Epocrine
During treatment, it is necessary to monitor blood pressure weekly and perform a complete blood count (including platelets, hematocrit, ferritin). In the pre- and postoperative period, Hb should be monitored more often if the initial value was less than 140 g/l.
It must be remembered that the drug in the treatment of anemia does not replace blood transfusion, but reduces the need for its repeated use.
In patients with controlled arterial hypertension or a history of thrombotic complications, an increase in the dose of antihypertensive drugs and anticoagulants may be required, respectively.
When prescribed to patients with liver failure, a slowdown in drug metabolism and a pronounced increase in erythropoiesis are possible. The safety of the drug in this category of patients has not been established. Although the drug stimulates erythropoiesis, the possibility of the drug affecting the growth of certain types of tumors, incl. bone marrow.
The possibility that a preoperative increase in Hb may predispose to the development of thrombotic complications should be considered. Before undergoing elective surgery, patients should receive adequate prophylactic antiplatelet therapy. In the pre- and postoperative period, it is not recommended to prescribe it to patients with an initial Hb of more than 150 g/l. In adult patients with chronic renal failure and clinically significant ischemic heart disease or heart failure, Hb should not exceed 100-120 g/l.
Before starting treatment, possible causes of an inadequate reaction to the drug should be excluded (deficiency of Fe, folic acid, cyanocobalamin, severe Al3+ poisoning, concomitant infections, inflammatory processes and injuries, hidden bleeding, hemolysis, bone marrow fibrosis of various etiologies) and, if necessary, adjust the treatment. Before starting treatment, iron reserves in the body should be assessed. In most patients with chronic renal failure, in cancer and HIV-infected patients, the plasma ferritin concentration decreases simultaneously with an increase in hematocrit. Ferritin concentrations must be determined throughout the course of treatment. If it is less than 100 ng/ml, replacement therapy with oral Fe preparations is recommended at a rate of 200-300 mg/day (100-200 mg/day for children). Patients donating autologous blood and in the pre- or postoperative period should also receive an adequate amount of Fe orally at a dose of 200 mg/day.
In patients with chronic renal failure, correction of anemia may result in improved appetite and increased absorption of K+ and proteins. Periodic adjustments of dialysis parameters may be required to maintain BUN, creatinine, and K+ concentrations within normal limits. In patients with chronic renal failure, it is necessary to monitor serum electrolytes.
According to available data, the use of the drug in predialysis patients does not accelerate the progression of chronic renal failure. Due to increased hematocrit, it is often necessary to increase the dose of heparin during hemodialysis. With inadequate heparinization, blockage of the dialysis system and thrombosis of shunts are possible, especially in patients with a tendency to hypotension or with complications of an arteriovenous fistula (stenosis, aneurysm, etc.). In such patients, early revision of the shunt and timely prevention of thrombosis (for example, ASA) are recommended.
Experimental studies on rats and rabbits did not reveal a teratogenic effect when administered intravenously in doses up to 500 IU/kg body weight per day; at higher doses, a weak, statistically insignificant decrease in fertility was noted.
Chronic toxicity studies (in rats and dogs) revealed the development of subclinical fibrosis of bone marrow tissue. During the 13-week study, dogs treated subcutaneously or intravenously at doses of 80, 240, or 520 units/kg/day developed anemia without or with signs of bone marrow hypoplasia. Due to the fact that the drug is a human glycoprotein, it is recognized that these changes could be caused by the action of antibodies to the drug. Similar phenomena were observed in isolated cases when using the drug in veterinary practice and were explained by the appearance of antibodies to epoetin alfa. No carcinogenicity studies have been conducted. The drug does not cause gene mutations in bacteria (Ames test), chromosomal aberrations in mammalian cells, micronucleia in mice, or gene mutations in the HGRT locus.
During the treatment period, until the optimal maintenance dose is established for patients with chronic renal failure, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions (increased risk of increased blood pressure at the beginning of therapy).
Epocrine, 10 pcs., 1 ml, 10000 IU, solution for intravenous and subcutaneous administration
Before and after starting therapy with Epocrine®, blood pressure must be adequately monitored. Epokrin® should be used with caution in the presence of untreated or poorly controlled hypertension. During therapy with Epocrine®, antihypertensive therapy may be necessary. If it is impossible to reduce blood pressure with antihypertensive drugs, therapy with Epocrine® should be discontinued.
