- Treatment of dysmenorrhea
- Attending doctors
- Prices for services
Dysmenorrhea (algodysmenorrhea) is a menstrual disorder characterized by pain during menstruation. According to statistics, more than half of women of reproductive age complain of painful menstruation. In order to avoid dangerous complications, it is very important to diagnose the pathology in a timely manner and undergo a course of treatment.
We are talking about dysmenorrhea only if the pain syndrome is severe enough. According to various sources, approximately every tenth woman experiences significant pain that is cyclical in nature and associated with menstruation. Moreover, in many cases, patients note not only pain, but also a noticeable deterioration in their general condition, decreased performance, changes in psycho-emotional state, and forced abandonment of the usual rhythm of life.
Causes of dysmenorrhea
The main causes of dysmenorrhea:
- congenital defects that appear as a result of exposure to negative factors during the period of intrauterine development of the fetus - a closed accessory vagina, a closed uterine horn. During menstruation, blood accumulates in the accessory structures, causing intense pain. Sometimes such formations reach quite large sizes, the pain becomes very severe and is even accompanied by a short-term loss of consciousness. The intensity of the pain increases with each menstrual cycle, forcing the patient to see a doctor;
- spasm of the smooth muscles of the uterine body, caused by deviations in the synthesis and metabolism of prostaglandins and thromboxanes. These are biologically active substances that are produced in almost all organs and structures. Some of them are the main mediators of pain and inflammation, others regulate the tone of smooth muscles, and others are responsible for the condition of the microvasculature. By acting on the myometrium, prostaglandins provoke intense contraction of myocytes, which is externally manifested by severe pain. It should be noted that pathological abnormalities can be either congenital or acquired;
- hormonal imbalance, especially excess estrogen in combination with progesterone deficiency. Estrogen is produced by the ovaries; the corpus luteum, which appears after ovulation at the site of the burst follicle, is responsible for the production of progesterone. An increased amount of estrogen increases myometrial spasm, which leads to pain;
- endometriosis is a gynecological nosology of a chronic nature, which is manifested by the appearance of pathological foci of endometrioid tissue. These lesions, like the normal inner lining of the uterus, are susceptible to cyclic changes - in the first half they grow, in the second they are rejected. The process is accompanied by the accumulation of blood, the development of inflammation and the formation of adhesions in the affected area;
- ovarian tumors, especially those producing hormonal substances;
- fibroids are benign neoplasms of the uterus that develop from the myometrium. This is one of the most common gynecological diseases. According to statistics, fibroids are diagnosed in every fourth woman. The main symptom of fibroids is heavy and prolonged periods, often with the release of blood clots. The pain is cramping in nature, reminiscent of a feeling of heaviness. If the fibroid is located close to the peritoneum, dyspepsia and severe pain in the entire abdomen often occur;
- an incorrectly installed or misaligned spiral is a structure made of a polymer material with the addition of metal. This is a reliable means for preventing unwanted pregnancy, which is installed in the uterine cavity. If for some reason the IUD has moved, or was initially installed incorrectly, it can cause severe menstrual pain and intense bleeding;
- varicose veins of the small pelvis, accompanied by inflammation;
- diseases of the reproductive system of an infectious nature - endometritis (inflammation of the endometrium), salpingitis (inflammation of the fallopian tubes), adnexitis (inflammation of the fallopian tubes and ovaries). Most often, these processes are provoked by pathogenic microflora, infection of which occurs through unprotected sexual contact. When the ovaries are involved, in addition to direct inflammation, there is a disruption in the production of hormones;
- formation of adhesions in the pelvis. Adhesions are rather dense formations, peculiar cords, consisting mainly of collagen fibers. By preventing the normal contraction and relaxation of the uterus during menstruation, adhesions cause quite intense pain (read more here);
- incorrect position of the uterus, as a result of which expulsion of the functional layer of the endometrium and bleeding is difficult;
- delayed sexual development, genital infantilism;
- suffered injuries to the genital organs.
Depending on the cause, dysmenorrhea is of two types - primary and secondary.
Causes of dysmenorrhea
Dysmenorrhea
B
Painful menstruation is commonly called dysmenorrhea. This disease is a relatively common menstrual dysfunction. Dysmenorrhea is a Greek word that literally means “difficult menstrual flow.” Hippocrates also believed that the most important cause of dysmenorrhea is a mechanical obstacle to the release of blood from the uterine cavity. Subsequently, the view on the cause of dysmenorrhea progressively changed. It is very interesting to note that, according to various researchers, the frequency of dysmenorrhea ranges from 8 to 80%, and often only those cases of dysmenorrhea that reduce a woman’s normal level of activity or require medical intervention are statistically taken into account. About 1/3 of women suffering from dysmenorrhea are unable to work for 1-5 days every month. Among all the reasons for girls' absence from school, dysmenorrhea ranks first. A connection was revealed between social status, nature and working conditions and the severity of dysmenorrhea. Moreover, among women engaged in physical labor and athletes, the frequency and intensity of dysmenorrhea is higher than in the general population. Heredity plays an important role - in 30% of patients, mothers suffered from dysmenorrhea. Some researchers have found that the occurrence of dysmenorrhea is preceded by various adverse effects of the external environment on a woman’s body (hypothermia, overheating, infectious diseases) and stressful situations (physical and mental trauma, mental and physical overload, etc.).
| Dysmenorrhea is usually divided into primary and secondary. With primary dysmenorrhea in women, as a rule, there are no pathological changes in the genital organs. With secondary dysmenorrhea, the appearance of pain in the lower abdomen during menstruation is associated with various (most often gynecological) diseases. |
Secondary dysmenorrhea is a symptom of a number of diseases, most often endometriosis, inflammatory diseases of the pelvic organs, developmental anomalies of the internal genital organs, ruptures of the posterior leaf of the broad ligament (Allen-Masters syndrome), varicose veins of the pelvic veins of the parietal or in the area of the ovarian ligament, etc. Primary Dysmenorrhea, as defined by most authors, is a cyclic pathological process, expressed in the fact that on the days of menstruation, severe pain in the lower abdomen appears, which can be accompanied by severe general weakness, nausea, vomiting, headache, dizziness, lack of appetite, increased body temperature to 37 - 38 0 C with chills, dry mouth or drooling, bloating, feeling of “wobbly” legs, fainting and other emotional and autonomic disorders.
