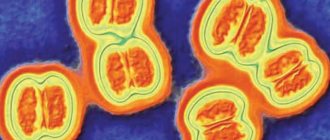
Another cause of purulent meningitis is meningococci. This is a large group of pathogens that cause more than 60% of meningitis in children and adults. They, in turn, are also divided into a number of groups - A, B, C, W135, Y, etc. The disease is transmitted by airborne droplets from person to person. The range of clinical manifestations of meningococcal infection is very wide. Just like with hemophilus influenzae, its source is not only a patient with meningococcal meningitis, but also carriers of this microorganism (there are about 5%, but carriage is mostly short-term, unlike hemophilus influenzae infection), as well as those who suffer from a mild form of infection , which looks like an acute respiratory illness.
Vaccine options
There are three types of vaccines available to combat this disease.
- Polysaccharide vaccines have been available to prevent meningococcal disease for more than 30 years. Meningococcal polysaccharide vaccines designed to combat the disease are bivalent (groups A and C), trivalent (groups A, C and W) or quadrivalent (groups A, C, Y and W135).
- It is impossible to develop polysaccharide vaccines against group B bacteria due to antigenic mimicry with polysaccharides in human neurological tissues. Therefore, group B vaccines, used in particular in Cuba, New Zealand and Norway, were outer membrane protein (OMP) and were intended to combat epidemics caused by specific strains. Other universal group B protein vaccines are in the final stages of development.
- Meningococcal group C conjugate vaccines have been available and widely used since 1999. Since 2005, quadrivalent group A, C, Y, and W135 conjugate vaccines have been licensed for use in children and adults in Europe, Canada, and the United States. The new group A meningococcal conjugate vaccine, introduced in 2010, has a number of advantages over existing polysaccharide vaccines: it produces a stronger and more durable immune response to group A meningococcus; reduces the carriage of bacteria in the throat. It is expected to provide long-lasting protection not only to vaccinated people, but also to family members and others who would otherwise be exposed to meningitis. The vaccine is available at a lower cost than other meningococcal vaccines; it is expected to be particularly effective in protecting children under two years of age who do not respond to conventional polysaccharide vaccines.
The following names of vaccines are used: polysaccharide - meningococcal group A vaccine, polysaccharide dry, polysaccharide meningococcal vaccine A+C, Meningo A+C, Mencevax ACWY and Menugate (conjugated tetravalent, against ACWY serotypes) and Menactra (conjugated tetravalent, against ACWY serotypes).
Vaccination is especially indicated for the following groups at high risk of meningococcal disease:
- persons who had direct contact with patients infected with meningococci of serogroups A, C, Y or W-135 (in the family or in closed institutions);
- persons with deficiency of properdin and complement components;
- persons with functional or anatomical asplenia;
- persons with cochlear implants;
- tourists and persons traveling to hyperendemic areas for meningococcal disease, such as sub-Saharan Africa;
- employees of research, industrial and clinical laboratories who are regularly exposed to N. meningitidis in aerosol-forming solutions;
- students of various universities, and especially those living in dormitories or apartment-type hotels;
- conscripts and new recruits.
It should be added that the European Commission has currently approved the drug Bexsero, produced by the Swiss pharmaceutical company Novartis, intended to protect patients of all age groups, including children over two months, from meningococcal infection serogroup B.
Who is at risk and how to prevent infection
Prevention of meningococcal infection can be nonspecific, it includes the following measures:
- isolation of identified carriers and sick people;
- preventing a recovered person from joining the team for 10 days after discharge;
- monitoring persons who have been in contact with sick people;
- teaching children basic hygiene rules;
- avoiding crowded places;
- increasing immunity by all available methods.
However, the most effective specific prevention is vaccination.
Meningococcal infection can affect anyone. The only exceptions are those who have been vaccinated.
However, doctors identify categories of people for whom the pathogen poses a particular danger. So, who should definitely get vaccinated against meningococcal infection:
- conscripts into the army (funds are allocated from the budgets of the regions sending guys to serve);
- travelers, especially to 26 meningitis belt countries: Benin, Burkina Faso, Burundi, Democratic Republic of the Congo, Gambia, Ghana, Guinea, Guinea-Bissau, Cameroon, Kenya, Ivory Coast, Mali, Mauritania, Niger, Nigeria , Rwanda, Senegal, Sudan, Tanzania, Togo, Uganda, Central African Republic, Chad, Eritrea, Ethiopia, South Sudan;
- pilgrims (since May 2001, vaccination with a quadrivalent (A+C+W135+Y) vaccine is mandatory for the Hajj to Saudi Arabia);
- persons with risk of contacts in outbreaks, i.e. according to epidemiological indications;
- children and teenagers before joining new groups (kindergarten, camp, school, boarding school, etc.) - paid for at the expense of CARING parents;
- medical workers.
