"I have seen cases
when a person felt good at breakfast,
and by lunchtime he was already dead!
Dr Clayton Golledge, microbiologist, infectious disease specialist, USA.
Meningococcal infection is an acute infectious disease caused by the bacterium Neisseria meningitidis. The severity of meningococcal infection ranges from nasopharyngitis to fulminant sepsis, leading to death within a few hours.
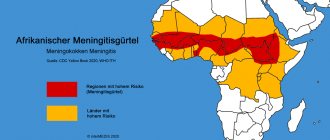
In Russia, the incidence averages 5 per 100 thousand population per year, which is a fairly high figure. The highest prevalence of meningococcal infection in the world occurs in Central Africa, China, and South America (the so-called “meningitis belt”), where large epidemics of this disease regularly occur. Outbreaks of infection occur mainly in conditions of unsanitary conditions and crowded populations.
Meningococcal infection is characterized by seasonality - the incidence is highest in winter and early spring, because The immune system during this period is weakened by the entry into the body of a large number of viruses, which are also activated at this time of year - ARVI, influenza, etc. In addition, hypothermia is an important trigger for the development of meningococcal infection.
The only carrier of the bacterium Neisseria meningitidis is humans.
The infection spreads through airborne droplets and through direct contact with a patient or carrier. The incubation period averages 3-4 days, but can vary from 2 to 10 days. In the fulminant form of the disease, symptoms develop within a few hours from the moment the meningococcal infection enters the body.
The most common target for menigococcal infection is children under 5 years of age. The immune system of children at this age is not fully formed; In addition, children tend to touch their mouths with unwashed hands and various objects; they still poorly observe the rules of general hygiene, such as covering their mouths when coughing and sneezing, and regularly washing their hands. In addition, the spread of infection is facilitated by preschool institutions, where children closely interact with each other while playing and eating.
The mildest form of the disease is meningococcal nasopharyngitis, which symptomatically occurs as an uncomplicated acute respiratory viral infection, and therefore is often not diagnosed. At this stage, the disease may end, after which the infection becomes asymptomatic carriage, which occurs in 8-25% of patients. However, bacteria often enter the bloodstream and cause meningococcemia (or meningococcal sepsis). In this case, bacteria rapidly multiply in the blood and cause disruption of the blood coagulation system, which leads to hemorrhages in the skin and internal organs, and often ends in death. Meningococcal sepsis can be complicated by meningitis. Meningitis is an inflammation of the meninges that cover the brain and spinal cord. Meningitis is not only meningococcal - other bacteria (pneumococcus, staphylococcus, Haemophilus influenzae type B) can cause inflammation, and viral and fungal forms of meningitis also occur. Meningococcal infection has an increased tendency to affect the meninges.
Manifestations of meningococcal infection are insidious and deceptive. The first symptoms are often nonspecific; making a correct diagnosis at the initial signs of the disease can be extremely difficult. However, when a detailed picture of the disease appears, the patient often cannot be saved. There are three forms of meningococcal infection, each of which can occur independently, or have a sequential development - from nasopharyngitis to bacteremia (sepsis) and meningitis.
***
About 1 in 10 people who contract meningitis die, and up to a quarter are left with lifelong complications, including amputations and deafness.
***
Symptoms characteristic of menigococcal nasopharyngitis (similar to the symptoms of ARVI):
- Increase in body temperature to febrile levels (on average up to 38-38.5ºС)
- Phenomena of rhinitis
- A sore throat
- Headache
- Pale skin
- General weakness.
Among the above symptoms, it is extremely important not to miss a sharp deterioration in the condition, which usually develops in the shortest possible time.
Symptoms characteristic of meningococcal meningitis (50%):
- Fever that does not respond well to antipyretics and headache (flu-like symptoms)
- Stiffness of the neck (neck) muscles
- Nausea, vomiting
- Photophobia
- Impaired consciousness, confusion and disorientation
- Cramps.
Symptoms characteristic of bacteremia (sepsis), including meningococcemia (37.5%):
- Fever
- Petechial and purpuric rash (usually begins on the lower extremities)
- Hypotension
- Shock
- Multiple organ failure
- Death can occur within the first 24 hours from the onset of the first symptoms.
About 10% of people with meningococcal infection die, and 20% experience disabling complications. The basis of effective treatment is early diagnosis of the disease; prevention also plays an important role, in particular, vaccination against meningococcal infection.
