Paroxetine (Paxil) for anxiety disorders
Chakhava V.O.
Anxiety disorders (AD) develop in 25% of the population. They are often combined with each other and are comorbid with depression and various somatic diseases. TRs with comorbid conditions are usually less responsive to treatment and have a less favorable prognosis. Dysfunction of the serotonergic system has been found to play a significant role in the pathogenesis of TR, which puts forward antidepressants of the selective serotonin reuptake inhibitor (SSRI) class as first-line treatment in most cases of TR. The effectiveness of paroxetine, a representative of the SSRI, for TR is confirmed by the results of numerous randomized studies.
The results of epidemiological studies indicate that anxiety disorders are among the most common forms of mental pathology, occurring throughout life in approximately 25% of the population [1]. Despite the relatively shallow level of mental disorders, TD can significantly impair not only the subjective quality of life, but also social adaptation, as well as performance.
The main types of TD include panic disorder (PD), generalized anxiety disorder (GAD), social phobia (SSP), post-traumatic stress disorder (PTSD) and obsessive-compulsive disorder (OCD). It is important to note that when isolated, each of these conditions is less common than when accompanied by one or more other anxiety spectrum disorders. The frequency of combination of TD with depression, bipolar affective disorder, alcoholism, drug addiction and substance abuse is also high. Comorbid mental disorders worsen the prognosis of TR and complicate their treatment.
TR occurs in 30-40% of patients visiting general practitioners. In these patients, the symptoms of pathological anxiety include massive vegetative manifestations, masking the actual psychopathological symptoms. The hypochondriacal nature of many such patients prompts them to undergo multiple repeated examinations by internists, postponing the diagnosis and initiation of treatment for TR for a long time (sometimes for years).
It should also be noted that TR is often combined not only with other mental disorders, but also with somatic diseases, such as duodenal ulcer, coronary heart disease, arterial hypertension, rheumatoid arthritis, bronchial asthma [2]. According to epidemiological studies, in patients with TR these somatic diseases are detected much more often than in the general population.
As a result of numerous studies, it has been established that the serotonergic system plays a decisive role in the pathogenesis of anxiety disorders [3]. It has been shown that antidepressants that suppress the reuptake of serotonin by presynaptic neurons of the central nervous system are effective in the treatment of not only depression, but also TR.
Significant progress in pharmacological research in the 1980s was marked by the development of selective serotonergic agents (SSRIs) used in modern clinical practice. Their main advantage over the so-called “classical” or “traditional” tricyclic antidepressants (“dirty drugs”) is the reduction of side effects due to the selective mechanism of action.
As a rule, anxiety disorders require long-term therapy and satisfactory patient compliance, since premature cessation of treatment often leads to exacerbation [3,4]. One of the most common reasons for premature discontinuation of therapy is the development of unwanted side effects. The favorable tolerability profile of SSRIs due to the high degree of selectivity of their action contributes to good tolerability and, as a result, significantly greater adherence of patients to treatment.
Paroxetine (Paxil), one of the highest-potency SSRIs, was synthesized by GlaxoSmithKline and has been used since 1992. Paroxetine is a phenipiperidine derivative and is chemically distinct from both tricyclic and tetracyclic antidepressants.
The mechanism of action of paroxetine consists of a powerful inhibition of serotonin reuptake by presynaptic receptors, desensitization of serotonin receptors, an increase in direct neurotransmission of serotonin in the intersynaptic cleft, weak inhibition of norepinephrine reuptake, as well as a mild anticholinergic effect.
The accumulated experience of clinical use of the drug confirms its high effectiveness and good tolerability in various anxiety disorders. This publication reviews the most important results from clinical trials of paroxetine in TR.
