Melatonin is the most common sleep drug that can be found in pharmacies around the world and as a dietary supplement: it is produced in tablets, dragees, capsules, drops, and even in the form of gummy bears. This is a natural remedy - in the sense that melatonin from medications is no different from the one produced by the body itself. And it really does trigger sleep. But does this mean that a melatonin pill will help you get rid of insomnia? It is not that simple.
Detection of melatonin
In 1958, the team of Aaron Lerner, a professor of dermatology from Yale University in the USA, managed to isolate a new compound from the epiphyses of cows, which, when introduced into the skin of a tadpole, lightened it.
The substance blocked the production of melanocyte-stimulating hormone, which is why it was called “melatonin”. Later they discovered that the open compound is synthesized in the body mainly at night. This was associated with daily periods of rest and wakefulness, and for two decades melatonin was considered only a sleep hormone that regulates human circadian rhythms.
What is melatonin for?
Melatonin is a hormone produced by the pineal gland, or “pineal gland,” a part of the brain so called because it is shaped like a small bump.
Modern science believes that melatonin appeared billions of years ago, living beings began to produce it as a substance that captured oxygen molecules in the air when there was an excess of it. Now melatonin performs many important functions in our body and is known to support circadian rhythms. The circadian rhythm is the body's internal clock. It tells the body when to sleep and when to wake up.
Melatonin production
80% of melatonin is produced by the pineal gland, a 100-125 mg pineal gland located in the brain. The remaining 20% of melatonin is produced by special cells:
- digestive tract;
- bronchi and lungs;
- kidney;
- pancreas;
- prostate and ovaries;
- retina, other organs and tissues.
Melatonin is produced even by blood cells: eosinophils and lymphocytes.
This discovery was made in 1974 by Soviet scientists Nathan Tanfelevich Raikhlin and Igor Moiseevich Kvetnoy. This “peripheral” melatonin does not affect circadian rhythms, working exclusively at the local level.
Action of melatonin
The “sleep hormone”
begins to be produced between 20 and 22 hours (earlier for early risers, later for night owls). The concentration of melatonin peaks from midnight to two o'clock in the morning, and by six to seven o'clock in the morning it drops to its minimum level.
How does melatonin work?
- Absorbs free radicals - unstable molecules that damage organs and tissues, lead to decreased immunity, the development of tumors and cardiovascular diseases.
- It is the strongest natural immunomodulator, restores damaged cells, prevents diseases, including cancer.
- It has a pronounced chronobiotic effect: it regulates daily and seasonal biorhythms.
- Promotes sleep, is responsible for calm restorative sleep, bringing natural rest.
- Regulates the functioning of the endocrine system, normalizes body temperature.
- Acts as an antidepressant and prevents the occurrence of certain mental disorders.
- Slows down the rate of aging, increases life expectancy.
What lowers melatonin levels?
- Age. After 45-50 years, the production of natural melatonin decreases.
- Light. The pineal gland can only produce melatonin in the dark. If the lights are turned on at night, the production of the hormone slows down until it stops completely. The glow of the screens of a mobile phone, tablet, laptop, computer or TV reduces the synthesis of melatonin.
- Smoking.
- Drinking alcoholic or caffeinated drinks.
- Taking nonsteroidal anti-inflammatory drugs (NSAIDs), vitamin B12, and some other medications.
What increases melatonin production?
- Lack of light at bedtime
- Calcium
- Magnesium
- Vitamin B6
- A nicotinic acid.
Melatonin-SZ
Registration number
LP-004758
Dosage form
film-coated tablets
Compound
1 tablet contains:
active ingredients, melatonin - Zmg excipients, microcrystalline cellulose - 48.5 mg: sodium carboxymethyl starch - 6.5 mg; calcium hydrogen phosphate dihydrate - 41.0 mg; magnesium stearate - 1.0 mg
shell composition: hypromellose - 1.53 mg; polysorbate-80 (Tween-80) - 0.64 mg; talc - 0.51 mg; titanium dioxide E 171-0.32 mg.