Sometimes the leading symptom may be one of the listed complaints, which bothers the patient more than pain.
Severe pain depletes the nervous system, contributes to the development of an asthenic state, reduces memory and performance. All symptoms of dysmenorrhea can be divided into emotional-mental, vegetative, vegetative-vascular and metabolic-endocrine. Emotional and mental:
irritability, anorexia, depression, drowsiness, insomnia, bulimia, odor intolerance, taste perversion, etc.
Autonomic:
nausea, belching, hiccups, chills, feeling hot, sweating, hyperthermia, dry mouth, frequent urination, tenesmus, bloating, etc.
Vegetative-vascular:
fainting, headache, dizziness, tachycardia, bradycardia, extrasystole, pain in the heart, cold snap, feeling of numbness in the arms and legs, swelling of the eyelids, face, etc.
Exchange-endocrine:
vomiting, feeling of “woolly » legs, general severe weakness, itchy skin, joint pain, swelling, polyuria, etc.
Primary dysmenorrhea
Primary dysmenorrhea usually appears in women during adolescence, 1-3 years after menarche, with the onset of ovulation. In the first years of the disease, pain during menstruation is usually tolerable, short-lived and does not affect performance. Over time, there may be an increase in pain, an increase in its duration, and the appearance of new symptoms accompanying the pain. Pain usually begins 12 hours before or on the first day of the menstrual cycle and continues during the first 2-42 hours or the entire menstruation. The pain is often cramping in nature, but can be aching, tugging, bursting, and radiate to the rectum, appendage area, and bladder. In the clinical picture of dysmenorrhea, compensated and uncompensated forms are distinguished. In the compensated form of the disease, the severity and nature of the pathological process on the days of menstruation do not change over time. In the uncompensated form, the intensity of pain in patients increases every year.
Table 1 System for rating dysmenorrhea by severity
| Severity | Performance | Systemic symptoms | The effectiveness of prescribing analgesics |
| 0 – menstruation is painless, does not affect daily activities | Doesn't decrease | None | Prescribing analgesics |
| I - menstrual bleeding is accompanied by mild pain and only rarely leads to a decrease in the woman’s normal daily activity | Rarely decreases | None | Analgesics are rarely required |
| II - daily activity is reduced, absenteeism from school or work is rare, as analgesics have a good effect | Moderately reduced | Single | Analgesics have a good effect, but they must be taken |
| III - daily activity is sharply reduced, analgesics are ineffective, the presence of vegetative symptoms (headache, fatigue, nausea, vomiting, diarrhea, etc.) | Sharply reduced | Occur frequently | Ineffective |
Greek scientists Efthimios Deligeoroglou and D.I. Arvantinos in 1996 developed a system for assessing dysmenorrhea by severity (Table 1). Etiology of dysmenorrhea
not clear.
There are several theories of its development; at different times, the origin of dysmenorrhea was explained by different factors (both physiological and psychological). Currently, most researchers associate the occurrence of primary dysmenorrhea with high levels of prostaglandins
(PG) F2a and E2 in the menstrual endometrium.
PGs are actually found in all tissues of animals and humans. They belong to the class of unsaturated fatty acids. PGF2a and PGE2 are the most likely causative factors causing dysmenorrhea. PGs are not hormones. Hormones are substances secreted by the endocrine glands, which, spreading through the bloodstream, have a biologically active effect on various systems of the body. PGs are produced by various tissues and exert their effect where they are synthesized. The obligate precursor of PG is arachidonic acid. This fatty acid is usually present among tissue phospholipids. Arachidonic acid is released by enzymes called phospholipases. Free arachidonic acid can be converted into various compounds. The enzymes that catalyze this reaction are called cyclooxygenases. With the help of cyclooxygenase, arachidonic acid is converted into the following 3 compounds: prostacyclin (PGI2), thromboxane (A2) and PG D2, E2 F2a PGE2 and PGF2a are powerful stimulators of myometrial contractile activity. An increase in the concentration of F2a and an increase in the PGF2a / PGE2 ratio cause dysmenorrhea. Table 2 Doses of non-steroidal anti-inflammatory drugs for the treatment of dysmenorrhea
| A drug | Recommended dose |
| Ibuprofen | 300 mg 3 or 4 times a day 400 mg 3 or 4 times a day 600 mg 3 or 4 times a day |
| Indomethacin | 25 mg 3 or 4 times daily |
| Mefenamic acid | 250 mg 3 or 4 times a day 500 mg 3 or 4 times a day |
| Naproxen | 250 mg 2 times a day 275 mg 2 times a day 550 mg 2 times a day |
| Ketoprofen | Capsules: 1 capsule (50 mg) in the morning with meals, 1 in the afternoon, 2 capsules in the evening (or 1-2 suppositories per day). 1 capsule morning and afternoon and 1 suppository (100 mg) in the evening. Tablets: 1 tablet forte (100 mg) 3 times a day or 1 tablet retard (150 mg) 2 times a day with an interval of 12 hours. The daily dose of the drug should not exceed 300 mg |
| Diclofenac | 25-50 mg 2-3 times a day. Maximum daily dose 150 mg |
The formation and release of PG from the endometrium is provoked by many irritants - stimulation of nerves and a decrease in oxygen delivery to the organ, exposure to hormones and simple mechanical stretching of the organ, etc. In some cases, in response to these irritations, the organ releases PGs in quantities that are tens of times greater than their concentration in this organ at rest. An excess of PGs is associated with both an increase in their synthesis and a decrease in their catabolism. Their level in menstrual blood in women with dysmenorrhea is significantly higher than in healthy women, and decreases with appropriate treatment. Drugs commonly used to treat dysmenorrhea act by blocking the activity of cyclooxygenase, and therefore inhibiting the production of prostacyclin, thromboxane and PG. Cyclic fluctuations in the concentration of PG/F2a in the blood of women with a peak during menstruation have been described (similar cyclic fluctuations for PGE2 have not been described). An increase in PG levels in the secretory endometrium occurs long before menstruation. There is no doubt that during the luteal phase the endometrium secretes PG. An increase in the content of PGF2a of uterine origin was noted, coinciding with the regression of the corpus luteum. The role of PG in regression of the corpus luteum in women remains unclear. The presence of hormonal regulation of PG synthesis is evidenced by a positive correlation between the high level of PGF2a in the middle and late period of the secretory phase and the level of estradiol. The stimulating effect of estrogens on the synthesis of PG and progesterone has been proven. A decrease in progesterone levels at the end of the menstrual cycle causes the release of phospholipase A2 from endometrial cells. This enzyme, acting on cell membrane lipids, leads to the release of arachidonic acid and, with the participation of prostaglandin synthetase, to the formation of PGs F2a, I2 and E2. PGs are involved