According to WHO recommendations, one of the recommended approaches to the prevention of meningococcal infection is primary mass vaccination of all children and adolescents aged 9 months to 18 years, followed by inclusion of the vaccine in the routine childhood immunization program. In countries with lower incidence (<2 cases/100 thousand people per year), vaccination against meningococcal disease is recommended only in certain risk groups:
- children and adolescents in closed institutions, i.e. boarding schools, military camps;
- bacteriology laboratory workers at high risk of exposure to meningococci;
- Travelers to highly endemic regions of the world should be vaccinated against serogroups common in those regions.
At Children's Medical, you can protect your child from a dangerous disease with Menactra.
Manufacturer: Sanofi Pasteur, France.
Compatibility with other vaccines
Menactra was administered concomitantly with a polysaccharide typhoid vaccine and with an adsorbed tetanus and diphtheria toxoid vaccine for use in adults (Td) in persons aged 18–55 years and 11–17 years, respectively. The BCG vaccine should not be used simultaneously with the Menactra vaccine. Vaccines must always be administered to different parts of the body, using separate syringes for each of them.
Administering several vaccines on the same day does not place an excessive burden on the immune system. All vaccines in the Russian national vaccination calendar are interchangeable.
special instructions
The vaccine drug Menactra is recommended for use especially by people from risk groups who have an increased likelihood of developing meningococcal infection:
- people in direct contact with infected people;
- confirmed deficiency of properdin, complement components;
- tourists and those people who are going to visit areas unfavorable for meningococcal infection, located mainly in Africa;
- congenital or acquired absence of the spleen;
- accommodation in hostels, apartment-type hotels;
- people who are planning to serve in the army or are already recruits.
It is prohibited to combine the vaccine drug Menactra with any other drugs in the same syringe. Also, you cannot use subcutaneous, intravenous or intradermal methods of administering the vaccine. The studies conducted did not involve the use of the drug in people who have bleeding disorders and thrombocytopenia.
The vaccine is not used as a prophylactic against meningitis, which can be caused by other microorganisms or meningococci serogroup B. There have been cases of Guillain-Barré syndrome, which can progress after administration of the vaccine. Therefore, people who have previously suffered from this condition may be at risk of recurrence in the future. The decision to use the vaccine drug Menactra should be made by a doctor after assessing the possible risks of developing Siillain-Barré syndrome.
Patients who suffer from immune disorders and are being treated with immunosuppressive therapy may have a reduced immune response after using the vaccine.
Menactra has not been studied to affect driving.
Personal application experience
At the Sanare clinic, patients (children) aged 9 months and older were vaccinated with Menactra. The vaccine was well tolerated. There were no complaints in the post-vaccination period. (All patients at the clinic were called and interviewed by a nurse the next day).
The first to be vaccinated with the drug "Menactra", after its arrival at the clinic, were pediatricians, clinic staff, as well as their children (aged from 2 to 11 years). The drug was also well tolerated.
Side effects
The activity of adverse reactions and their frequency depend on the age of the vaccinated patients. In children from the age group of 9-18 months, within a week after using the drug, pain was observed at the injection site with increased sensitivity of the skin in this area. Children from 2 to 10 years of age also had moderate pain and redness at the injection site of the vaccine. In this age group, symptoms such as drowsiness, decreased appetite, and irritability were noted.
Adolescents from 11 to 18 years of age and adults up to 55 years of age noted after vaccination the appearance of moderate pain at the injection site, as well as a tendency to headaches and increased fatigue.
Children from 9 to 18 months
Among the adverse reactions from this age group, there are mainly local manifestations in the form of redness of the skin, increased sensitivity during the first 2-3 days after using the vaccine, and the formation of erythema.
Common reactions include the following:
- drowsiness;
- irritability;
- cry;
- increase in body temperature.
Children 2-10 years old
Adverse reactions are mild and mildly expressed. In addition to local manifestations (swelling, rash, erythema, pain at the injection site), general manifestations may be observed:
- drowsiness;
- appetite disorders;
- nausea and vomiting;
- diarrhea;
- pain in muscles and joints;
- irritability.
People 11-55 years old
In patients from this age group, the most common adverse reactions were:
- swelling, redness, moderate soreness of the skin at the site of vaccine administration;
- headache;
- nausea and vomiting;
- decreased appetite;
- diarrhea;
- skin rash;
- joint pain;
- chills, malaise;
- increase in body temperature.