Principles and purposes of vaccination
Meningococcal disease is potentially fatal and should always be treated as a medical emergency. Meningococcal meningitis occurs in small clusters worldwide, with seasonal variations and a varying percentage of epidemic bacterial meningitis cases.
Meningococcal meningitis is a bacterial form of meningitis, a serious infection that affects the lining of the brain. It can cause severe brain damage and, if left untreated, is fatal in 50% of cases. But even when diagnosed early and treated properly, up to 16% of patients die, usually within 24 to 48 hours of symptoms appearing.
It is important to remember that there are endemic areas of meningococcal infection in the world, the so-called meningitis belt of Africa (sub-Saharan Africa, stretching from Senegal in the west to Ethiopia and Egypt in the east). High incidence is observed in Canada, with outbreaks occurring in France and the USA. Students of closed educational institutions and colleges are especially vulnerable.
What complications may there be?
As mentioned above, if meningococcal infection is detected late, there is a high probability of death. However, even if treatment was prescribed on time, often the disease does not go away harmlessly. The consequences can lead to a variety of complications, ranging from hearing loss, vision and speech disorders, to amputation of limbs, paralysis, epilepsy and hydrocephalus. And here is another video (video by our partners - Sanofi Pasteur) with a girl who, at the age of 5, suffered a meningococcal infection and was left deaf for the rest of her life:
Vaccine effectiveness
Vaccination is carried out once, the effectiveness is about 90%, immunity is formed on average within 5 days and lasts 3-5 years. In December 2010, a new meningococcal group A conjugate vaccine was introduced throughout Burkina Faso and parts of Mali and Niger, where a total of 20 million people aged 1–29 years were vaccinated. Subsequently, in 2011, these countries reported the lowest ever number of confirmed cases of meningitis A during the epidemic season. Immunization with polysaccharide vaccines leads to a rapid rise in antibodies, which persist in children for at least 2 years, and in adults - up to 10 years; revaccination is carried out every 3 years. Conjugate vaccines maintain immunity for 10 years and develop immunological memory.
WHO recommends polysaccharide vaccines A and C for persons over 2 years of age from risk groups, as well as for mass vaccination during an epidemic - both for individual protection and to create collective immunity and reduce carriage. A type C conjugate vaccine has been created and used in Europe, which has led to a sharp decrease in the incidence of meningitis C; England, Holland and Spain have included this vaccine in their calendars.
The effectiveness of meningococcal vaccine was also assessed in post-registration studies. Thus, in the fight against an outbreak of meningococcal infection in the United States, 36 thousand people aged 2 to 29 years were vaccinated. As a result of the case-control study, 85% effectiveness was revealed, and among children from 2 to 5 years old it was 93%.
Meningococcus is not only in Africa
This infection is widespread throughout the world. And in Africa there is even a so-called “meningitis” or “meningococcal belt”:
However, this disease does not only exist somewhere far away, on other continents; unfortunately, it is also close to us. Outbreaks of meningococcal infection are recorded every now and then in different regions of Russia.
For example, in Novosibirsk in 2021, 25 cases of the disease were registered in less than two weeks. And this is very characteristic of this infection: usually long periods of well-being (10-15 years) are interrupted by sharp increases in incidence, which have a focal outbreak nature.
The increase in incidence can be explained by the widespread carriage of meningococcal bacteria. As the number of susceptible individuals increases, the number of cases increases. And declines are ensured by an increase in the immune layer as a result of latent immunization as bacterial carriage spreads among the population of a given territory.
You need to understand that during recession years the infection does not disappear: 50% of diseases occur in children under 5 years of age; 20% - for children aged 6-14 years. As age increases, incidence rates decrease, but carriage rates increase. The age group of 15-20 years is also subject to a high degree of susceptibility, because its representatives - students, military personnel - communicate intensively in schools, dormitories, barracks, etc. First of all, those who come from remote areas get sick, i.e. not previously in contact with the pathogen.
Why are doctors sometimes unable to identify meningococcal infection in the early stages of the disease and provide timely assistance? The fact is that the first symptoms of the disease are similar to the onset of a regular acute respiratory viral infection, and later medicine turns out to be powerless against the lightning-fast course of the disease. Moreover, during periods of prosperity, cases of the disease are so rare that the alertness of even experienced doctors, not to mention young novice doctors, gradually decreases.
