affected area;
- Sykinesia (cooperative movements in which one nerve controls many muscles);
- contracture and spontaneous contraction of the facial muscles;
- conjunctivitis.
Causes
Trigeminal neuropathy can be associated with a variety of conditions. Neuropathy can be caused by blood vessel compression on the trigeminal nerve as it exits the brainstem. This compression causes the protective covering around the nerve (myelin sheath) to wear or become damaged. Symptoms of trigeminal neuropathy can also occur in patients with multiple sclerosis, a disease that damages the myelin sheath of the trigeminal nerve. Rarely, symptoms of neuropathy may be due to nerve compression by a tumor or arteriovenous malformation. Damage to the trigeminal nerve (possibly as a result of oral surgery, stroke, or facial trauma) can also lead to neuropathic pain.
When to see a doctor
If you experience symptoms of trigeminal neuralgia, you should immediately consult a doctor, as it may be a sign of another serious disease. In the treatment of neurological pathologies, accurate and timely diagnosis is extremely important. This is done by a neurologist, with whom you can make an appointment at our clinic in the center of Moscow. The specialist knows not only how to relieve trigeminal neuralgia, but also how to correctly diagnose it in order to prescribe effective treatment in the future.
Prognosis of post-traumatic neuropathy
Important! It is impossible to classify the extent and prognosis of sensory nerve injury based on clinical findings early after injury. Thus, in order to assess the actual outcome of nerve damage, it is necessary to re-interview, examine and test the patient after 2 to 3 weeks of drug treatment.
Prognosis for recovery after injury to the inferior alveolar nerve during implantation:
Full recovery – 50%
Partial recovery – 44%
No signs of recovery – 6%
Diagnosis of trigeminal neuralgia
A preliminary diagnosis can be made by a neurologist based on the patient’s complaints, studying the history of his disease and an objective examination of the face with an assessment of symmetry at rest and when trying to smile. Also, during the consultation, the doctor may conduct additional tests, asking the patient to close his eyes, purse his lips, frown, etc.
Laboratory and instrumental diagnostics of trigeminal neuralgia include the following examinations:
- general blood and urine tests;
- computed tomography (CT) and magnetic resonance imaging (MRI);
- radiography of the paranasal sinuses;
- panoramic radiography of the oral cavity;
- electroneuromyography to determine the localization of inflammation.
Diagnostics
The neurologist makes a diagnosis based on the clinical picture, the patient's medical history, the results of a neurological examination and a physical examination. The doctor must rule out diseases that may manifest as facial pain (herpes, headaches). An accurate diagnosis is necessary in order to choose the right tactics for treating neuritis. With neuritis, palpation of the exit points of the trigeminal nerve is accompanied by painful sensations. Diagnosis includes MRI. This is necessary in order to exclude tumors and demyolinating diseases. The diagnosis can be confirmed by the positive effect of low-dose anticonvulsants or tricyclic antidepressants.
Treatment
Treatment of inflammation of the trigeminal nerve is carried out depending on the severity of symptoms. First, conservative therapy is prescribed. If this does not help, doctors resort to surgical methods. Their essence is to eliminate the cause of neuralgia. This may be compression of the nerve by the vessel. Surgical treatment is carried out using radiofrequency destruction, microvascular decompression or percutaneous surgery.
What drugs are most effective for the treatment of trigeminal neuralgia:
- antibiotics. Prescribed for infectious nature of the disease;
- glucocorticosteroids. Relieves severe inflammation in the body;
- non-steroidal anti-inflammatory drugs (NSAIDs). Helps suppress inflammatory processes;
- painkillers. Relieves soreness in the facial muscles;
- muscle relaxants.
To improve metabolic processes in the nervous tissue, the patient is prescribed B vitamins. How to relieve acute pain with trigeminal neuralgia:
- use anticonvulsants;
- provide physical rest, preferably bed rest;
- Apply an anti-inflammatory ointment or a warm compress to the site of pain.
Treatment of neuralgia
Treatment of neuralgia is a long and difficult process, but doctors at the CELT Pain Clinic know how to carry it out with maximum positive effect. For this, two treatment methods are used.
Conservative method of treating neuralgia
Conservative treatment involves taking medications:
- antispasmodics;
- anticonvulsants;
- non-steroidal anti-inflammatory drugs;
- glucocorticoids;
- anticholinesterase drugs;
- antidepressants;
- vitamins
It is very important to correctly calculate the dosage of medications (this is done by the doctor) and take them regularly (this is the patient’s function), since this is the only way to achieve the desired effect. In complex conservative therapy, physiotherapeutic methods of treatment - Bernard currents - help to achieve a good effect; acupuncture; paraffin applications, etc.
If conservative therapy does not bring the desired effect, the attending physician may decide on surgical treatment.
Surgical method for treating neuralgia
The following surgical treatment methods have proven themselves well:
- microvascular decompression of the root using implants that prevent compression on the nerve;
- radiofrequency destruction, which involves destruction of the nerve root;
- stereotactic radiosurgery (implies a targeted impact on the pathological focus with ionizing treatment using Gamma Knife and CyberKnife devices);
- balloon compression (carried out without violating the integrity of the skin) - a conductor with a balloon at the end is inserted into the area of the trigeminal nerve ganglion using a special needle. By inflating the balloon, the doctor compresses the nerve, which leads to its destruction and cessation of pain impulses.
In any case, the key to successful treatment is timely consultation with a doctor. Contact the CELT clinic, our specialists are always ready to help and relieve you of pain!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Home remedies
Before treating trigeminal neuralgia at home, you should consult a doctor, since many remedies can only worsen the situation. If the specialist allows it, it is also possible to use various home recipes.
According to recommendations for trigeminal neuralgia, it is worth consuming orally or lubricating the affected side with birch sap. You need to drink 4-5 glasses per day. Heated buckwheat folded in cotton cloth will help relieve pain. The compress is made 2 times a day, keeping it at the site of inflammation until it cools down. At home, it is useful to massage the sore area: rub, stroke and lightly knead the area of inflammation.
Basic information about the disease
Our two trigeminal nerves provide sensitivity to the face. One nerve passes on the left, the other on the right. Each has three branches.
With neuralgia of the right or left nerve, attacks of intense shooting pain begin in the locations of the branches of the nerve . Pain does not allow you to live an active life: for example, there are difficulties with eating and maintaining hygiene. You can get sick at any age. Women get sick more often.
The disease can occur on its own or be a complication of another disease.
Myths and dangerous misconceptions in treatment
Due to the fact that neuralgia does not affect the general condition of the body, many patients postpone visiting a doctor and treating the trigeminal nerve. In fact, this is the wrong approach, since the disease can lead to paralysis and muscle paresis. In addition, it has a significant impact on psychological and social aspects of life.
No less important is the fact that painkillers for trigeminal neuralgia provide only a temporary effect. Over time, anticonvulsant medications may also stop working as they become addictive. Therefore, you should not abuse medications. They only relieve the symptoms of neuralgia, and its cause can only be identified by a qualified specialist.
Prevention
There is no specific prevention against neuralgia. Doctors only recommend eliminating as much as possible exposure to the body of those risk factors that can lead to nerve inflammation. To avoid this, it is necessary to prevent hypothermia of the face, especially in the summer when using fans and air conditioners. It is important to harden yourself and worry less in order to reduce the impact of stress. It is also imperative to treat underlying diseases that are risk factors for neuralgia.