These occurrences occurred predominantly in the first 2-3 days after vaccine administration. But discomfort may persist a little longer - up to 5-7 days.
In the post-marketing period, some people associated the use of the vaccine drug Menactra with the following changes in the body, complaints and disorders:
- From the immune system: increased general sensitivity and irritability, problems with respiratory function, skin hyperemia, itching, decreased blood pressure.
- From the musculoskeletal system: muscle pain.
- From the side of the central nervous system: convulsions, dizziness, episodes of loss of consciousness, facial paralysis, Guillain-Barré syndrome (GBS), paresthesia, encephalomyelitis, transverse myelitis.
A study was conducted in the USA that assessed the risk of Guillain-Barré syndrome. Experts used data from patients aged 11-18 years. The total number of people whose health care information was reviewed was 9,578,688. Of these, 15% were vaccinated with Menactra. And none of those who received the vaccine had Guillain-Barré syndrome within 42 days of vaccination. Another 129 potential cases with this condition were not medically confirmed.
How is vaccination carried out?
Vaccination is carried out in a vaccination room, in compliance with all sanitary requirements. All drugs are certified. A certificate for the drug is provided upon request.
Without reminders, before vaccination, the medical worker must show the drug and the expiration date of the vaccine.
Only sterile and disposable instruments are used. The vaccination must be carried out using disposable medical gloves.
On the day of vaccination, the child is examined by a pediatrician and the temperature is measured. In the absence of contraindications, vaccination is carried out. Information about the vaccination performed is entered into the card, vaccination certificate, and detailed recommendations for caring for the child in the post-vaccination period are given.
Before vaccination, the doctor will answer all your questions. Be sure to bring information about previous vaccinations to your appointment!
Please note that vaccination of a child, Mantoux test, Diaskintest can only be carried out in the presence of parents or legal representatives of the child (guardians), or if the accompanying person has a NOTARIZED power of attorney to carry out the manipulation (indicating the drug planned for administration) . Otherwise, vaccination will be denied. We comply with the laws of the Russian Federation.
Only here!
Vaccination schedule with Menactra vaccine
from 9 to 23 months: 2 times with an interval of at least 3 months from 2 years to 55 years: once
The vaccine is administered intramuscularly into the deltoid muscle or the anterolateral surface of the thigh.
According to clinical studies, the tolerability of the vaccine is satisfactory. During the first 5-7 days after vaccination, the following vaccination reactions may occur:
- soreness and redness at the injection site
- temperature increase
Young children may also experience irritability, decreased appetite, and fatigue.
Storage at temperature +2 +8.
Contraindications
Only a doctor can decide whether Menactra is suitable for vaccination
The Menactra vaccine is contraindicated if there is a history of an allergic reaction to any component of the vaccine and in the following cases:
- A severe allergic reaction (eg, anaphylaxis) after a previous dose of meningococcal vaccine, diphtheria toxoid.
- Acute infectious and non-infectious diseases, exacerbation of chronic diseases (in these cases, vaccination is carried out after recovery or in remission).
What vaccines against meningococcal disease exist?
Meningococcus has many serotypes (subspecies) - more than 10, and there is no universal vaccine against them. The epidemic serogroups are considered the most dangerous: A, B, C, D, W-135 and Kh. V. S. Kovalev in the same interview notes an increase in the incidence of the W-135 group, affecting not only children, but also young adults in crowded groups (institutes, hostels, in the army), where the infection rate is, for obvious reasons, higher.
There are only three vaccines in the world that protect against meningococci: Nimenrix, Menactra and Bexero. At the same time, only Bexsero protects against serotype B, which accounts for up to 25% of all cases of meningococcal infection, and it is not certified in Russia. Doctors strongly recommend that parents vacationing with children in Europe vaccinate their children there.
But, in addition to serotype B, there are also vaccinations against equally dangerous serotypes A, C, Y and W-135. The most famous of them is the American Menactra. Fortunately, it is available in Russia - although they are not included in the National Calendar due to their high cost. Vaccination with Menactra in public clinics is possible only in emergency cases, for example, after contact with a patient. In other countries, for example, in the UK, Germany, Holland and the USA, this vaccine is on the National Calendar.
Let's summarize and return to the issue of vaccine compatibility
All vaccines can be divided into 2 large blocks: live and inactivated
(non-living).
Alive
include living but weakened microorganisms (bacteria and viruses).
