Pharmacology
Tablets are a medicinal product with a sedative and antispasmodic effect. Melissa, valearian and mint extract provides a calming and antispasmodic effect.
In general, after taking the drug there is a decrease in feelings of anxiety and nervousness. There is a noticeable improvement in the condition of people in an excited and emotional state. With insomnia, the patient falls asleep much easier and faster, sleeps more soundly, and does not feel drowsy throughout the day.
Persen has a general effect on the human body due to its constituent components. Therefore, no clinical studies have been conducted. It is not possible to determine the metabolites of the drug.
Persen
Persen from the Slovenian pharmaceutical is a patented combined herbal remedy that has a sedative effect. Natural sedatives are one of the main attributes of the recently popular trend towards naturalization of the healing process. According to a WHO survey, about 80% of the world’s population prefer “natural products” to medicines. And the patient’s high trust in the treatment method used can significantly increase the effectiveness of the latter. Persen contains three plant extracts: valerian, lemon balm and peppermint. Valerian extract has long gained fame as a sedative. The conducted studies indicate that the action of valerian is aimed at stimulating GABAergic mediation. This is due to a decrease in the reflex reactivity of the central nervous system with a simultaneous increase in the processes of neuronal inhibition. Such qualities of valerian make it possible to use it as a sedative for excessive nervous excitement. Valerian has a positive effect on sleep, increasing its quality. Moreover, it is absolutely non-toxic and even in high doses does not cause surges in blood pressure. The list of adverse events that can be observed when taking valerian is limited to allergic reactions. The second “whale” on which the sedative effect of persen is based is lemon balm. Which, in itself having a sedative effect, potentiates that of valerian, which makes these two plants a truly “shock” combination used in many sedative herbal preparations.
Scientists suggest that the effect of lemon balm on the central nervous system is mediated by its interaction with acetylcholinesterase in the brain and suppression of the activity of muscarinic and nicotinic receptors in the cerebral cortex. The last member of this natural sedative triumvirate is peppermint, which has a wide range of uses: this plant object is used as an antispasmodic, sedative, vasodilator and analgesic. There is information that peppermint in the form of essential oil eliminates nervous tension, increases vitality, and relieves stress. Persen is widely used in pediatric practice because dThis drug is considered “pure”, not containing synthetic products and ethyl alcohol. Its use can be successfully combined with almost any psychotropic drug. The undeniable advantage of Persen is its good tolerability, which sets it apart from other drugs used to correct sleep disorders and anxiety conditions.
Persen is available in tablets and capsules (in the latter case, the drug contains a larger amount of valerian and “forte” is added to its name). It is recommended to take this medication 2-3 tablets 2-3 times a day (for increased excitability) and 2-3 tablets 1 hour before going to bed for insomnia. For children, the optimal dose is selected by the doctor. Capsules are taken in slightly smaller quantities: 1-2 at a time.
Instructions for use
The tablets are intended for internal use. Can be taken at any time, regardless of meals. You need to drink enough water.
From 12 years old you can take 2 tablets 2 times a day. The attending physician will be able to prescribe the correct course of treatment.
If a person has insomnia, then you need to take 2 tablets in the evening an hour before bedtime. The maximum permissible dosage is 12 tablets per day.
The duration of continuous treatment should not exceed more than 45 days. After finishing taking the pills, withdrawal symptoms do not appear.
Adverse reactions and overdose
When taking pills, negative reactions may occur in the form of:
- allergies, manifested by hyperemia, bronchospasms and skin rash;
- Long-term use may cause constipation.
Cases of overdose are possible. Usually happens if more than 60 tablets have been taken. Nausea, vomiting, lethargy, pain inside the body, and dizziness may occur. 24 hours after taking the drug in large quantities, the signs of overdose disappear. No toxic effects are observed. If necessary, you can do symptomatic treatment.
Other information
The drug should be stored at room temperature. Shelf life – 36 months from the date of release. Sold in pharmacies without a doctor's prescription.
Before taking Persen, you need to familiarize yourself with the features of its action and in what cases the tablets will be effective. If during therapy the symptoms do not disappear or the condition becomes even more severe, then you need to seek help from a specialist.