in the contraction of spiral arterioles, which causes the menstrual reaction. Tissue rejection leads to an increase in their content, which explains their high concentration in menstrual blood. A high level of PG leads to increased contractile activity of the uterus, vasospasm and local ischemia, which in turn causes pain, since it is the disturbance of pelvic hemodynamics in the form of hypertension and vasospasm or prolonged vasodilation and venous stagnation that contributes to cell hypoxia and the accumulation of halogenic substances , irritation of nerve endings and pain. At the same time, there is an increase in intrauterine pressure and amplitude, as well as the frequency of uterine contractions by 2 - 2.5 times, compared with women whose menstruation is painless. Increased pain is facilitated by the accumulation of potassium salts in tissues and the release of free active calcium. In addition, under the influence of an increased concentration of PG, ischemia of other organs and tissues may occur, which leads to extragenital disorders in the form of headache, vomiting, diarrhea, etc. The introduction of antiprostaglandin drugs leads to a marked decrease in pain intensity in almost 80% of women with dysmenorrhea. of vasopressin is also widely discussed in the literature.
.
Studies have shown that in women with dysmenorrhea, the concentration of vasopressin in the blood plasma during menstruation is increased. The administration of vasporessin increases the contractile activity of the uterus, reduces uterine blood flow and causes dysmenorrhea. Infusion of vasopressin leads to an increase in the concentration of PGF2a in the blood plasma. The action of vasopressin is not blocked by antiprostaglandin drugs. Perhaps this is what explains the ineffectiveness of treatment for dysmenorrhea in some cases. However, it has been proven that combined oral contraceptives lead to a decrease in the content of this substance, confirming the validity of simultaneous treatment with oral contraceptives and antiprostaglandin drugs. The same modulator of PG release is bradykinin and oxytocin, which change the supply of oxidation substrate (free fatty acids), apparently through a calcium current. A positive feedback relationship was noted between the PG content and the effect of oxytocin. Publications devoted to the etiology of primary dysmenorrhea also constantly emphasize the significant role of mental factors
.
Sensitivity to pain plays an important role in a woman's response to increased spasmodic contractions of the uterus during menstruation. Pain
is a unique psychophysiological state of a person that arises as a result of exposure to super-strong or destructive actions that cause an organic or functional disorder in the body. Pain is an integrative function that mobilizes a wide variety of body functions to protect it from the effects of a harmful factor and includes components such as consciousness, sensation, memory, motivation, autonomic, somatic and behavioral reactions, and emotions. Reactions that occur in animals and humans to the action of a stimulus that can cause damage to the body or carries the danger of such are called nociceptive reactions (from the Latin nocere - to harm). The question of whether there are specific pain receptors or whether pain arises as a result of irritation of various receptors when a certain intensity of stimulation is reached is still a subject of debate. According to the most common opinion, one of the components of pain - painful sensation - occurs when non-encapsulated nerve endings are excited. For the sensation of pain to occur, it is necessary to irritate the nerve endings with biologically active substances, mainly from the group of kinins, PGs, as well as some ions (K, Ca), which are normally found inside cells. Under the influence of damaging factors that disrupt the permeability of membranes, these substances enter the intercellular spaces and irritate the nerve endings located here. It is currently believed that, due to their physiological properties, these free nerve endings are chemoreceptors. It has been established that the receptors that perceive nociceptive stimuli have a high threshold of excitability. The level of excitability is regulated by special fibers of the sympathetic division of the autonomic nervous system. Excitation caused by nociceptive stimulation is carried out through both thin myelinated and non-myelinated fibers. The concepts of “pain receptors” and “pain conductors” should be considered conditional, since the pain sensation itself is formed in the central nervous system. The process of transmission and processing of excitations that form pain is ensured by structures located at different levels of the central nervous system. The most important structure that processes information entering the brain is the reticular formation, where the reaction to painful stimulation appears earlier than in the cerebral cortex. This electroencephalographic reaction is expressed in the appearance of a slow regular rhythm with a frequency of 4-6 vibrations per 1 s, which is called the tension rhythm, as it accompanies a state of stress. Based on many experimental data, a position was formulated according to which the activation reaction of the cerebral cortex, which occurs during nociceptive stimulation, is formed with the participation of the adrenergic substrate of the reticular formation. It has been established that narcotic substances and analgesics exert their effect primarily on this area of the brain. The possibility of obtaining an analgesic effect without turning off consciousness indicates that the state of wakefulness and the conscious sensation of pain are provided by various brain mechanisms. It has long been believed that the leading role in the formation of sensations belongs to the thalamus. This is confirmed by modern data obtained in experiments and clinics. The limbic system of the brain, which is directly related to memory, motivation and emotions, is also involved in the formation of pain integration. Medicinal substances from the group of tranquilizers, which have a predominant effect on the limbic structures of the brain, have little effect on the threshold of excitation, but clearly modify pain integration as a whole, affecting mainly emotional manifestations. The criteria for assessing pain include various indicators (measurement of cardiac activity, respiration, blood pressure level, pupil size, galvanic skin reflex, cry, reaction of avoidance and aggression, electrophysiological indicators, biochemical changes in the blood, endocrine shifts, etc.) Intensity of pain sensation depends on a number of factors: the type of autonomic nervous activity, psychological mood, emotional background, and the environment in which the patient is located. It is known that strong motivations, efforts of the will of the patient himself, switching attention to some kind of intellectual activity, etc. can reduce or even completely suppress the sensation of pain. In case of mental disorders (some forms of schizophrenia, extensive lesions of the frontal lobes of the brain, alcohol intoxication), pain sensitivity may be impaired and even a painless course of severe pathological conditions.