Description
White or almost white, film-coated tablets, round, biconvex, scored on one side. In cross-section, the core of the tablet is white or almost white
ATX code
[N05CH01]
Pharmacological properties
Pharmacodynamics
A synthetic analogue of the pineal gland hormone (epiphysis); has an adaptogenic, sedative, hypnotic effect. Normalizes circadian rhythms. Increases the concentration of gamma-aminobutyric acid (GABA) and serotonin in the midbrain and hypothalamus, changes the activity of pyridoxal kinase, which is involved in the synthesis of GABA, dopamine and serotonin. Regulates the sleep-wake cycle, daily changes in locomotor activity and body temperature, has a positive effect on the intellectual and mnestic functions of the brain, on the emotional and personal sphere. Helps organize biological rhythm and normalize night sleep. Improves sleep quality, speeds up falling asleep, regulates neuroendocrine functions. Adapts the body of weather-sensitive people to changes in weather conditions. Pharmacokinetics Absorption
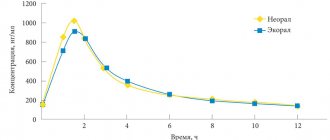
Melatonin after oral administration is quickly absorbed from the gastrointestinal tract. In elderly people, the rate of absorption may be reduced by 50%. The kinetics of melatonin in the range of 2 - 8 mg is linear. When taken orally at a dose of 3 mg, Sta> in blood plasma and saliva is achieved after 20 minutes and 60 minutes, respectively. The time to reach the maximum concentration of Tta> in the blood serum is 60 minutes (normal range 20-90 minutes). After taking 3-6 mg melatonin, the maximum concentration of Cax in the blood serum is usually 10 times higher than the endogenous melatonin in the blood serum at night. Concomitant meals delay the absorption of melatonin.
Bioavailability
Oral bioavailability of melatonin ranges from 9 to 33% (approximately 15%).
Distribution
In in vitro studies, the binding of melatonin to plasma proteins is 60%. Melatonin mainly binds to albumin, acidic glycoprotein and high-density lipoproteins. The distribution volume Vd is about 35 liters. It is quickly distributed into saliva and passes through the blood-brain barrier and is detected in the placenta. The concentration in cerebrospinal fluid is 2.5 times lower than in plasma.
Biotransformation
Melatonin is metabolized primarily in the liver. After oral administration, melatonin undergoes significant transformation during its initial passage through the liver, where it is hydroxylated and conjugated with sulfate and glucuronide to form 6-sulfatoxymelatonin; the level of first-pass metabolism can reach 85%. Experimental studies suggest that isoenzymes CYP1A1, CYP1A2 and, possibly, CYP2C19 of the cytochrome P450 system are involved in the metabolism of melatonin. The main metabolite of melatonin, 6-sulfatoxymelatonin, is inactive.
Selection
Melatonin is excreted from the body by the kidneys. The average half-life (T|/2) of melatonin is 45 minutes. Excretion is carried out in the urine, about 90% in the form of sulfate and glucuronic conjugates of 6-hydroxymelatonin, and about 2% - 10% were excreted unchanged.
Pharmacokinetic parameters are affected by age, caffeine intake, smoking, and oral contraceptives. Accelerated absorption and impaired elimination are observed in critically ill patients.
Elderly patients
Melatonin metabolism is known to slow down with age. At different doses of melatonin, higher values of the area under the concentration-time curve (AUC) and Cmax were obtained in the elderly, which reflects a reduced metabolism of melatonin in this group of patients.
Patients with impaired renal function No accumulation of melatonin was observed during long-term treatment. These data are consistent with the short half-life of melatonin in humans.
Patients with liver dysfunction The liver is the main organ involved in the metabolism of melatonin, so liver diseases lead to increased concentrations of endogenous melatonin. In patients with liver cirrhosis, plasma melatonin concentrations increased significantly during the daytime.
Indications for use
For sleep disorders, incl. caused by a violation of ri, such as desynchronosis (sudden change of time zones).
Contraindications
Hypersensitivity to the components of the drug, autoimmune diseases, liver failure, severe renal failure, pregnancy, breastfeeding, children under 18 years of age.