Panic disorder (PD)
The main manifestation of PR is panic attacks - attacks of sudden, extremely intense fear that arises and grows within a few minutes, accompanied by a complex of autonomic disorders (vegetative crisis - palpitations, a feeling of suffocation, sweating, dizziness). During a panic attack, patients fear sudden death, loss of consciousness, or insanity (loss of self-control). The panic attack lasts for 2-10 minutes. The frequency of panic attacks in PD varies widely: from several per day to single ones throughout the year. In some patients, PD is complicated by agoraphobia - fear and avoidance of situations with which the patient associates the occurrence of panic attacks and in which they may find themselves in a helpless position. Most often it manifests itself as a fear of riding in public transport, stuffy rooms, crowds.
According to international publications, the lifetime prevalence of panic disorder is 2-3% [12]. PD usually manifests itself between the ages of 20 and 30. In women, panic disorder develops 2-3 times more often [5].
SSRIs, particularly paroxetine, are the first choice drugs for the treatment of PD (with or without agoraphobia).
In a 12-week study of 120 patients, Ohrenberg et al. showed a significant superiority of paroxetine over placebo (p<0.05) in effectiveness, assessed by reducing the number of panic attacks [6] over 6 weeks. Paroxetine was used in a dose of 40-60 mg.
These data are confirmed by the results of a double-blind study in a larger sample (n=278), which used fixed doses of paroxetine (10, 20 and 40 mg). The most pronounced improvement was observed when paroxetine was administered at a dose of 40 mg per day, at which (and not at 10 or 20 mg) a significant superiority over placebo was revealed [7].
A 12-week, placebo-controlled, multicenter study of 367 patients with PR compared paroxetine with clomipramine and placebo. Paroxetine was ahead of clomipramine in the time of realization of the therapeutic effect: at the 9th week of treatment, the proportion of patients with complete reduction of panic attacks was significantly greater in the paroxetine group (51%) than in the clomipramine (37%) and placebo (32%) groups [7, 8]. The differences in the effectiveness of the two antidepressants disappeared only after 12 weeks of therapy. Both drugs provided a significant reduction in anxiety, agoraphobia, as well as significant improvement in indicators of work ability, social functioning and family life. However, paroxetine caused significantly fewer side effects than clomipramine.
In the prospective 9-month phase of this study, which included 176 patients with panic disorder, the proportion of patients with complete reduction of panic attacks in the paroxetine group increased to 85%, in the clomipramine group - 72%, and placebo - 59%. The significant advantage of paroxetine over placebo in this indicator remained throughout the study [9,10].
The recommended daily dose of paroxetine for panic disorder is 30-40 mg, the maximum is 60 mg/day. [eleven]. The same doses are recommended for maintenance therapy for at least 6 months after complete reduction of symptoms [11].
Generalized anxiety disorder (GAD)
The lifetime prevalence of generalized anxiety disorder is 4–6.6%. The main symptoms of GAD are anxiety and restlessness not related to specific environmental circumstances. Anxiety is provoked and intensified in connection with various, often unimportant reasons. Important symptoms of GAD include muscle tension, a feeling of stiffness, an inability to relax, and signs of autonomic hyperactivity. Most often, GAD manifests itself at the age of 18-30, usually acquires a chronic wave-like course and lasts 10 years or more.
Along with antidepressants, tranquilizers are treatments for GAD. Their use, however, is limited to short courses due to the possibility of developing tolerance and subsequent drug dependence. It is believed that this probability is less than in the treatment of PR, but it must also be taken into account. In addition, it is known that patients with GAD often subsequently develop depressive states, and treatment of GAD with antidepressants, unlike the use of tranquilizers, is simultaneously preventive against depression.
The effectiveness of paroxetine in GAD was first demonstrated by Rocca et al. (1997)[12]. In an open-label, randomized study lasting 8 weeks, the authors compared 3 drugs for GAD: paroxetine, imipramine and chlordiazepoxide. The dose of paroxetine was 20 mg, imipramine - 50-100 mg, chlordiazepoxide - 3-6 mg. The study showed that in the first 2 weeks the benzodiazepine tranquilizer chlordiazepoxide had an advantage over antidepressants in reducing anxiety, but from the 4th week antidepressants (paroxetine and imipramine) were more effective. It turned out that antidepressants had a greater effect on mental symptoms of anxiety, while the tranquilizer mainly had an effect only on somatic signs of anxiety. As expected, imipramine was significantly less well tolerated than paroxetine due to anticholinergic effects (dry mouth, constipation, etc.).