Secondary dysmenorrhea
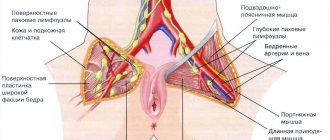
Secondary dysmenorrhea is caused by organic changes in the pelvic organs. It usually occurs several years after the start of menstruation, and pain may appear or intensify 1-2 days before the start of menstruation. Secondary dysmenorrhea, unlike primary dysmenorrhea, occurs most often in women after 30 years of age. One of the most common causes of secondary dysmenorrhea is the inflammatory process in the pelvic organs and endometriosis. Dysmenorrhea can also be caused by the use of an intrauterine device. Dysmenorrhea in diseases of the internal genital organs occurs as a result of impaired blood flow, spasm of smooth muscles, stretching of the walls of hollow organs, excessive irritation of the nervous elements during contractions of the uterus, inflammatory changes in organs and tissues, endometriosis, developmental abnormalities, etc. In chronic inflammatory processes, the tension of the adhesions formed between the abdominal covering of the uterus and neighboring organs is important. A vaginal examination of the pelvic organs may reveal signs of pathology such as pain, enlargement of the uterine appendages, and limited mobility. With endometriosis, there may be a similar clinical picture, however, with this pathology, pain can be observed throughout the entire cycle and intensify 2 - 3 days before menstruation. Most often, they are not cramping, but aching in nature, with irradiation to the rectum, appendages, lumbar region, etc. (depending on the location of endometrioid heterotopias) and are most pronounced on days when menstrual flow is especially intense. During a gynecological examination of the pelvic cavity, roughness and thickening of the uterosacral ligaments, pain when the uterus is displaced, soreness, enlargement, immobility of the appendages, changes in the size of the uterus and ovaries before and during menstruation and their reduction after its end, the uterus becomes spherical with heterogeneous consistency shape, most often deviated posteriorly and limited in mobility. When internal organs are damaged, it is diagnostically important to identify the corresponding neurological symptoms, in particular, the identification of pain points, sensory disturbances, and symptoms of tension in the nerve trunks. However, the latter does not exclude the presence of combined processes (diseases of the nervous system and secondary involvement in the process of receptors and pain sensitivity pathways in somatic diseases). Dysmenorrhea may occur in women who use intrauterine contraception. It has been proven that when using an IUD, the concentration of PG in the endometrium during the adaptation period increases and causes increased contractile activity of the uterus, which in women with an increased threshold of excitability leads to dysmenorrhea. Dysmenorrhea can also develop in women with uterine malformations that impede the outflow of menstrual blood and myomatous nodes that are born when the node reaches the internal os and is pushed out through the cervical canal by contractions of the uterus. Methods for diagnosing secondary dysmenorrhea include culture of material taken from the cervix and vagina, pelvic ultrasound, hysterosalpingography, hysteroscopy, laparoscopy, etc. One of the important diagnostic points in recognizing the nature of the pathological process is the effectiveness of medications that affect various levels of pain integration.
Treatment of dysmenorrhea
The main treatments for primary dysmenorrhea are oral contraceptives and non-steroidal anti-inflammatory drugs.
Oral contraceptives
reduce the volume of menstrual flow by inhibiting endometrial proliferation and suppressing ovulation.
Under conditions of anovulation, PG secretion by the endometrium decreases. Oral contraceptives cause a decrease in the threshold of excitability of the smooth muscle cell and reduce its contractile activity, thereby helping to reduce intrauterine pressure, frequency and amplitude of contractions of the uterine muscle. Increased uterine contractility may be the result of an increase in estrogen concentrations in the luteal phase of the cycle. Estrogen can stimulate the release of PGF2a and vasopressin. The use of combined estrogen-gestagen-containing monophasic contraceptives (rigevidon, microgynon, miniziston, marvelon, femoden, mersilon, etc.) and contraceptives containing only progestogen (continuin, microlut, excluton, depo-provera, norplant, intrauterine hormonal system "Mirena" etc.), leads to a decrease in the concentration of estrogen, and therefore PG, and the disappearance or reduction in the severity of symptoms of dysmenorrhea. Combined estrogen-gestagen-containing contraceptives for the treatment of primary dysmenorrhea are taken according to the usual regimen: 1 tablet daily at the same time of day, starting from the 5th day of the menstrual cycle, until the end of the package, a 7-day break, then the next package. Mini-pills are used daily, 1 tablet at the same time of day, continuously. Injectable contraceptives, for example Depo-Provera, are used once every 3 months, intramuscularly. The first injection is given on the 1st - 5th day of the menstrual cycle. Norplant is injected under the skin of the forearm on days 1–5 of the cycle. The intrauterine hormonal system is introduced on the 4-8th day of the menstrual cycle. If contraceptives do not provide the desired effect, PG synthetase inhibitors are additionally prescribed. PG synthetase inhibitors
are considered the drugs of choice for young women who do not wish to use oral contraceptives for the treatment of primary dysmenorrhea, and in cases where these drugs are contraindicated.