In patients with gastroesophageal reflux disease, the condition may only worsen during treatment.
After taking the pills, it is better to stop driving a vehicle and other dangerous mechanisms.
The duration of the treatment course should not exceed 60 days. If negative reactions occur, you should immediately inform a specialist.
Experience with the use of the drug Persen for subthreshold anxiety spectrum disorders in adolescents
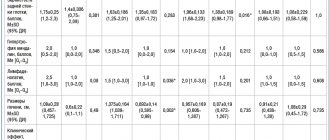
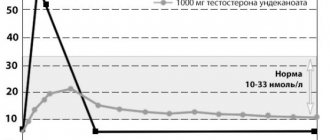
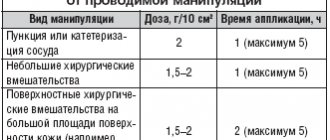
Anxiety disorders in adolescents often have nonspecific clinical manifestations affecting various organs and systems. The range of clinical syndromes and symptoms of anxiety can be extremely wide: from tension cephalgia, insomnia disorders to cardialgia, abdominal pain syndrome, and ventilation disorders. The pathogenesis of these manifestations is most likely based on psycho-vegetative syndrome. In adolescence, combinations of anxiety with comorbid disorders such as obsessive-compulsive syndrome, neurotic motor and vocal tics, secondary nocturnal enuresis, hysterical reactions, hypochondriacal and depressive (subdepressive) disorders, and phobias are often found. Correct diagnosis of somatized manifestations of anxiety disorder causes significant difficulties due to the need to exclude the entire spectrum of organic somatic pathology, which is associated with high material costs for conducting a complex of instrumental and laboratory examinations. An equally important aspect is the adequate interpretation of the examination results, the doctor’s ability not to overestimate the significance of random diagnostic findings, and in some cases, to recognize the mental attitudes of the patient’s environment. The greatest difficulties are caused by the diagnosis of subthreshold anxiety disorders, the most common in the population, considered in accordance with ICD-10 within the framework of nonspecific anxiety [5]. The diagnostic criteria for subthreshold anxiety disorder correspond to the presence of at least two anxiety symptoms listed in Table 1. These symptoms must be present simultaneously for at least two weeks and lead to deviations in the patient’s social adaptation. In adolescence, it should be noted the dynamism of anxiety symptoms, their transformation over time, the lack of persistence of the clinical symptom complex, which does not allow diagnosing any defined disease - a specific type of anxiety disorder. The presence of individual anxiety symptoms in adult patients, as a rule, is not considered by them or their loved ones as a significant pathological condition, so the motivation to seek medical help is often absent. Anxiety disorders in adolescents, as opposed to adults, to a greater extent acquire the character of a significant medical and social problem, since they disrupt family and school interactions, negatively affect academic performance, and can lead to maladaptation of children among their peers. In the absence of treatment, anxiety symptoms can undergo transformation, become more persistent - permanent and reach the level of delineated anxiety syndromes. According to the modern concept, the formation of anxiety syndrome is based on an imbalance of certain nervous system mediators: serotonin, norepinephrine and gamma-aminobutyric acid (GABA). Currently, there is a rich arsenal of anti-anxiety drugs that can influence not only mental, but also somatic manifestations of anxiety [12]. Anti-anxiety drugs exert their action precisely through these neurotransmitter systems. Among GABAergic anxiolytics, the leading place is occupied by benzodiazepine tranquilizers [10]. Tricyclic antidepressants and selective serotonin reuptake inhibitors act on anxiety through the noradrenergic and serotonergic systems [9]. However, drugs from these groups have known side effects, such as daytime drowsiness, inhibition of thought processes, depression of general condition, and the formation of drug dependence [11]. The listed side effects can neutralize the positive clinical effect expected from the drugs and often force the patient to interrupt the necessary course of treatment. In addition, such active drugs are usually recommended for patients only with clinically defined anxiety disorder syndromes. Official herbal preparations, which have significantly fewer side effects, can be considered as an alternative and highly safe therapy for subthreshold anxiety disorders. The basis of official anti-anxiety complex herbal remedies is valerian. It has been used in traditional medicine for many years due to its hypnotic and sedative effects and remains a highly sought