CAREFULLY
The drug Melatonin-SZ should be used with caution in patients with varying degrees of renal failure.
USE IN PREGNANCY AND BREASTFEEDING
The drug is contraindicated for use during pregnancy and breastfeeding
Directions for use and doses
Inside. For sleep disturbances - 3 mg once a day 30-40 minutes before bedtime.
For desynchronosis, as an adaptogen when changing time zones - 1 day before the flight and in the next 2-5 days - 3 mg 30-40 minutes before bedtime. The maximum daily dose is 6 mg.
Elderly patients
With age, melatonin metabolism decreases, which must be taken into account when choosing a dosage regimen for elderly patients. Taking this into account, in elderly patients, it is possible to take the drug 60-90 minutes before bedtime.
Kidney failure
The effect of varying degrees of renal impairment on the pharmacokinetics of melatonin has not been studied, so melatonin should be taken with caution in such patients. The use of the drug is not recommended for patients with severe renal failure.
Side effect
Classification of the frequency of side effects according to the recommendations of the World Health Organization: very often (>1/10), often (>1/100 to <1/10), uncommon (>1/1000 to <1/100), rarely ( from >1/10000 to <1/1000), very rarely (<1/10000), including isolated reports; frequency unknown (it is not possible to determine the frequency of occurrence based on available data).
Infectious and parasitic diseases: rarely: herpes zoster.
Blood and lymphatic system disorders:
rarely: leukopenia, thrombocytopenia.
Immune system disorders: frequency unknown: hypersensitivity reactions. Metabolic and nutritional disorders: rarely: hypertriglyceridemia, hypokalemia, hyponatremia.
Mental disorders:
uncommon: irritability, nervousness, restlessness, insomnia, unusual dreams, nightmares, anxiety;
rarely: mood swings, aggression, agitation, tearfulness, symptoms of stress, disorientation, early morning awakening, increased libido, decreased mood, depression.
Nervous system disorders: uncommon: migraine, headache, lethargy, psychomotor hyperactivity, dizziness, drowsiness; rare: fainting, memory impairment, impaired concentration, delirium, restless legs syndrome, poor sleep quality, paresthesia.
Visual disturbances: rarely: decreased visual acuity, blurred vision, increased lacrimation.
Hearing and labyrinth disorders:
rarely: vertigo, positional vertigo.
Cardiovascular system disorders: uncommon: arterial hypertension; rarely: angina pectoris, palpitations, hot flashes.
Gastrointestinal disorders: uncommon: abdominal pain, abdominal pain in the upper abdomen, dyspepsia, ulcerative stomatitis, dry mouth, nausea;
rare: gastroesophageal disease, gastrointestinal disorder or disorder, bullous stomatitis, ulcerative glossitis, vomiting, increased peristalsis, bloating, hypersecretion of saliva, bad breath, abdominal discomfort, gastric dyskinesia, gastritis. Liver and biliary tract disorders: uncommon: hyperbilirubinemia.
Skin and subcutaneous tissue disorders: uncommon: dermatitis, night sweats, itching and generalized itching, rash, dry skin; rarely: eczema, erythema, hand dermatitis, psoriasis, generalized rash, itchy rash, nail damage; frequency unknown: Quincke's edema, swelling of the oral mucosa, swelling of the tongue.
Musculoskeletal and connective tissue disorders: uncommon: pain in the extremities;
rarely: arthritis, muscle spasms, neck pain, night cramps.
Renal and urinary tract disorders: uncommon: glucosuria, proteinuria; rarely: polyuria, hematuria, nocturia.
Disorders of the genital organs and breast:
uncommon: menopausal symptoms; rarely: priapism, prostatitis; frequency unknown: galactorrhea.
General disorders and disorders at the injection site: uncommon: asthenia, chest pain; rarely: fatigue, pain, thirst.
Laboratory and instrumental data: uncommon: abnormal laboratory parameters of liver function, weight gain; rarely: increased activity of “liver” transaminases, deviation from the norm in the content of electrolytes in the blood, deviation from the norm in the results of laboratory tests.