The most widely used PG synthetase inhibitors are non-steroidal anti-inflammatory drugs: aspirin, indomethacin, ibuprofen, mefenamic acid, naproxen, etc. Typically, a non-steroidal anti-inflammatory drug is prescribed orally from the 1st day of the menstrual cycle until pain completely subsides. The prescription regimen is as follows: when pain appears - 1 tablet, every subsequent 3 - 6 hours - 1 tablet until the pain completely disappears, or from the moment the pain begins - a double dose (2 tablets), then 1 tablet 3 - 4 times a day until complete disappearance pain relief. PG synthetase inhibitors reduce the PG content in menstrual blood and relieve dysmenorrhea. These drugs themselves have an analgesic effect, and the advisability of their use during the first 48–72 hours after the onset of menstruation is determined by the fact that, as researchers have shown, PGs are released into the menstrual fluid in maximum quantities in the first 48 hours of menstruation. Antiprostaglandin drugs are rapidly absorbed and act within 2 to 6 hours. Most of them must be taken 1 to 4 times a day in the first few days of menstruation (Table 2). Aspirin, being a mild cyclooxygenase inhibitor, helps only some patients. Paracetamol is also not effective enough in most cases. In the treatment of primary algodismenorrhea, zomepirac, fentiazac, flubiprofen, diclofenac, ketoprofen, piroxicam, etc. are also used. However, all of these drugs can have a number of side effects, both extragenital and antifertility, which may limit their use in gynecological patients. Although serious complications and significant side effects are usually rare and most women tolerate them well. The use of antiprostaglandin drugs is contraindicated for gastric or duodenal ulcers, gastritis and other diseases of the gastrointestinal tract, as they can cause an exacerbation of the process. There is also a prophylactic option for using the drugs:
1-3 days before the expected menstruation, 1 tablet 2-3 times a day.
The course of treatment usually lasts 3 menstrual cycles. The effect of non-steroidal anti-inflammatory drugs lasts for 2 - 3 months after their discontinuation, then the pain resumes, but is less intense. Given that in a controlled study using placebo, some patients felt better after receiving a placebo, it appears to make sense to prescribe a multidrug treatment that includes vitamins, amphetamines, and tranquilizers. The effectiveness of placebo is 21 - 41%, which indicates the importance of cortical regulation in this pathological condition. antioxidants
in order to limit pain .
In particular, a natural antioxidant - a-tocopherol acetate (vitamin E) 150-200 mg/day orally 3-4 days before the start of menstruation (preventive option) or 200-300 mg/day starting from the 1st day of menstruation (therapeutic option). For the treatment of primary dysmenorrhea, antispasmodics, calcium channel blockers, nonspecific analgesics, progestogens, gonadotropin-releasing hormone analogues, magnesium are also used, dilation of the cervical canal and its curettage are performed, methods of neurectomy in the presacral region, transcutaneous electrical nerve stimulation and acupuncture are used. Psychotherapeutic assistance that affects the reactive component of pain can also have a good effect. If nonsteroidal anti-inflammatory drugs are ineffective for dysmenorrhea, calcium and serotonin antagonists, b -stimulants, and antispasmodics are prescribed.
The activity of the uterine muscles is characterized by high active and residual pressure and largely depends on the concentration of free calcium in the cytoplasm.
Dysfunction of the uterine muscles is explained by changes in the content of free active calcium. An increase in the level of free calcium in the uterus stimulates the formation of PGF2a, and this process is hormone dependent. It is interesting that the relationship between free calcium content and PG levels is unidirectional, i.e. It was noted that prostaglandins E2 and F2a do not change the calcium current into the cell. Thus, calcium antagonists indirectly reduce the content of prostaglandins, thereby reducing the frequency of uterine contractions, intrauterine pressure and, accordingly, the severity of dysmenorrhea. Uterine contractions are often painless, and pain may be due to irritation of the endocervix. Under the influence of nimesulide and nifedipine, intrauterine pressure, frequency and amplitude of uterine contractions decrease, and the pain stops after approximately 30 minutes. The selective b-stimulant terbutaline relieves muscle activity, reduces intrauterine pressure, and relieves pain. Partusisten and orciprenaline reduce the frequency and amplitude of uterine contractions, the latter inhibiting contractions caused by potassium, oxytocin, and vasopressin, effectively reducing the content of prostaglandins E2 and F2a. Treatment of secondary dysmenorrhea.
As for secondary dysmenorrhea, most researchers consider it to be a consequence of organic disorders in the female reproductive system - developmental anomalies, inflammatory diseases of the pelvic organs, endometriosis, submucous uterine fibroids, etc. Accordingly, the choice of therapeutic agents is determined by the nature of the main pathological process. If organic pathology of the pelvic organs is detected, treatment of secondary dysmenorrhea should be aimed at eliminating the identified lesions. Studies by many authors have found an increase in the synthesis of endogenous PGs in salpingoophoritis and endometriosis, which indicates the pathogenetic significance of PG hyperproduction and justifies the use of antiprostaglandin drugs for secondary dysmenorrhea. For chronic inflammatory diseases of the pelvic organs, endometriosis, malformations, and uterine fibroids, therapeutic hysteroscopy and laparoscopy are used. Among surgical interventions for secondary algodismenorrhea, presacral sympathectomy is most often of historical interest. Quite often, bougienage of the cervical canal is performed; hysterectomy, without a doubt, is a measure of despair, especially since the pain often remains after it. When curing a somatic disease, persistent pain syndrome is possible: residual effects of damage to the nerve trunks, ischemic changes, adhesive processes, changes in the functional state of the nodes of preganglionic autonomic innervation, in which persistent morphological changes are observed, as well as psychogenic fixation of the pain syndrome. Therefore, when treating secondary dysmenorrhea, it is necessary to eliminate pain. Therefore, when treating secondary dysmenorrhea, it is necessary to eliminate pain. In the search for an effective remedy for pain, one should not forget about the central regulation of the pathological symptom complex by both the hypothalamic-pituitary system and the cerebral cortex. In this sense, the effectiveness of psychotherapy, tranquilizers, auto-training and acupuncture is known. It must also be remembered that if the nature of the disease is unspecified, accompanied by pain, long-term use of analgesics and tranquilizers is contraindicated, since this erases not only pain sensitivity, but also the clinical picture, for example, in acute processes in the abdominal cavity. Thus, menstrual pain, the cause of which is not organic lesions, is considered as primary dysmenorrhea, and those associated with lesions or diseases of an organic nature - as secondary dysmenorrhea. Due to the fact that non-steroidal anti-inflammatory analgesics sometimes reduce the severity of some symptoms associated with organic pathology, it may be difficult to make a diagnosis. If the doctor believes that the pain is caused only by menstruation, a thorough history should be taken to identify diseases of the gastrointestinal tract, urological and other diseases. Treatment should be primarily aimed at identifying endometriosis, uterine fibroids, adenomyosis and salpingitis. If the prescribed treatment leads to complete disappearance of symptoms, no further studies are required. If it does not give positive results, laparoscopy should be performed. Many women have minimal symptoms and do not need such tests. However, if an organic pathology is suspected or severe symptoms (the patient is forced to remain in bed and not go to work for several days every month), the only way to make a correct diagnosis is to perform laparoscopy. If laparoscopic examination reveals the initial symptoms of endometriosis, then heterotopias can be subjected to coagulation directly during this operation. The diagnosis of submucous uterine fibroids can be made by hysteroscopy or
Primary dysmenorrhea
This is a functional disease, manifested by a typical clinical picture without pathologies of the reproductive system. It usually appears at a young age, several years after the start of the first menstruation. As a rule, the pain is minor at first, but the condition worsens every year. The lower abdomen begins to hurt on the first day of menstruation, or a few hours before it begins. The duration of discomfort varies from 1 to 3–4 days. The reasons for this condition are not exactly known, however, there are suggestions that primary dysmenorrhea
occurs due to the action of biologically active substances produced in dead endometrial cells - prostaglandins E2 and E2-α.