One of the features that can also be canceled is that meningococcal infection is characterized by a winter-spring seasonality with the maximum number of diseases in February – April.
There are many real stories about how this can happen, here is one of them (a video from our partners - Sanofi Pasteur):
Post-vaccination reactions
Vaccines against meningococcal disease are well tolerated. In 25% of vaccinated people, a post-vaccination local reaction is possible in the form of soreness and redness of the skin at the injection site. Sometimes there is a slight increase in temperature, which normalizes after 24-36 hours. These vaccines are not required for routine immunization in our country, but you need to know about them, especially for those parents whose child is at high risk of developing meningococcal infection, or those who are planning a vacation in countries with unfavorable conditions for the spread of this infection.
How does meningococcal infection manifest?
Symptoms depend on the form of infection; When carried, the bacterium can only be detected using laboratory analysis, since there are no external signs. In other cases, symptoms may be as follows:
- acute nasopharyngitis – headache, runny nose or nasal congestion, weakness, increased body temperature;
- meningitis - a sharp increase in temperature, severe pain in the head, vomiting, pulling the legs towards the stomach, the inability to lower the neck and others characteristic of this disease;
- blood poisoning - a sharp increase in temperature, headache, confusion, muscle aches, rashes of varying sizes (most often on the lower part of the body);
- meningoenephalitis - symptoms similar to meningitis, various rashes on the skin and/or mucous membranes
A story from life! Muscovite Yana Savchenko’s 5-year-old daughter died of meningitis in January 2021. Mom and daughter were returning home by train. The girl’s temperature quickly rose to 41˚, her throat turned red, and her body took on the “coping dog” pose (with her legs pressed to her stomach). Upon arrival in Moscow, the child was immediately taken to the infectious diseases hospital, but after some time she died. Everything happened within 24 hours.
There is a test for mengococcal rash. You need to press the side of the glass against the rash-covered skin. It is important that you see the rash through the walls of the glass. If the rash is not visible when pressed, it is not meningococcal.
ATTENTION! Due to the high risk of serious complications and even death, at the slightest suspicion of meningococcal infection, you should immediately consult a doctor! Diagnosis is carried out by laboratory examination!
When to vaccinate?
Domestic vaccines - meningococcal A, A + C - are used from 18 months, and are also administered to adolescents and adults. These drugs can also be administered to children under 18 months of age if there is a sick person in the family or depending on the epidemic situation in the region. However, this measure does not create long-term, lasting immunity, and vaccination must be repeated after 18 months. Polysaccharide vaccines "Meningo A+C" and "Mencevax ACWY" are administered to children from 2 years of age. For vaccination of children over 9 months of age, the conjugate vaccine "Menactra" can be used, in this case it is prescribed twice with an interval of at least 3 months, and after 2 years is done once. The level of protective antibodies lasts up to 10 years.
Composition of vaccines
Currently, vaccines against meningococcus subgroups A, C, W135, Y, etc. are being produced in the world. The vaccine against meningococcus group B has been developed by a number of foreign companies, and is currently undergoing large-scale pre-licensing trials. Our country produces domestic vaccines MENINGOCOCCAL A and A + C; and also registered foreign analogues from various manufacturers: MENINGO A+S. All of these are polysaccharide vaccines, that is, those that contain polysaccharides1 of the cell wall of meningococcus, and not the entire microbe. These preparations do not contain preservatives or antibiotics.
Polysaccharides are the general name for carbohydrates; are structural elements of various tissues.
Symptoms of meningitis
Children and adolescents are more susceptible to developing pathology. The most common symptoms of meningitis are:
- stiffness and pain in the neck muscles, especially when tilting the head;
- hyperthermia;
- headache;
- nausea, vomiting;
- sleep cycle disturbance;
- irritability, tearfulness;
- A rash and cough may occur.
The nature of the inflammatory process in meningitis
Meningitis is classified according to several criteria. According to the nature of inflammation, they are purulent and serous.
Purulent
Pathogens: streptococci, staphylococci, pneumococci and others. Meningococcus enters the brain through the bloodstream. This is a dangerous type of disease, as the risk of death is high. When the first symptoms appear, urgent treatment with antibiotics is necessary. Features include the release of pus and the development of cell necrosis.
Serous
Occurs in epidemic outbreaks. The peculiarity is the release of serous exudate. It consists of a small number of leukocytes. How a secondary infection develops after influenza, mumps, and fungal diseases. The prognosis is favorable.