Overdose
According to available literature data, the use of melatonin in a daily dose of up to 300 mg did not cause clinically significant adverse reactions. Flushing, abdominal cramps, diarrhea, headache and scotoma have been observed when melatonin was used in doses of 3000 - 6600 mg for several weeks. When very high doses of melatonin (up to 1 g) were used, involuntary loss of consciousness was observed.
In case of overdose, drowsiness may develop. Treatment is gastric lavage and the use of activated carbon, symptomatic therapy.
Clearance of the active substance is expected within 12 hours after oral administration.
Interaction with other drugs
Pharmacokinetic interaction
• It is known that in concentrations significantly exceeding therapeutic levels, melatonin induces the CYP3A />7 isoenzyme in vitro. The clinical significance of this phenomenon is not fully understood. If signs of induction develop, consider reducing the dose of concomitantly used drugs.
• At concentrations significantly higher than therapeutic levels, melatonin does not induce CYP1A isoenzymes in vitro. Therefore, the interaction of melatonin with other drugs due to the effect of melatonin on CYP1A isoenzymes is apparently insignificant.
• Melatonin metabolism is mainly mediated by CYP1A isoenzymes. Therefore, it is possible that melatonin may interact with other drugs due to the effect of melatonin on isoenzymes of the CYP1A group.
• Caution should be exercised in patients taking fluvoxamine, which increases melatonin concentrations (17-fold increase in AUC and 12-fold increase in Cmax) due to inhibition of its metabolism by cytochrome P450 isoenzymes (CYP): CYP1A2 and CYP2C19. This combination should be avoided.
• Caution should be exercised in patients taking 5- and 8-methoxypsoralen, which increases melatonin concentrations due to inhibition of its metabolism.
• Caution should be exercised in patients taking cimetidine (an inhibitor of CYP2D isoenzymes) as it increases plasma melatonin levels by inhibiting the latter.
Smoking can reduce melatonin concentrations due to the induction of the CYP1A2 isoenzyme.
• Caution should be exercised in patients taking estrogens (eg, contraceptives or hormone replacement therapy), which increase melatonin concentrations by inhibiting their metabolism by CYP1A1 and CYP1A2.
• Inhibitors of CYPA2 isoenzymes, such as quinolones, can increase melatonin exposure.
• Inducers of the CYP1A2 isoenzyme, such as carbamazepine and rifampicin, can reduce the plasma concentration of melatonin.
• The current literature contains a wealth of data regarding the effects of adrenergic and opioid receptor agonists/antagonists, antidepressants, prostaglandin inhibitors, benzodiazepines, tryptophan and alcohol on the secretion of endogenous melatonin. There have been no studies of the mutual influence of these drugs on the dynamics or kinetics of melatonin. Pharmacodynamic interaction
• While taking melatonin, you should not drink alcohol, as it reduces the effectiveness of the drug.
• Melatonin potentiates the sedative effects of benzodiazepine and non-benzodiazepine hypnotics such as zaleplon, zolpidem and zopiclone. In a clinical study, clear evidence of a transient pharmacodynamic interaction between melatonin and zolpidem was observed one hour after administration. Combined use may lead to progressive impairment of attention, memory and coordination compared to zolpidem monotherapy.
• In studies, melatonin was given together with thioridazine and imipramine, drugs that affect the central nervous system. In none of the cases was there a clinically significant pharmacokinetic interaction. However, concomitant use with melatonin resulted in increased feelings of calmness and difficulty performing certain tasks compared with imipramine monotherapy, as well as increased feelings of brain fog compared with thioridazine monotherapy.
special instructions
During the period of use of the drug Melatonin-SZ, it is recommended to avoid exposure to bright light.
It is necessary to inform women who want to become pregnant that the drug has a weak contraceptive effect.
There are no clinical data on the use of melatonin in patients with autoimmune diseases, and therefore, use in this category of patients is not recommended.
Impact on the ability to drive vehicles and operate machinery
The drug Melatonin-SZ causes drowsiness; therefore, during the treatment period, you should refrain from driving vehicles and engaging in potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Release form
Film-coated tablets, 3 mg.