Rickels et al. (2002) [13] studied paroxetine for GAD compared with placebo in an 8-week study. Paroxetine was used in doses of 20 and 40 mg. It turned out that in both doses the drug was significantly superior to placebo. However, efficacy varied depending on the dose of parksetine: at a dose of 20 mg there was a 68% responder rate, and at a dose of 40 mg there was an 81% response rate. Similar results were obtained in the study by Pollack MH et al. [14].
Paroxetine has also been effective in the long-term treatment of GAD, as well as as an anti-relapse therapy. 652 middle-aged patients with GAD were studied. It turned out that during long-term therapy with paroxetine, anxiety symptoms continued to decrease. The relapse rate in patients receiving paroxetine was significantly lower compared to placebo (10.9 vs. 39.9%). The time to relapse in the paroxetine group was also significantly longer than in the placebo group [15].
The effective daily dose of paroxetine for GAD is 20 mg, but if necessary it can be increased to 40-60 mg/day. without significant changes in safety and tolerability.
Social phobia (SSP)
SCF is manifested by a fear of being the center of attention, accompanied by fears of negative evaluation by others and avoidance of public situations.
In most cases, the disorder manifests itself between the ages of 14 and 18 years. Outbursts of anxiety are triggered by social situations, such as public speaking (exams at school, going on stage), eating in a public place, writing or talking on the phone in the presence of other people, using a public toilet. Anxiety attacks are accompanied by autonomic disorders characteristic of states of emotional stress (hot flashes, increased sweating, hand tremors, rapid heartbeat, etc.). According to epidemiological studies, the prevalence of social phobia is estimated at approximately 6%. In women, the disorder is somewhat more common.
Among the antidepressants used in the treatment of social phobia are SSRIs and reversible monoamine oxidase inhibitors (MAOIs). Clonazepam (a high-potency benzodiazepine anxiolytic) is also used.
Data on the effectiveness of paroxetine for social phobia were obtained in a double-blind, placebo-controlled study on 187 patients [16]. Paroxetine was used in a dose of 20-50 mg. Significant differences with placebo were revealed in all studied parameters, starting from the 4th week of therapy, and persisted until the end of the study. In a similar study with a sample of 290 patients, Baldwin et al. (1999) paroxetine was also effective in treating social phobia [17], and the differences between paroxetine and placebo reached statistical significance also from the 4th week of treatment. Paroxetine in daily doses of 20-50 mg was well tolerated by patients.
Post-traumatic stress disorder (PTSD)
PTSD develops after exposure to a psychotraumatic factor of extreme intensity (natural disasters, terrorist attacks, acts of violence). Approximately 16% of the population experiences natural disasters. Of these, 4% develop PTSD. The incidence of PTSD is significantly higher in people who have been taken hostage. According to various authors, it is in the range of 50-100%.
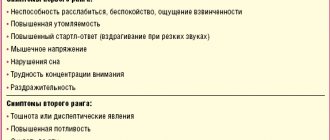
Clinical manifestations include persistently recurring unpleasant memories of a traumatic event. Increased physiological reactivity to internal or external stimuli that symbolize or resemble traumatic events. Patients attempt to avoid thoughts, feelings, or conversations related to the trauma and make efforts to achieve such avoidance. There is a noticeable decrease in interest or participation in previously meaningful activities, and a feeling of isolation or alienation from others. Some people complain of being “unemotional”—a limited range of feelings (for example, an inability to experience feelings of love). Among the symptoms of increased excitability, the most typical are difficulty falling asleep or early awakening, irritability or outbursts of anger, and difficulty concentrating. Increased alertness, hypervigilance, constant anticipation of a threat, and fearfulness bring PTSD closer to other anxiety spectrum disorders.