after medicine to this day. The hypnotic effect of valerian is more obvious in individuals suffering from insomnia than in healthy individuals. The mild hypnotic effect of valerian makes it possible to use it to relieve minor insomnia disorders caused by anxiety. In addition, the vegetotropic effect of valerian is well known, its ability to have an even effect on both mental and somatic (vegetative) symptoms of anxiety. The range of side effects of valerian is very narrow and is practically limited only to allergic reactions. Despite the fact that valerian extract is metabolized by the cytochrome P450 system, it has virtually no effect on the metabolism of other drugs and, accordingly, unwanted drug interactions are excluded. Among the herbal medicines used by clinicians to treat subthreshold anxiety, the drug Persen (pharmaceutical), which is characterized by a favorable combination of anxiolytic and sedative effects, has become widespread. Along with valerian, the pharmacologically active components of the drug are dry extracts of medicinal plants with pronounced anxiolytic activity - peppermint and lemon balm. Thanks to the successful combination of the active components of Persen, an enhanced anti-anxiety effect is achieved. The additional antispasmodic effect allows the drug to be successfully used in patients with a pronounced somatic component of anxiety syndrome. Persen is available in two dosage forms: tablets and capsules (forte). One tablet of Persen contains 50 mg of valerian and 25 mg of peppermint and lemon balm. One capsule of Persen-Forte contains 125 mg of valerian extract. Patients and research methods A group of 48 adolescents (29 girls and 19 boys) aged 14 to 16 years (average age 14.94±0.84 years) who sought outpatient neurological care at the Department of Psychoneurology of the Children's Clinical Hospital was subjected to clinical analysis. No. 38 of the Federal Medical and Biological Agency. Clinical examination of patients was carried out in a standard manner and included analysis of anamnestic information, assessment of current complaints, neurological and somatic status, and psychological testing of a number of features of the emotional sphere and cognitive processes. The severity of pain in patients (mainly headaches) was assessed using a visual analogue scale (VAS). In order to exclude organic changes in the somatic sphere of patients, a comprehensive laboratory and instrumental examination was carried out. Conventional echographic diagnostic methods were used (echocardiography, sonography of the abdominal organs, transcranial Doppler sonography). All patients underwent electrocardiography. In some cases, esophagogastroduodenoscopy was performed for abdominal pain syndrome. Instrumental neurological diagnostics included electroencephalography, which was carried out in patients with paroxysmal disorders. Laboratory diagnostic methods included standard studies of hemogram, urogram, basic biochemical parameters of blood serum (total protein, bilirubin, liver transaminases, glucose, urea, creatinine, electrolytes). The results of a comprehensive clinical, laboratory and instrumental examination did not reveal any significant changes in the internal organs, as well as organic neurological disorders in the analyzed group of patients. Significant deviations during the examination were the criterion for excluding this patient from the analyzed group. Psychological examination of patients was carried out in two stages: during the initial visit to the doctor and again, after 2 months during the therapy. To diagnose the characteristics of the emotional sphere, standardized rating scales were used. The Spielberger Situational and Personal Anxiety Questionnaire, modified by A.D., was used. Andreeva for older adolescents [6], which allows identifying the level of cognitive activity, anxiety and negative emotional experiences; as well as a special questionnaire that allows you to assess your current state of health, activity and mood - the SAN questionnaire (an abbreviation for the first letters of “well-being–activity–mood”) [6]. To assess the current emotional state, the Luscher color test was also used [8]. To diagnose attention disorders, the following were used: the “Corrective Test” test, which allows assessing the stability of voluntary attention [6]; study of the volume and general indicator of attention switching using Gorbov-Schulte tables [6]. Comparison of the dynamics of quantitative indicators was carried out using the Wilcoxon T-test. The significance level of p<0.05 was considered reliable. All 48 patients were prescribed the drug Persen as monotherapy at a dose of 2 tablets up to 3-4 times a day (Persen) or 1 capsule. 