10 or 30 tablets per blister pack. 30 tablets in polymer jars made of low-density polyethylene with a lid made of high-density polyethylene or in polymer bottles made of low-density polyethylene with a lid made of high-density polyethylene. Each jar, bottle, 1, 2, 3 blister packs of 10 tablets or 1, 2 blister packs of 30 tablets, together with instructions for use, are placed in a cardboard box.
Best before date
3 years. Do not use after the expiration date stated on the packaging.
Storage conditions
In a place protected from light, at a temperature no higher
25 °C.
Keep out of the reach of children.
Vacation conditions
Dispensed without a prescription
Prescription drug
Over-the-counter drug
Website
melatonin-sz.ru
The use of synthetic melatonin analogues in medicine
Most often, melatonin preparations are used to treat various sleep disorders.
Conducted studies prove the effectiveness of melatonin for acute insomnia: the time to fall asleep decreases, the quality of night sleep and its duration improve. Taking melatonin is justified in case of chronobiological disorders, when a person often changes time zones or works on a shift schedule alternating night and day shifts.
“Sleep hormone” drugs cannot be used as a usual sleeping pill. They help only with failures caused by a decrease in melatonin production. In other cases there will be no effect.
Melatonin is not prescribed for:
- chronic insomnia;
- maintaining the daily secretion of your own melatonin;
- normal biological rhythms.
Where is melatonin?
Melatonin is produced in the body. Melatonin is also found in some foods and can be synthesized artificially from animal pineal hormone. Nowadays you can find many melatonin preparations in pharmacies in the form of medicines or nutritional supplements, so let’s figure out together who needs to take melatonin and how safe it is.
There are several indications for taking melatonin:
- Delayed sleep phase syndrome (DSPS or night owl syndrome) is a rare pathology when a person’s biorhythms are disrupted, such people cannot sleep and get up late. Research shows that taking melatonin by mouth shortens the time it takes to fall asleep and speeds up sleep onset in people with this condition. However, a year after stopping therapy, the problem may return.
- Insomnia. According to studies, short-term use of melatonin reduces the time to fall asleep for insomnia by about 7-12 minutes. Melatonin has been shown to improve sleep and sleep problems in comorbid conditions such as depression, schizophrenia, epilepsy, autism, and various cognitive impairments. Melatonin may reduce evening confusion and restlessness in people with Alzheimer's disease, Parkinson's disease, dementia, and traumatic brain injury, but does not improve cognitive performance.
- Insomnia caused by beta blockers. Sleep disturbance caused by certain blood pressure medications can be regulated with melatonin. Melatonin has been shown to slightly shorten the time it takes to fall asleep, but its effect on sleep quality and overall sleep time is unclear. Melatonin may also be beneficial for older adults who have a physiological melatonin deficiency.
- Disorder of daily biorhythms due to long-distance flight. Most studies show that melatonin can improve certain symptoms of jet lag, such as daytime sleepiness and fatigue. It also helps you quickly adapt to a new time zone.
- Migraine. According to many domestic and foreign studies, melatonin helps prevent migraines in adults and children, and the attacks that occur pass away faster.
- Shift work. It has not been fully proven whether melatonin can improve the quality and duration of daytime sleep in people who work at night.
- Circadian rhythm disturbances in blind people. Melatonin helps regulate biorhythms in blind people.
- Sleep disorders in children. Small studies have shown that melatonin may help treat sleep problems in children with various forms of developmental delays. However, developing a daily routine and healthy bedtime habits is usually recommended as a starting point.
Is it safe to take melatonin?
Although melatonin is not as effective as some sleeping pills, it has fewer side effects than other medications. In rare cases, it causes headaches, dizziness, mild anxiety, and decreased concentration.
Since melatonin has a certain sedative effect, for the first 5-6 hours after taking it you should refrain from driving and working with technically dangerous mechanisms.
Although melatonin is a fairly safe substance, the decision to take it should be discussed with your doctor. The doctor will determine the indications and contraindications, help you choose the dosage if he thinks that you need to take melatonin and determine the duration of the course of treatment. As a rule, after stopping taking melatonin, sleep disturbances return, since taking the hormone does not help to regulate its production by the body, but is only a temporary measure. Therefore, in addition to prescribing melatonin, the doctor will give recommendations on how to eliminate the causes of disturbed sleep, how to restore the disrupted mechanisms of falling asleep and maintaining normal sleep.