A hypertensive crisis accompanied by encephalopathy and seizures, requiring immediate medical intervention, can also occur during therapy with Epocrine in patients who previously had normal or low blood pressure. Particular attention should be paid to sudden shooting migraine-like headaches as a possible signal of the onset of a crisis (see Side effects).
Epoetin alfa should also be used with caution in patients with chronic liver failure. The safety of epoetin alfa in patients with hepatic impairment has not been established. Due to reduced metabolism in patients with impaired liver function, increased erythropoiesis may occur when using epoetin alfa.
An increased incidence of thrombotic vascular events, such as venous and arterial thrombosis and embolism (including several fatal cases), such as deep vein thrombosis, pulmonary embolism, retinal thrombosis and myocardial infarction, has been observed in patients receiving erythropoietin-stimulating drugs. In addition, cerebrovascular accidents (including cerebral infarction, intracerebral hemorrhage and transient ischemic attacks) have been observed. The reported risk of thrombotic vascular events should be carefully weighed against the benefit of treatment with epoetin alfa, particularly in patients with risk factors.
Hemoglobin levels should be closely monitored in all patients due to the potential increased risk of thromboembolic events and deaths observed in patients with elevated hemoglobin levels when treated with Epocrine.
The safety and effectiveness of epoetin alfa therapy in patients with underlying hematological diseases, such as hemolytic anemia, sickle cell anemia, thalassemia, have not been studied.
When treated with Epokrin®, regular monitoring of platelet levels is required, especially during the first 8 weeks, since a dose-dependent relative increase in platelet count may develop, which will normalize further without discontinuation of therapy; in rare cases, there is an absolute increase in the platelet count.
Other causes of anemia (iron, folic acid or vitamin B12 deficiency, aluminum toxicity, infection or inflammation, blood loss, hemolysis and bone marrow fibrosis of any origin) should be assessed and treated before initiating epoetin alfa therapy or when deciding to increase the dose. . In most cases, serum ferritin levels decrease simultaneously with an increase in hematocrit. To achieve an optimal response to epoetin alfa, adequate iron stores should be ensured, with supplemental iron supplementation if necessary:
- In patients with chronic renal failure, supplemental iron supplementation (elemental iron 200–300 mg/day orally in adults and 100–200 mg/day orally in children) is recommended if serum ferritin levels are below 100 ng/mL.
- Patients with cancer are recommended to take additional iron supplements (elemental iron 200-300 mg/day orally) if transferrin saturation is less than 20%.
- For patients in the autologous blood collection program, iron supplementation (elemental iron 200 mg/day orally) is recommended for several weeks before the start of autologous blood collection in order to achieve large iron stores before starting epoetin alfa therapy and throughout the course of epoetin alfa therapy. .
- For patients scheduled for major elective orthopedic surgery, supplemental iron supplementation (elemental iron 200 mg/day orally) is recommended throughout the course of epoetin alfa therapy. If possible, the use of iron supplements should be started prior to initiation of epoetin alfa therapy to ensure adequate iron stores are established.
Very rarely, exacerbations of porphyria were observed early in treatment in patients treated with epoetin alfa. Epoetin alfa should be used with caution in patients with porphyria.
Erythropoiesis-stimulating agents are not necessarily equivalent. Therefore, patients should be transferred from one erythropoiesis-stimulating drug (such as Epocrine®) to another only with the approval of the treating physician.
In patients with chronic renal failure treated with subcutaneous epoetin, antibody-mediated true erythrocyte aplasia (IEA) was very rarely observed after months and years of treatment.
Rare cases of this disease have also been reported in patients with hepatitis C treated with interferon and ribavirin when erythropoietin-stimulating drugs were concomitantly treated, so they are not approved for the treatment of anemia associated with hepatitis C.
In patients with chronic renal failure who experience a sudden decline in response, as measured by a decrease in hemoglobin (1-2 g/dL per month) with an increase in transfusion requirements, a reticulocyte count should be performed and assessed for typical causes of non-response (eg, deficiency of iron, folic acid or vitamin B12, aluminum toxicity, infection or inflammation, blood loss, hemolysis and bone marrow fibrosis of any origin). If the anemia-corrected reticulocyte count (i.e., reticulocyte “index”) is low (<20,000/mm3 or <20,000/μl or <0.5%) and the platelet and white blood cell counts are normal, and if no other reasons for the decreased effect, the level of antibodies to erythropoietin should be determined, and the possibility of a bone marrow examination should be considered to diagnose IEA.