Despite the fact that the concept of PTSD was developed more than a quarter of a century ago, research on the effectiveness of pharmacotherapy for this disorder is still scarce. To date, 3 large placebo-controlled studies have been conducted on the effectiveness of paroxetine in PTSD [18,19]. These were 12-week studies where paroxetine was used at a dose of 20-40 mg. The results were similar. According to a meta-analysis of these studies, paroxetine therapy was effective in 57% of patients, significantly superior to placebo (39%). The effect of the drug was noted in relation to all the main signs of PTSD.
Obsessive-compulsive disorder (OCD)
The main manifestations of OCD are obsessive thoughts and actions. OCD is one of the most severe non-psychotic disorders. The disease is usually chronic, significantly complicating daily activities. By obsessive we usually understand mental manifestations that arise in the psyche independently and against desire, unexpectedly, and often suddenly, without direct connection with the content of thinking. It is impossible to free yourself from obsessions through a conscious volitional effort; they interfere with the correct flow of thoughts and slow it down. At the same time, patients retain a critical attitude towards obsessions, which distinguishes them from “overvalued” and delusional ideas.
The lifetime prevalence of OCD is approximately 2%. The disease manifests itself gradually after a long latent phase, lasting up to 10 years. The onset of the disease usually occurs between the ages of 14 and 24 years. OCD tends to have a persistent, chronic course, often being drug-resistant and significantly impairing daily activities.
A number of studies have proven the decisive role of serotonin mechanisms in the development of OCD. It is clear that among the pharmacotherapeutic agents for the treatment of OCD, serotonergic antidepressants are primarily used - primarily SSRIs and clomipramine. Moreover, the treatment of OCD requires higher doses of drugs than the treatment of depression, and the effect of treatment appears later. Reduction of symptoms is observed 3-4 weeks after the start of therapy.
A 12-week placebo-controlled trial in 348 patients with OCD compared paroxetine 20, 40 or 60 mg with placebo [20]. Paroxetine was significantly more effective than placebo at all doses studied. Interestingly, in more severely ill patients the response to paroxetine 60 mg was better than that of 40 and 20 mg.
Another 12-week randomized trial compared paroxetine with clomipramine and placebo [21]. The dose of paroxetine could vary in the range of 10-60 mg, clomipramine - 25-250 mg. The study involved 406 patients. Significant differences from placebo were recorded at week 6 in both the paroxetine and clomipramine groups. A 25% reduction in symptoms was observed in 55% of patients in both groups. Not surprisingly, paroxetine was much better tolerated than clomipramine. Refusals to continue therapy were only 9% (in the clomipramine group - 17%), the rate of adverse events was 16% (in the clomipramine group - 28%).
In long-term treatment, paroxetine has also shown to be effective. In a long-term (12-month) follow-up study involving 104 patients with OCD, the use of paroxetine significantly reduced the frequency of exacerbations compared to placebo [22].
Doses of paroxetine for the treatment of OCD are usually 40-60 mg per day; if necessary, the dose can be increased to 80 mg/day. The recommended minimum duration of maintenance therapy after remission is 1 year [22].
Literature
1. Robins, L.N., Helzer, J.E., Weismann, M.M., Orvaschel, H., Gruenberg, E., Burke, J., Regier, D.: Lifetime prevalence of specific psychiatric disorders in three sites. Arch. Gen. Psychiatry 41, 949-958 (1984).
2. Rouillon, F.: Depression comorbid with anxiety or medical illness: The role of paroxetine. Int. J. Psychiat. Clin. Practice 5, 3-10 (2001).