Dietary supplement or medicine?
There is still no consensus among doctors whether to consider melatonin a medicine or a biologically active supplement (dietary supplement).
IN THE USA
The Food and Drug Administration (FDA) has not approved it for medical use, so melatonin is sold over-the-counter as a dietary supplement.
In the European Union and Australia,
melatonin is considered a medicine, sold by prescription and used to treat insomnia in children, adolescents and people over 55 years of age.
In Russia
Dosage forms of the drug and dietary supplements have been registered and can be purchased in pharmacies and sports nutrition stores without a prescription.
Melatonin is used as an adjuvant therapy for:
- peptic ulcer of the stomach and duodenum;
- hypertension;
- Alzheimer's disease and other memory disorders;
- depression and other diseases.
Research into the pharmacological activity and effectiveness of melatonin is ongoing. To date, more than 26 thousand scientific papers have been published, each of which opens up new pages in the use of this amazing substance.
In what form and how to take melatonin
Melatonin comes in two formats: regular and extended-release. The regular one dissolves as soon as you take the pill and instantly enters the bloodstream. After just four hours, it is almost 90% processed by the body. Long-acting additives dissolve more slowly. Their action is more reminiscent of natural melatonin, which is produced in the body gradually during the night.
If the problem is one-time (jet lag caused by flying across several time zones, for example), a regular supplement will do. In other cases, it is better to take long-acting melatonin. And not a supplement, but a medicinal product that has passed quality control and examination. This gives more confidence that its composition and dosage are truly as the manufacturer claims. But before buying, you will need to go to the doctor: melatonin medicine is not sold freely, but by prescription.
Immediate-release melatonin is taken 30 minutes before bedtime, and long-acting melatonin is taken 1-2 hours before bedtime. With dosage, everything is not so simple: studies test different options, since the effect depends on the type of problem and the individual characteristics of a person’s metabolism. One study found that melatonin levels in the blood plasma of healthy young adults taking a 0.1-0.3 mg supplement reached natural levels. But a dose higher than 1 mg per day can already increase the concentration of melatonin so that it exceeds the physiological one.
The recommended dose of the supplement, regardless of the purpose for which you take it, is no more than 3 mg per day: if you take more, you are likely to experience daytime drowsiness and other side effects. If your sleep pattern is only slightly disrupted due to jet lag or short-term insomnia occurs, you can start taking a dosage of 0.1 mg and gradually increase to 1 mg until sleep returns to normal. And in the case of chronic insomnia, where a low dose may not work, it is better to consult a doctor and discuss with him whether it is worth trying melatonin or looking for another solution.
Reminder has a free video course “Healthy Sleep for Professionals”
: 11 lessons that will give you a theoretical basis, learn about sleep management techniques from the arsenal of cognitive behavioral therapy for insomnia, and also master several basic meditation techniques that will help you relax. We recommend starting the fight for sleep with it.
Melatonin and COVID-19
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has forced scientists to actively study the effect of melatonin on the course of this disease. As a result, the usual “sleep regulator” began to be used in a complex of means of auxiliary therapy for COVID-19. In the fall of 2020, it was even used to treat US President Donald Trump. US
Melatonin Reviews In October 2021, the electronic scientific library medRxiv published a report on a research work in which 800 cases of severe COVID-19 were studied. It turned out that patients who initially had high levels of their own melatonin, and those who received the hormone in the form of a drug, were significantly more likely to survive in intensive care. Melatonin increased the chances of recovery, both from coronavirus and any other infection that affects the lungs.
Canada and Argentina.
The work was published in the journal Diseases in November 2021. A joint study from the University of Toronto and the Pontifical Catholic University found that the disease may be more severe in older people due to decreased levels of melatonin. Melatonin in adequate doses prevents the development of an aggressive form of COVID-19, and also supports the effect of the anti-coronavirus vaccine.
Brazil.