Non-living
contain killed whole microorganisms or their artificially created parts.
The following variants are registered in Russia:
NON-LIVE VACCINES against the following infections:
- Viral Hepatitis B (Regevac, Recombinant yeast vaccine, Combiotech)
- Viral Hepatitis A (Havrix, Avaxim, Algavac)
- Poliomyelitis IPV (Polimilex, Poliorix, Imovax Polio, as part of complex vaccines)
- Flu (Influvac, Vaxigrip, Ultrix, Influenza, Sovigrip).
- Tick-borne encephalitis (Encevir, FSME-immune, Klesh-E-Vac, Encepur)
- Human Papilloma Virus (Gardasil, Cervarix)
- Whooping cough, diphtheria, tetanus (as part of complex vaccines: DTP, Bubo-Kokk, Bubo-M, Pentaxim, Tetraxim, Infanrix, Adasel)
- Haemophilus influenzae infection type b (Act-hib, Hiberix, as part of complex vaccines)
- Pneumococcus (Prevenar 13, Synflorix, Pneumo 23, Pneumovax 23)
- Meningococcus (Menactra, Menveo, Mencevax and others)
and LIVE VACCINES:
- Tuberculosis vaccine (BCG, BCG-M)
- Measles vaccine (monovaccine without brand name)
- Rubella vaccine (monovaccine without brand name)
- Mumps vaccine (monovaccine without brand name)
- Measles+Mumps (divaccine without brand name)
- Vaccine against measles, rubella, mumps (Priorix, MMR-II)
- Oral Polio Vaccine (Bivak polio)
- Oral vaccine against Rotavirus (Rotatek)
- Chickenpox vaccine (Varilrix)
How to diagnose meningococcal infection?
With a mild form of the disease, it can be quite difficult to distinguish it from ARVI. That is why it is important to consult a doctor in a timely manner in case of even a not very serious (in your opinion) ailment! Nasopharyngitis may develop into a more severe form in a few days, and precious time will be lost.
In the case of fulminant development of meningococcemia, the main symptoms are a sharp rise in temperature and a rash. Contact an ambulance immediately, this is critically important to do as soon as possible!
How great is the risk of getting sick?
Approximately 10-20% of people are carriers of meningoccal infection. Not all of them are sick - the carrier himself may be healthy. The bacteria live in the nasopharynx and are transmitted by airborne droplets. The sick person is contagious for about 3 weeks, of which 1 week is the incubation period, when the disease does not manifest itself in any way. You cannot get infected from animals or objects.
“We are riding the wave of a rise in meningococcal meningitis.”
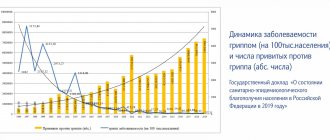
The infectiousness of this infection is quite low. However, the incidence of meningococcal disease has a wave-like nature, and 2021 appears to have seen a surge in incidence. For example, V.S. Kovalev, a pediatrician at the Children's Research and Clinical Center for Infectious Diseases of the FMBA in St. Petersburg, in an interview given in February 2021 to the website miloserdie.ru, notes that such rises occur approximately once every 20-25 years, and now Russia is on the rise.
“A large number of people in Russia have already fallen ill with meningitis”
The Business Information Agency of Khakassia cites data from Rospotrebnadzor, according to which the epidemiological threshold for meningococcal infection was exceeded back in March 2021:
According to Rospotrebnadzor, in the first six months of this year, 549 Russian residents fell ill with meningococcal infection. This is 23% more than in the same period last year.
What is meningococcal infection?
Meningococci are the bacteria Neisseria meningitidis that cause meningococcal disease. Contrary to popular belief, meningococcal disease is not the same as meningitis, although both are extremely dangerous diseases. Meningitis, or inflammation of the meninges, can be caused by meningococci, pneumococci, or even Haemophilus influenzae. Unfortunately, it is meningococcal meningitis that causes the greatest number of deaths. In the so-called “meningitis belt” of West Africa, it accounts for 80% of all meningitis cases.
But meningococcal infection does not necessarily manifest itself as inflammation of the meninges. Bacteria can cause mild forms of infection, for example, nasopharyngitis (this is a standard sore throat and stuffy nose, as with ARVI), and very severe ones, for example, meningococcemia (sepsis, that is, blood poisoning). It happens that the disease develops at lightning speed and cannot be stopped. It is most dangerous for children.