2–3 times a day (Persen-forte). The duration of treatment was 2 months. Tolerability of the drug was satisfactory; no significant side effects that could predetermine interruption of the course of treatment were recorded. Results and discussion The range of main clinical complaints presented by patients at the initial outpatient appointment is reflected in Table 2. The etiological factors for the development of subthreshold anxiety disorder in the analyzed group, in most cases, were psycho-emotional stress, difficulties in school and family interaction against the background of existing premorbid features character of teenagers. Thus, in 64.6% of cases, the relationship between parents and a teenager from early childhood was of an overprotective nature; in 54.2% of cases, adolescents experienced emotional stress due to rejection and hostile attitude towards them from teachers and peers at school; 41.7% of the children examined experienced a feeling of uncertainty, inferiority, and inability to meet the requirements and expectations of the social environment. Among the premorbid personal characteristics of the examined children, the most significant were anxiety (100%), sensitivity (87.5%), the predominance of negative emotions over positive ones (47.9%), isolation (31.2%), low level of intellectual functioning in combination with expressed determination to achieve high results (29.2%). Analysis of complaints shows that the main disorders in patients concerned anxiety spectrum disorders with accompanying affective, phobic, cognitive and somatized vegetative manifestations. Painful manifestations in patients were represented mainly by chronic tension headaches (18 patients), which were characterized by moderate intensity, the absence of precursors, aura and focal loss. Headaches had a frontotemporal localization and developed after previous stress, occurring with a frequency of up to 3–5 times per month. Some patients (9 patients) experienced abdominal pain or a feeling of discomfort that occurred during moments of anxiety or emotional stress. The initial VAS score for pain manifestations was 6.63±1.08 points. During the initial clinical and psychological conversation with adolescents and their parents, the medical history data were clarified in the context of the social situation of the child’s development. It was noted that in 72.9% of cases, a decrease in mental performance, difficulty concentrating, and increased fatigue caused frequent conflicts between the teenager and his parents and teachers due to deterioration in academic performance and decreased motivation for schooling. Increased irritability and affective excitability in 43.8% of cases led to disruption of social interactions among adolescents both in the family environment and among peers, while in 10.4% of children these disturbances reached the level of social maladjustment. During the treatment, the following clinical symptoms significantly regressed (the percentages of patients whose complaints persisted after the course of treatment are indicated): a feeling of unmotivated anxiety (10.4%), general weakness (41.7%), fatigue (29.2%), decreased performance (31.3%), difficulty concentrating (33.3%), decreased mood (20.8%), feeling of internal tension (37.5%), headaches (14.6%), sleep disturbance (8.3%). The VAS score after the course of therapy significantly improved (p<0.001) and amounted to 3.93±1.41 points. Figures 1 and 2 show the dynamics of indicators of cognitive activity, anxiety and negative emotional experiences, assessed on the Spielberger scale for older adolescents. The initial values of personal anxiety on this scale were 28.83±5.38 points, which indicated a high probability of a teenager developing anxiety in situations where his competence and preparedness were assessed, and his tendency to perceive them as threatening. During treatment, a significant decrease in personal anxiety was noted to 21.98±3.77 points, which corresponded to the average level of values. The range of situations causing anxiety was significantly limited, cognitive activity and learning motivation increased. The level of reactive anxiety in the study group of adolescents, which is determined by the subjectively experienced emotions of tension, anxiety, concern, nervousness and is accompanied by autonomic dysfunction, initially amounted to 29.19±5.63 points and corresponded to high values of the scale. At the time of the re-examination, there was a significant change in this indicator to 22.69±4.60 points, which indicated a decrease in the intensity of the patient’s psycho-emotional stress. The dynamics of the