If anti-erythropoietin antibody-mediated IEA is suspected, epoetin alfa therapy should be discontinued immediately. Treatment with any other erythropoietin-stimulating drugs should not be initiated as there is a risk of cross-reaction. If indicated, patients may be given appropriate therapy, such as blood transfusions.
Patients with chronic renal failure during treatment with Epocrine® should regularly measure hemoglobin levels until the hemoglobin level reaches stable values, with periodic monitoring thereafter.
To reduce the risk of hypertension, the rate of increase in hemoglobin levels should be approximately 10 g/l (maximum 20 g/l) per month. The dose should be reduced when the hemoglobin level reaches 120 g/l.
In patients with chronic renal failure, the maintained hemoglobin level should not exceed the upper limit of the specified hemoglobin level range. A hemoglobin level of 130 g/L or higher may lead to an increased risk of cardiovascular events, including death.
Patients with chronic renal failure and inadequate hemoglobin response to erythropoietin-stimulating drug therapy may be at even greater risk for cardiovascular events and mortality than other patients.
Based on currently available information, use of epoetin alfa in patients prior to dialysis (end-stage renal disease) does not increase the rate of progression of renal disease.
Shunt thrombosis has occurred in hemodialysis patients, particularly in patients with a tendency to hypotension or with complications of arteriovenous fistulas (eg, stenoses, aneurysms, etc.). In these patients, early check of the shunt and prevention of thrombosis by administering, for example, acetylsalicylic acid are recommended.
In some cases, hyperkalemia was observed, although its cause-and-effect relationship with the use of the drug has not been established. Serum electrolytes should be monitored in patients with chronic renal failure. If serum potassium levels are elevated or worsening, then, in addition to appropriate treatment of hyperkalemia, discontinuation of epoetin alfa should be considered until serum potassium levels are adjusted.
Due to an increase in hematocrit during therapy with Epokrin®, patients on hemodialysis may require an increase in the dose of heparin, otherwise occlusion of the dialysis system is possible.
Some patients with chronic renal failure during treatment with Epocrine® experienced a resumption of menstruation. The possibility of pregnancy and the need for contraceptive measures should be discussed with the patient before starting therapy.
Erythropoiesis-stimulating agents are growth factors that primarily stimulate the formation of red blood cells. Erythropoietin receptors can be expressed on the surface of many tumor cells. As with other growth factors, there is concern that erythropoiesis-stimulating agents can stimulate tumor growth.
In view of the above, the decision to administer a recombinant erythropoietin drug should be made on the basis of a risk-benefit assessment involving the individual patient and should take into account the specific clinical situation. Factors that should be considered in this assessment include: tumor type and stage; severity of anemia; life expectancy; the setting in which the patient receives treatment; patient preferences.
In patients with cancer receiving chemotherapy, when assessing the suitability of epoetin alfa therapy (particularly in patients at risk of transfusion), the delay of 2-3 weeks between the administration of erythropoiesis-stimulating agents and the appearance of erythropoietin-stimulated red blood cells should be taken into account.
If an HIV-infected patient does not respond or responds insufficiently to epoetin alfa therapy, other possible causes of anemia, including iron deficiency, should be considered.
In patients associated with an autologous blood collection program and receiving additional treatment with epoetin alfa, all special warnings and special precautions should be taken into account, especially mandatory volume replacement.
Appropriate blood monitoring standards should always be followed pre- and postoperatively.
Patients scheduled for major elective orthopedic surgery should receive antithrombotic prophylaxis because thrombotic and vascular events may occur in surgical patients, particularly in patients with underlying cardiovascular disease. In addition, special precautions should be taken in patients with a predisposition to the development of thrombotic complications. Moreover, in patients with a baseline hemoglobin level >130 g/L (8.1 mmol/L), the possibility that treatment with epoetin alfa may be associated with an increased risk of postoperative thrombotic vascular events cannot be excluded. Therefore, in patients with a baseline hemoglobin level > 130 g/l (8.1 mmol/l), the use of epoetin alfa is not recommended.