Data published by Melatonin Research in early 2021. Scientists from the University of Sao Paulo have proven that melatonin, which is produced by the cells of the alveoli of the lungs, becomes a barrier to coronavirus. This may be why people with high levels of melatonin do not become infected with Covid or experience the disease easily. Regina Pekelman, the author of the study, is confident that using nasal drops or a spray with melatonin is an effective means of combating COVID-19.
To enter the human body, SARS-CoV-2 viruses must bind to angiotensin-converting enzyme 2 (ACE2) receptors located on the surface of lung cells. Only by combining with ACE2 do coronaviruses enter the cell and begin to multiply, leading to disease.
Melatonin reduces the number of free ACE2 receptors, as a result, the number of connections between the virus and the enzyme is reduced, which leads to damage to a minimum number of cells, which means the coronavirus infection will occur in a mild form.
Additionally, melatonin reduces the inflammatory response at the site of virus entry and controls the immune response, preventing the development of a “cytokine storm.” And since it is the violent cytokine reaction that leads to a fatal result, its suppression increases the patient’s chances of surviving and avoiding serious complications.
In our country
sufficient scientific experience has not yet been accumulated to confirm the fact that melatonin prevents severe COVID-19, and the mechanism of action of melatonin on the human body has not yet been sufficiently studied. However, empirical evidence provides encouraging results and supports the positive effect of melatonin on the outcome of COVID-19.
Melatonin preparations are available in Russia without a prescription, but you should not take them without an in-person consultation with a doctor, either to correct sleep disorders or to prevent or treat COVID-19.
Risks of Taking Melatonin
Melatonin is considered safe for short-term use - for example, to restore sleep patterns. Even taking single extreme doses is unlikely to cause harm. There is not yet enough data on long-term use to consider it completely safe, but there are few risks. Here are the ones worth keeping in mind.
- Melatonin has side effects.
Headache, dizziness, daytime sleepiness and nausea are rare but do occur. They may be an individual reaction or a consequence of too high a dosage (above 3 mg). Melatonin also inevitably causes drowsiness immediately after taking it, so it is best to avoid driving or operating machinery for five hours after taking the supplement.
- Melatonin may interfere with the way medications work.
The list of drugs that are best not taken with the supplement is quite long. Anticoagulants, antiplatelet drugs, and any supplements that reduce blood clotting when combined with melatonin increase the risk of bleeding. Antidepressants and hormonal contraceptives - cause excessive drowsiness and may worsen side effects. Diabetes medications may not work as well because melatonin reduces insulin sensitivity and production. Anticonvulsants and immunosuppressants also work worse. So if you take medications, you should consult your doctor before purchasing melatonin.
- The composition of the supplement does not always correspond to the label.
The production of dietary supplements is not as strictly regulated as drugs. As a result, they may not contain melatonin at all or may not contain the amount indicated on the package. In 2017, researchers tested 31 melatonin supplements and found that melatonin content was within 10% of label claims in more than 71% of the supplements. 26% of the supplements also contained serotonin, which, if exceeded, can lead to serotonin syndrome, a rare but dangerous toxic reaction.
- It is not so easy to choose the dosage.
The brain produces less than 0.1 g of melatonin per night. Melatonin supplements usually contain much more: 2–12 mg. This number seems excessive. Especially in the context of studies in which melatonin reduced insulin sensitivity and production.
Publications on the topic of the month “How to overcome post-Covid syndrome”
- Lung recovery after coronavirus
- Restoring the sense of smell after coronavirus
- Restoring memory after suffering from coronavirus
- Overcoming mental disorders during post-Covid syndrome
- We are experiencing COVID. How the coronavirus pandemic affects mental functioning
- Post-Covid screening - examination after a new coronavirus infection
- How to return digestion to normal after coronavirus?
- Loss of smell due to COVID-19 - advice from an otolaryngologist
- Recommendations from a cardiologist after suffering from COVID-19
- Coronavirus turned out to be “vindictive” - what is important to know
- Post-Covid syndrome: program for diagnosis and regression of post-Covid symptoms. How to Manage Long-Term Long COVID Symptoms