Kinds
There are primary and secondary dysmenorrhea. The first occurs when during the examination it is not possible to detect any pathological changes in the female body, i.e. there are no serious prerequisites for its development.
Primary dysmenorrhea can occur immediately during the first menstruation or several years after that. Initially, it usually does not cause significant disturbances in well-being, since the pain is usually mild and aching in nature. This is normally tolerated by girls and is not perceived as a deviation from the norm. But after a few years, with primary dysmenorrhea, the pain syndrome may intensify, and the duration of its persistence increases. Over time, other symptoms appear.
Primary dysmenorrhea is rarely present on its own. Very often, when conducting a comprehensive examination of a girl, other pathologies are discovered, in particular:
- mitral valve prolapse;
- vegetative-vascular dystonia;
- visual impairment (myopia, myopathy);
- scoliosis;
- flat feet.
Thus, primary dysmenorrhea may be the result of neurological disorders that occur against the background of the development of spinal pathologies. In such situations, there is infringement of the spinal root in the lumbar spine, which leads to disruption of the conduction of nerve impulses to the uterus. The consequence of this is the appearance of characteristic pain, but subsequently such disorders can cause the development of serious organic changes in the organs innervated by the pinched nerve. Therefore, in such situations, it is recommended to consult a chiropractor.
Secondary dysmenorrhea is diagnosed when pathological changes are detected, which are the cause of pain on the eve of and during menstruation. Most often, it appears in women aged 25-30 against the background of the development of endometriosis, inflammatory diseases of the internal genital organs, and the formation of adhesions. In such situations, dysmenorrhea becomes only one of the manifestations of a developing disease and to eliminate it, it will be necessary to eliminate the existing pathology.
Secondary dysmenorrhea
It is caused by pathological changes in the pelvic organs, such as developmental anomalies, inflammatory processes, etc. The presence of an intrauterine device may also be a cause. Most often, clinical manifestations of the secondary process appear after 30–35 years. Pain and other symptoms of dysmenorrhea usually begin 2-4 days before the start of menstruation and may continue even after it ends. The causes are disturbances in blood flow to the pelvic organs, as well as stretching of the walls of the uterus, myometrial spasms and pathological changes in tissue. Secondary dysmenorrhea
can be distinguished from the primary one by the presence of concomitant symptoms of the main pathology, as well as during examination by a gynecologist.
Types of dysmenorrhea
Diagnosis and treatment
As with the treatment of any other disease, the accuracy of the diagnosis for dysmenorrhea plays a key role. If this is a secondary form, then it is necessary to focus on finding the causes that led to the cyclical occurrence of pathological conditions. If patients complain of severe menstrual pain and other symptoms associated with dysmenorrhea, it is necessary to prescribe a comprehensive examination. It includes:
- clinical blood and urine analysis;
- biochemical blood test;
- gynecological examination;
- Ultrasound of the pelvic organs, abdominal cavity;
- tests for tuberculosis (to identify or exclude tuberculosis of the pelvic organs).
If necessary, the doctor can prescribe consultations with related specialists, as well as additional examinations according to indications:
- hysteroscopic;
- electroencephalographic;
- laparoscopic.
The data obtained during the examination is analyzed by the attending physician. He develops a treatment strategy, during which it is possible to prescribe clarifying examinations and tests. Thus, a doctor can prescribe, for example, diclofenac for diagnostic and treatment purposes for several days, which makes it possible to distinguish primary dysmenorrhea from secondary dysmenorrhea by the nature of changes in the pain syndrome, in particular those occurring against the background of endometriosis. If, when taking the drug, menstrual pain quickly subsides in the first days, then the likelihood of primary dysmenorrhea increases. If the pain remains, gradually weakening by the fifth day, then this picture is typical for endometriosis. When testing with non-steroidal anti-inflammatory drugs, which include diclofenac, the patient may not experience any dynamics of change in the nature of pain. This indicates the presence of psychosomatic problems, as well as genital defects.
Nonsteroidal anti-inflammatory drugs also find practical use in the symptomatic treatment of primary dysmenorrhea. Their action is directed against the synthesis of prostaglandins, the excessive production of which leads to pain. The effectiveness of these drugs in the treatment of primary dysmenorrhea reaches 80%. Painful attacks are well relieved by No-spa, nonspecific analgesics, as well as drugs containing magnesium and synthetic GnRH (gonadotropin-releasing hormone).
In the treatment of secondary dysmenorrhea, diclofenac and similar drugs are also used in the fight against pelvic inflammation. The side effects of these drugs must be neutralized with additional drugs, for example, nimesulide, etc. The doctor prescribes preventive and therapeutic drug regimens individually, taking into account the medical history of the particular patient.