3. Ballenger, JC: Selective serotonin reuptake inhibitors in panic disorder. In: Selective Serotonin Reuptake Inhibitors. (2nd edition) (Eds.: Feighner J. P, Boyer, W.), Wiley, Chichester, 1996. pp. 155-178.
4. Mavissakalian, M, Perel, J.: Protective effects of imipramine maintenance treatment in panic disorder with agoraphobia. Amer. J. Psychiatry 194, 1053-1057 (1992).
5. Kessler, RC, et al.: Lifetime and 12month prevalence of DSM-III-R psychiatric disorders in the United States. Arch. Gen. Psychiatry, SI, 8-19. (1994)
6. Oehrberg, P.E. et.al. Paroxetine in the treatment of panic disorder: a randomized, doubleblind, placebo-controlled study. pit. J. Psychiatry 167, 374-379, (1995). 16. Ballenger, JC, Wheadon, DE, Steiner, M., Bushnell, W., Gergel, IP: Double-blind, fixed-dose, placebo-controlled study of paroxetine in the treatment of panic disorder. Amer. J. Psychiatry 155, 36-42, (1998).
7. Mavissakalian, M, Perel, J.: Clinical experiment in maintenance and discontinuation of imipramine in panic disorder with agoraphobia. Arch. Gen. Psychiatry 49, 318-323 (1992).
8. LeCrubier, Y., Bakker, A., Judge, R. and the Collaborative Paroxetine Study Investigators: A comparison of paroxetine, clomipramine and placebo in the treatment of panic disorder. Acta Psychiat. Scand. 95, 145-152. (1997).
9. Dunbar, G. C., Judge R.: Long-term evaluation of paroxetine, clomipramine and placebo in panic disorder. Eur. Neuropsychopharmacol. 5, 361, Abstract P5-27, (1995).
10. LeCrubier, Y., Judge, R. and the Collaborative Paroxetine Study Investigators: Long-term evaluation of paroxetine, clomipramine and placebo in panic disorder. Acta Psychiat. Scand. 95, 153-160. (1997).
11. Dunner, D, Kumar, R: Paroxetine: a review of clinical experience. Pharmacopsychiat. 3, 189-201 (1998).
12. Rocca, P., Fonzo, P., Scotta, M., Zanalda, E., Ravizza, L.: Paroxetine efficacy in the treatment of generalized anxiety disorder. Acta Psychiat. Scand. 95, 444-450 (1997).
13. Nutt D., Rickels K. Dan J. Stein (ed.): Generalized anxiety disorder. Symptomatology, pathogenesis and management. (2002), p. 143.
14. Pollack, MH, Zaninelli, R., Goddard A., McCafferty, JP, Bellew, KM Burnham, DB, Iyengar, MK: Paroxetine in the treatment of generalized anxiety disorder: results of a placebo-controlled, flexible-dosage trial. J. Clin. Psychiatry 62, (5), 350-357 (2001).
15. Ballenger JC Clinical guidelines for establishing remission in patients with depression and anxiety. J. Clinical Psychiatry, 60s, 29-34 (1999).
16. Stein, MB, Liebowitz, MR, Lydiard, R., B., Pitts, CD, Bushnell, W., Gergel, I.: Paroxetine treatment of generalized social phobia (Social Anxiety Disorder). JAMA, 280, (8), 708-713. (1998).
17. Baldwin D., Bobes, J., Stein, DJ, Scharwachter, I., Faure, M.: Paroxetine in social phobia/social anxiety disorder. pit. J. Psychiatry I75, 120-126. (1999).
18. Stein MB, Fyer AJ Davidson JRT, Pollac MH Wiita B: Paroxetine treatment of PTSD, a double-blind, placebo-controlled study. Am.J. Psychiatry, 156, 746-60 (1999).