emotional state of patients during treatment were also assessed using the Luscher color test. During the initial treatment, in 39.6% of cases, a preference for achromatic and mixed colors was observed in the first two positions of the row, indicating a state of pronounced emotional stress, fatigue, feelings of uncertainty, anxiety, fearful fears, limitation of vigorous activity and social contacts. At the time of the repeated psychological examination, in 35.4% of cases, a pronounced reverse dynamics of the emotional state was noted in the form of harmonization of the color range, the movement of bright and mixed colors to the first positions, which indicated the normalization of the general background of mood, an increase in the need for action, activity, sociability, motivation achieving success. A significant increase in indicators (Fig. 3) was noted in adolescents’ subjective assessment of well-being (from 3.31 to 5.44 points), activity (from 4.11 to 4.60 points) and mood (from 3.88 to 4.98 points ) during treatment. The study of the dynamics of indicators of voluntary attention processes, as the main indicator of mental performance and organization of mental activity, indicated a significant improvement in productivity and accuracy during therapy, and an expansion of the volume of voluntary attention (Table 3). There was a decrease in the average time spent on completing tasks in four Gorbov-Schulte tables, an increase in the number of letters looked at in the “Proofreading Test” test, and a decrease in the percentage of errors made. Thus, against the background of the treatment, the majority of the examined adolescents showed a significant decrease in the intensity of signs of anxiety, an improvement in general well-being, mood, an increase in cognitive activity, and a normalization of voluntary attention processes. Along with the improvement in mental parameters, positive dynamics were noted in relation to somatized vegetative disorders and pain manifestations. The treatment significantly improved the quality of life in the analyzed group of patients. Summarizing the material from the study, we can conclude that Persen is a fairly highly effective drug in terms of its effect on subthreshold anxiety spectrum disorders. This conclusion confirms the conclusions of other researchers who observed the positive effect of the drug in patients with psychovegetative syndrome in the structure of anxiety neurotic disorders [2,3]. The drug has a good safety profile, is well tolerated, and has virtually no significant side effects or adverse reactions. Persus is convenient to use, does not cause daily sedation and oppression, which seems to be very important, since it does not interfere with the processes of study and the social interaction of patients. The drug is practically deprived of the properties of undesirable interactions with other drugs used by persons with concomitant chronic diseases. The drug is a good alternative to the use of synthetic pharmacotherapeutic agents, especially in cases of subsporage anxiety disorders, which is most relevant in the practice of treating children and adolescents.
Literature 1. Avedisova A.S. Anxiety disorders. In the book: Aleksandrovsky Yu.A. “Mental disorders in general medical practice and their treatment.” M: GEOTAR-MED. – 2004. – P. 66 – 73. 2. Voznesenskaya T.G., Fedotova A.V., Fokina N.M. Persen-forte in the treatment of anxiety disorders in patients with psychovegetative syndrome // Treatment of nervous diseases. – 2002. – No. 3 (8). – pp. 38–41. 3. Vorobyova O.V. Psychovegetative syndrome associated with anxiety (issues of diagnosis and therapy) //Russian Medical Journal. – 2006. – Vol. 14. – No. 23. – P. 1696–1699. 4. Korkina M.V., Lakosina N.D., Lichko A.E. Psychiatry. – M. – 1995. – 608 p. 5. Popov Yu. V., Vid V. D. Modern clinical psychiatry // St. Petersburg: Expert Bureau. – 1997. 6. Workshop on developmental psychology. // Ed. Golovey L.A., Rybalko E.F. – St. Petersburg: Speech. – 2002. – 694 p. 7. Smulevich A.B. Depression in general medical practice. – M. – 2000. – 160 p. 8. Sobchik L.N. Introduction to the psychology of individuality. – M.: Institute of Applied Psychology. – 1998. – 512 p. 9. Davidson JRT. Pharmacotherapy of generalized anxiety disorder // J Clin Psychiatry. – 2001. – Vol.62 (suppl. 11). – P. 46–50. 10. Fricchione G. Generalized anxiety disorder // New Engl J Med. – 2004. – Vol.351 (7). – P.675–682. 11. Roerig JL. Diagnosis and management of generalized anxiety disorder // J Am Pharm Assoc. – 1999. – Vol. 39. – P. 811–821. 12. Rouillon F. Long term therapy of generalized anxiety // Eur J Psychiatry. – 2004. – Vol. 19(2). – P. 96–101.