Antispasmodics are widely used to relieve spastic pain. In this case, they are preferable to analgesics (including non-narcotic ones), since they do not erase the symptoms of organ diseases, while relieving or preventing spasms of smooth muscles.
One of the pharmacological methods for treating dysmenorrhea is hormone therapy. In particular, two types of drugs are used: combined oral contraception and progesterone drugs. Birth control pills are not prescribed to women trying to become pregnant. In this case, hormone therapy is carried out with progesterone preparations, or rather, containing its derivatives.
Hormonal therapy allows you to control the production of prostaglandins, reduce the contraction of myometrial muscle cells, thus eliminating the main cause of pain.
Psychosomatics plays a certain role in the treatment of menstrual pain. A number of studies show the positive effects of placebo. It is possible that psychotherapy and psychotropic drugs may be effective for the treatment of dysmenorrhea. But for now this direction is at the research stage.
Symptoms of dysmenorrhea
The main symptom is pain in the abdominal area, mainly lower. This condition is called algomenorrhea. The pain can be aching, pulling or cramping. Often there are changes in the general condition, manifested in the form of weakness, dizziness, nausea, bloating, increased body temperature and loss of appetite. Such symptoms of dysmenorrhea can be severe, which significantly impairs the physical and mental state of a woman. Approximately 15% of women are forced to take sick leave in the first 1–3 days of menstruation.
With secondary dysmenorrhea, the above symptoms are accompanied by signs of the underlying pathology that caused the cycle disruption.
What is dysmenorrhea
Dysmenorrhea is not considered a disease in the truest sense of the word. This term refers to a certain condition of the female body that develops during the onset of menstruation and a couple of days before it. Often, the concept of dysmenorrhea includes other menstrual cycle disorders, in particular changes in the amount of bleeding, cycle irregularity, and others.
Today, more than 70% of women suffer from dysmenorrhea, among whom the vast majority are young girls, in whom 1-3 years have passed from the first menstruation to the appearance of signs of dysmenorrhea. Its presence can have a significant impact on the quality of life and even lead to loss of performance during menstruation.
Expert Opinion of a Doctor
Almost every woman in her life has encountered such complaints before the onset of menstruation, such as: bloating, anxiety, engorgement of the mammary glands, tearfulness, depression, fatigue, irritability, enlarged veins - all this is nothing more than a manifestation of premenstrual syndrome.
Mgdesyan Knarik Karlenovna
Obstetrician-gynecologist, gynecologist-endocrinologist
Experience: 24 years
Ask a Question
Previously, the term “algodismenorrhea” existed, but it was abandoned, since it reflected only the pain of menstruation and indicated serious changes in the body.
According to research, dysmenorrhea is more common among women whose close relatives had this disorder, as well as those who regularly engage in heavy physical work and experience stress.
Diagnosis of dysmenorrhea
Typically, diagnosing dysmenorrhea is not difficult, since women independently describe all clinical manifestations. The presence of secondary dysmenorrhea can be detected by undergoing an examination by a gynecologist and a series of laboratory and instrumental tests.
The most informative in terms of diagnosing dysmenorrhea are:
- laboratory determination of hormone levels in the blood in different phases of the cycle;
- ultrasonography;
- endoscopic examination - colposcopy, hysteroscopy;
- computed tomography or magnetic resonance imaging.
Laboratory determination of hormones in different phases gives the doctor an idea of the regularity of the cycle, the functioning of the ovaries, hypothalamus and pituitary gland, and thyroid gland.
Diagnostics
Directly diagnosing the presence of dysmenorrhea is not difficult for a gynecologist. Diagnostics is aimed at identifying the causes of pain and other disorders during menstruation. For this purpose, the doctor examines the patient, paying attention to body features and psycho-emotional state. An examination is required on a gynecological chair with manual examination of the uterus. In the presence of pathological changes, the gynecologist may note an increase in its size and the presence of infiltration in the pelvis.
For primary prevention and diagnosis, it is important to take a general and biochemical blood test. But in our clinic you can also learn in more detail about the composition of your body and the state of the vascular system, which is involved in the blood supply to internal organs, skeletal muscles, and the brain. Our experienced doctors will explain the data obtained to you in detail. Bioimpendansometry calculates the ratio of fat, muscle, bone and skeletal mass, total fluid in the body, and basal metabolic rate. The intensity of recommended physical activity depends on the state of muscle mass. Metabolic processes, in turn, affect the body's ability to recover. Based on the indicators of active cell mass, one can judge the level of physical activity and nutritional balance. This simple and quick test helps us identify disturbances in the endocrine system and take the necessary measures. In addition, it is also very important for us to know the condition of blood vessels for the prevention of diseases such as heart attacks, hypertension, heart failure, diabetes and much more. Angioscan allows you to determine such important indicators as the biological age of blood vessels, their stiffness, stress index (which indicates heart rate), and blood oxygen saturation. Such screening will be useful for men and women over 30, athletes, those undergoing long-term and severe treatment, as well as everyone who monitors their health.
For a full examination of a woman, she may be prescribed:
- UAC and OAM;
- blood test for the level of major sex hormones;
- Ultrasound of the pelvic organs;
- MRI.
With dysmenorrhea, disturbances in the functioning of the endocrine system, as well as the autonomic nervous system, are often detected.
Based on the data obtained, the doctor can make a diagnosis and understand what caused dysmenorrhea, and therefore prescribe effective treatment.
Doctor's opinion
During an ultrasound examination, you can see an incorrectly located uterus, tumors, adhesions, and a displaced helix.
Hysteroscopy helps diagnose endometriosis, endometrial polyps and other disorders of the lining of the uterus. CT and MRI are prescribed in doubtful cases, mainly for differential diagnosis. — Barakhoeva Zarema Bekhanovna Reproductologist, obstetrician-gynecologist, Ph.D.
If a tumor is suspected, a biopsy and pathomorphological examination of the obtained material is indicated. Such a diagnosis of dysmenorrhea will make it possible to make a correct final diagnosis, practically eliminating the possibility of error.