Impact on the ability to drive vehicles and machinery
The effect on the ability to drive vehicles and moving machinery has not been studied. However, during the treatment period, until the optimal maintenance dose is established, patients with uremia should avoid engaging in potentially hazardous activities that require increased concentration and psychomotor speed due to the increased risk of increased blood pressure at the beginning of therapy.
Features of treatment
Epocrine is prescribed together with iron supplements. This could be Hemobalance or Ferum Lek. The latter is administered in combination with vitamin B12. However, such a scheme does not guarantee a 100% improvement in the blood count. Weekly monitoring of your cat's health is very important. Due to the fact that animals often develop antibodies to the drug, the hematocrit may initially increase and then begin to fall sharply. In this case, the positive effect can last two to three months, and then the indicators will begin to deteriorate.
Epocrine should not be abruptly discontinued. If a cat is diagnosed with chronic renal failure and iron-containing therapy does not lead to a positive result, injections of the drug for preventive purposes should be carried out once a week under the control of the level of reticulocytes, red blood cells and hemoglobin.
In veterinary practice, two treatment regimens have been developed:
- A course of 3-4 injections repeated after two months. This regimen is suitable for animals in which it is not possible to achieve a stable remission in raising hemoglobin levels.
- A course of Epocrine at a dosage of 100-150 units/kg (for 3-4 days), taking tests and raising the hematocrit to a level of 30-35. If the dynamics are positive, preventive administration of the drug once a week. After 20 days, repeat tests. If the indicators are normal (and the cat is diagnosed with chronic renal failure or cancer is detected), a maintenance dose of medication remains.
Epocrin®
Treatment of anemia in patients with chronic renal failure: Epocrine® is administered subcutaneously or intravenously.
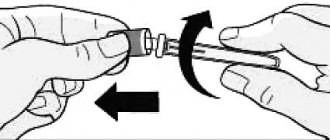
For hemodialysis patients, the drug is administered through an arteriovenous shunt at the end of the dialysis session. When changing the method of administration, the drug is administered at the same dose, then the dose is adjusted if necessary (with the subcutaneous route of administration of the drug Epocrine®, to achieve the same therapeutic effect, a dose of 20-30% less than with intravenous administration is required). Treatment with Epocrine® includes two stages:
1. Correction stage: When administering Epocrine® subcutaneously, the initial single dose is 30 IU/kg 3 times a week. When administering Epokrin® intravenously, the initial single dose is 50 IU/kg. The correction period lasts until the optimal level of hemoglobin (100-120 g/l in adults and 95-110 g/l in children) and hematocrit (30-35%) is achieved. These indicators must be monitored weekly. The following situations are possible:
1) Hematocrit increases from 0.5 to 1.0% per week. In this case, the dose is not changed until optimal values are achieved.
2) The rate of increase in hematocrit is less than 0.5% per week. In this case, it is necessary to increase the single dose by 1.5 times.
3) Growth rate of more than 1.0% per week. In this case, it is necessary to reduce the single dose of the drug by 1.5 times.
4) Hematocrit remains low or decreases. Necessary
analyze the causes of resistance.
The effectiveness of therapy depends on correctly selected
individual treatment plan.
2. Maintenance therapy stage: To maintain the hematocrit at a level of 30-35%, the dose of Epokrin® used at the correction stage should be reduced by 1.5 times. Then, the maintenance dose of the drug is selected individually, taking into account the dynamics of hematocrit and hemoglobin. After stabilization of hemodynamic parameters, it is possible to switch to the administration of the drug Epokrin® once every 1-2 weeks.
Prevention and treatment of anemia in patients with solid tumors: Before starting treatment, it is recommended to determine the level of endogenous erythropoietin. When the concentration of serum erythropoietin is less than 200 IU/ml, the initial dose of Epokrin® is 150 IU/kg for intravenous administration. When administered subcutaneously, the initial dose of Epocrine® can be reduced to 1000/kg. If there is no response, the dose may be increased to 300 IU/kg. Further increase in dose seems inappropriate. It is not recommended to prescribe erythropoietin to patients with serum endogenous erythropoietin levels above 200 IU/ml.