19. Stein DJ Improving treatment options - new clinical data on paroxetine. CINP, 2000.
20. Wheadon D., Bushnell WD, Steiner M. A fixed-dose comparison of 20,40 or 60 mg of paroxetin to placebo in the treatment of obsessive-compassive disorder. American college of neuropsychopharmacology Annual meeting (1993)
21. Zohar, J., Judge, R.: Paroxetine versus clomipramine in the treatment of obsessive-compulsive disorder. pit. J. Psychiatry 169, 468-474 (1996).
22. Dunbar, G.C., Steiner, M., Bushell, W.D., Gergel, I., Wheadon, DE: Long-term treatment and prevention of obsessive-compulsive disorder with paroxetine. Eur. Neuropsychopharmacol. 5, 372 (1994).
PAXIL (tablets)
from the clinic, he said that it was VSD, and prescribed Mexidol, I took it for 3 months, but there was no effect.
And then my husband called his neurologist friend, and she, happily for me, prescribed Paxil. After reading the instructions, I decisively began treatment. The instructions say to take one tablet a day. And so I took one whole pill for the first time, and it was a nightmare... I felt unreal, hot and cold, shaking... two days of torment and I decided no, I won’t drink. But the doctor persuaded me that it’s still worth drinking them, and I shouldn’t give up the condition that many people have. But she really advised gradually increasing the dosage. And a miracle happened, I was on them without any side effects. I drank like this: 3 days, 1/4 tablet, 3 days, half a tablet, 3 days, 3/4 tablet And then a whole one. I felt just great, I became much calmer, I began to stay alone, go out somewhere, travel. The only thing while I was drinking them was that I completely eliminated alcohol and driving, although the instructions say that you can do this. And so I took my course prescribed by the doctor for 3 months, and began to “get off” them. I got down in the same way as I started drinking, only in reverse order. And here is the FIRST hellish day without them: I learned what withdrawal is! dizziness, blood pressure was then 80, after 10 minutes it was already 130, I was shaking and there were discharges all over my body, I walked and thought with difficulty, sometimes I could just get carried away, because my body doesn’t listen to you at all, I was either hot or cold. I chalked it all up to the weather (snow, then rain, and so on all day) and tried to lie down more, but since I have small children, my husband came to the rescue and sat with them. SECOND day: the same condition as the first, back to bed... and I think let me see what kind of reviews they write about Paxil and how to get off it. And I was simply shocked that people couldn’t do without it! And I decided to endure!!! Realizing that there are 3 tabs in my stash, and if I drink it, I will be human again, but I decided that I would not do this. Get off like that! THIRD day: I can’t... I call the neurologist and describe my condition and she says that I should have taken half and a quarter for 2 weeks so that my body wouldn’t wean itself off Paxil so abruptly, but there’s no point in me starting taking Paxil again. What did she advise me to alleviate the condition: 1. Drink more liquid (water) 2-3 liters; 2. Glycine up to 5 tablets per day, I took Glycine Forte up to 3-4 tablets; 3. Vitamins, I didn’t skimp, I bought natural ones with antioxidants; 4. Get over it. On my own behalf, I can add that I felt much better on the street than at home. And while I was doing something at home, there were no side effects of getting off, but as soon as I lay down in bed or sat down, it started rolling in... Conclusion, I need to find something to do, I wash my apartment 10 times a day) FOURTH day: when I followed the doctor’s recommendations, the dizziness went away, coordination is still impaired, nausea and discharges throughout the body remain, let’s bear with it. FIFTH day: coordination begins to return, I begin to feel human. Nausea and discharges throughout the body remain.
Let me say this, all this went away for me within 8-9 days! I just endured it, no matter how hard it was!!! And I got off them... now, after a week after all this, something comes up (like I’m afraid, I’m afraid), such small attacks. But I either calm myself down or scold myself, realizing that I don’t want to take any more antidepressants! As one person said, all our fears are in our heads, we screw ourselves up!!! and this is now my motto! The only thing is that I don’t drive alone in the car yet; I sit behind the wheel if there is someone nearby. I feel liberated)))
So good luck to you all in overcoming your Paxil addiction!!!