Diagnostic methods
Causes of occurrence - anamnesis
There are risk factors for the development of this pathology, which include:
- Start of menstruation at an early age.
- Anomalies of the development of the uterus and appendages.
- Habitual intoxication (smoking, alcohol, drugs).
- The presence of chronic diseases (endometriosis, fibroids).
- Constant stress.
- Physical inactivity.
- Low socio-economic status.
Also an important factor is the presence of a family history. The likelihood of developing dysmenorrhea increases significantly in the presence of this pathology in close female relatives.
Treatment of dysmenorrhea
Regardless of the reasons and the age at which the diagnosis was made, dysmenorrhea requires treatment, first of all, to alleviate the woman’s general condition, as well as to prevent disability. Treatment of primary dysmenorrhea involves taking medications aimed at blocking the action of prostaglandins. These include non-steroidal anti-inflammatory drugs such as Ibuprofen, Naproxen, Diclovit and Nimesulide. These medications also have an analgesic effect. Combined oral contraceptives have a good effect. In case of significant pain, it is possible to take analgesics or antispasmodics (Analgin, Sedalgin and No-shpa)
Sometimes a preventative course is prescribed - taking anti-inflammatory drugs 3-5 days before the onset of menstruation.
The duration of such treatment is 3 menstrual cycles. Treatment of dysmenorrhea as a secondary phenomenon is aimed at treating the underlying gynecological pathology that caused this manifestation. Analgesics are prescribed to eliminate pain and alleviate the general condition. The choice of drug, dosage and methods of use are determined by the doctor after interviewing and examining the patient.
Particular attention is paid to physiotherapeutic procedures. Relaxing baths with extracts of pine needles, mint and lemon balm normalize the functioning of the central nervous system. A course of 10–15 baths is enough to stabilize the central nervous system. Electrosleep has a similar effect. Ultratonotherapy improves blood supply to internal organs, normalizes the tone of blood and lymphatic vessels, and improves metabolism. Sunbathing also has a noticeable effect. Sun rays improve the functioning of the immune system, activate regenerative processes, and normalize metabolism. The procedures are recommended to be taken in the morning and evening hours. Electrical stimulation of the cervix allows you to regulate the functioning of the hypothalamic-pituitary system by activating peripheral receptors and triggering reflex reactions. If necessary, the patient is recommended psychotherapy sessions. These can be both group and individual sessions, the type of which is selected by the psychotherapist.
Severity of dysmenorrhea
It is customary to distinguish several degrees of severity of this menstrual cycle disorder.
Dysmenorrhea of the 1st degree involves the presence of pain, which only periodically can lead to a decrease in a woman’s activity. There are no symptoms associated with a general feeling of well-being.
Dysmenorrhea of the 2nd degree is characterized by a more pronounced pain syndrome, the relief of which requires the use of painkillers. A woman’s well-being noticeably worsens during menstruation, which affects her performance and in some cases forces her to change her usual rhythm of life.
Dysmenorrhea of the 3rd degree is characterized by severe pain, which is practically not relieved with the help of analgesics. The woman has nausea, headaches, weakness and other vegetative symptoms. As a rule, the patient has to change her usual rhythm of life due to a significantly deteriorated state of health and a pronounced decrease in performance.
Causes
Dysmenorrhea can result from a number of factors affecting women's health and lifestyle.
The causes of discomfort may be:
- Mechanical properties - associated with injuries or anomalies of the genitourinary system and leading to abnormal outflow of menstrual blood from the uterine cavity (atypical location of the uterus, abnormal development of the cervix, etc.)
- Endocrine in nature - a disruption in the process of synthesizing hormones (prostaglandins) and, as a result, cramps before and during menstruation.
- Anatomical. Due to the underdevelopment of the system involved in the removal of blood mucus, muscles and nerve endings do not stretch properly when blood accumulates, resulting in pain.
- Neuropsychogenic type - when the sensitivity threshold is reduced (with certain mental or nervous diseases).
Dysmenorrhea in women may be associated with contraception using an intrauterine device. Pain often occurs when the contraceptive intrauterine device is placed incorrectly or when there is individual intolerance to such contraceptives.
Dysmenorrhea can become a “concomitant” factor in a number of diseases of the genitourinary system of women.
Repeated appointment and treatment control
After the course of treatment, the patient must come for examination and evaluation of the results. If after or during the course the pain in the lower abdomen during menstruation does not go away, it means that the course of treatment is adjusted or completely changed. It may be necessary to undergo further examination.
The results and timing of treatment for lower abdominal pain during menstruation and recovery are always strictly individual and depend on the complexity and severity of the disease. If there are diseases that are sexually transmitted, then treatment and prevention are prescribed to the partner.
What is prescribed for pain during menstruation after examination and diagnosis?
Treatment, of course, is built according to an individual plan, according to the results of diagnostics and tests, as well as the collected medical history. If severe pain in the lower abdomen during menstruation is secondary dysmenorrhea, the doctor will look for the root cause, the underlying disease that caused the menstrual irregularities.
As a rule, treatment consists of a whole range of medicinal and non-medicinal measures:
- herbal medicines and a number of antispasmodics (for the primary form of the disease and its mild to moderate severity);
- if pain in the lower abdomen during menstruation is provoked or appears together with infectious and inflammatory diseases caused by viruses and bacteria, then antiviral drugs can be prescribed;
- if the disease has relatively mild psychogenic causes, then reflexology (drugs with a weak psychostabilizing effect) and, possibly, consultation with a psychologist are prescribed;
- in complex treatment, it is also possible to prescribe drugs and medications that reduce spasms and serve as an analgesic;
- it is possible to prescribe hormonal contraceptives, etc.
For successful treatment of lower abdominal pain during menstruation, physiotherapy is also prescribed in the form of:
- normalization of nutrition;
- rational management of time for work and rest;
- sufficient time to sleep;
- sufficient physical activity;
- reducing and reducing stressful and psychological situations, etc.
Contraindications will include individual intolerance to the components of treatment, allergic reactions and the characteristics of your body. You should also avoid additional stressful situations and anything that somehow provokes illness these days.