Prevention and treatment of anemia in patients with HIV infection: Intravenous administration of the drug Epocrine® at a dose of 100-150 IU/kg 3 times a week is effective in HIV patients receiving zidovudine therapy, provided that the level of the patient's serum endogenous erythropoietin is less than 500 IU /ml, and the dose of zidovudine is less than 4200 mg/week. When administered subcutaneously, the dose of Epocrine® can be reduced by 1.5 times.
Prevention and treatment of anemia in patients with multiple myeloma, low-grade non-Hodgkin lymphomas and chronic lymphocytic leukemia: In these patients, the advisability of treatment with epoetin alfa is determined by the inadequate synthesis of endogenous erythropoietin against the background of the development of anemia. When the hemoglobin content is below 100 g/l and serum erythropoietin is below 100 IU/ml, Epocrine® is administered subcutaneously at a starting dose of 100 g/kg three times a week. Laboratory monitoring of hemodynamic parameters is carried out weekly. If necessary, the dose of Epocrine is adjusted upward or downward every 3-4 weeks. If, upon reaching a weekly dose of 600 IU/kg, an increase in hemoglobin content is not observed, further use of the drug Epokrin® should be discontinued as ineffective.
Prevention and treatment of anemia in patients with rheumatoid arthritis: In patients with rheumatoid arthritis, suppression of the synthesis of endogenous erythropoietin is observed under the influence of increased concentrations of proinflammatory cytokines. Treatment of anemia in these patients is carried out with subcutaneous administration of the drug Epocrine® at a dose of 50-75 IU/kg 3 times a week. If the hemoglobin content increases by less than 10 g/l after 4 weeks of treatment, the dose of the drug is increased to 150-200 IU/kg 3 times a week. Further increase in dose seems inappropriate.
Treatment and prevention of anemia in premature infants born with low body weight: Epocrine® is administered subcutaneously at a dose of 200 IU/kg three times a week, starting from the 6th day of life until the target hemoglobin and hematocrit levels are achieved, but not more than 6 weeks.
Prevention of anemia during extensive surgery and acute blood loss: Epocrine® is administered intravenously or subcutaneously three times a week at a dose of 100-150 IU/kg until hematocrit and hemoglobin content normalize.
Dosage
The instructions for Epocrine do not contain data on use for cats, so the drug should be prescribed exclusively by a veterinarian after the cat has passed tests. The average dosage is 50-200 units/kg every 3-4 days. For example, if the active substance is in a concentration of 1000 IU, then a cat weighing 6 kg will receive one injection in a volume of 0.3 ml. On average, when hematocrit and hemoglobin are two times lower than normal, 150 units/kg is prescribed. It is necessary to make 3-4 injections and take tests again.
The medicine can only be stored and transported at low temperatures. An open ampoule is enough for 2-3 times, depending on the prescribed dosage. To prevent the medicine from spoiling, you can draw it into an insulin syringe and put it in the refrigerator.
Indications for use
Veterinarians have differing opinions regarding the appropriateness of Epocrine for cats. Some believe that this drug is able to enhance the production of red blood cells, others are against it, arguing that Epocrine is a recombinantly produced human erythropoietin, and in mammalian cells there is a gene that encodes it. According to statistics, the development of antibodies to this hormone occurs in 30% of cases of medication prescription. However, the remaining 70% of animals are successfully treated with it. Indications for its use are:
- Anemia in chronic renal failure, including hemodialysis.
- Toxic bone marrow depression as a result of decreased synthesis of endogenous erythropoietin in the kidneys.
- Hypovitaminosis B6 and B
- Dysfunction of iron absorption in the intestine.
- Anemia during tumor development.
Epocrine is not a panacea for anemia. To ensure the advisability of prescribing this drug, it is necessary to take a biochemical blood test. It is very important to know your iron levels. In the initial stages, you can try less drastic measures: giving iron supplements, vitamin B12 and folic acid. Epoetin alfa is used when the hematocrit drops below 19.
Reviews from veterinarians
Maxim Petrovich, veterinarian with 5 years of experience:
“I often prescribe Epocrine to treat cats. Despite the statistics (this drug is not suitable for every animal), it is difficult to find a replacement medicine. Thanks to him, I save the lives of my patients."
Margarita, veterinarian with 7 years of experience:
“To increase hemoglobin, I prescribe this drug to cats, the effect is usually noticeable after one course. In patients intolerant to epoetin alfa, I use darbepoetin; these drugs have a lower price and a gentle treatment regimen once a week.”