Eczema is a chronic skin pathology that manifests itself in the form of foci of inflammation on the body, arms, legs and head. Rashes that form on the skin go through several stages of development: primary redness, dense nodules that transform into blisters, then weeping erosions form, which during the healing process are covered with a scab (the so-called “crust”). The last stage is peeling. Against the background of eczema, secondary purulent infections often develop. If left untreated for a long time, cosmetic defects of the skin may appear in patients of all ages.
Effective treatments for eczema
Cryotherapy
NeoGen procedure
Plasma therapy
One of the fairly common skin diseases is eczema. It is an inflammation accompanied by redness, itching and the appearance of tiny blisters with liquid. It is the latter that explains the name of the disease: such bubbles resemble the boiling of water, from the Greek eczeo means “to boil.”
According to statistics, up to 2% of the world's population suffers from eczema. And in the practice of dermatologists, such pathology occurs in almost 40% of all skin diseases. Most often, patients come with the problem of the appearance of foci of inflammation on the arms, legs, body and head. The rash goes through several stages of development, over time developing from simple redness into weeping erosion and severe peeling. Against the background of such pathology, secondary purulent infections often develop. Without treatment, noticeable cosmetic defects remain on the skin that do not go away over time.
Let's figure out why eczema occurs, how to suspect its development and how such a pathology is treated.
Questions and answers
Are there differences in the causes of eczema on the hands and eczema on the feet?
The appearance of foci of inflammation on the extremities is in most cases associated with traumatic factors or exposure to aggressive chemicals. The formation of vesicles or weeping on the body is often the result of allergic reactions and systemic pathologies identified in patients.
What are the main clinical recommendations for diagnosed eczema?
A patient with a confirmed diagnosis of eczema should discuss with a dermatologist the advisability of consultations with other doctors: endocrinologist, allergist, gastroenterologist. Their use can reduce the frequency of exacerbations of the disease and reduce the intensity of reactions to factors that provoke the inflammatory process.
Do patients with chronic eczema need to take any medications regularly?
Drug and hardware treatment along with courses of physiotherapy are prescribed during periods of exacerbations. After relief of acute symptoms of the disease, the patient does not need to systematically take medications. A significant role during this period is played by the child or adult’s compliance with the recommendations of the attending physician and preventive measures.
Causes of the disease
Until now, doctors cannot unequivocally answer the question about the causes of the development of eczema in adults and children. Most experts agree that the disease develops as a result of the complex influence of endogenous factors (for example, genetic predisposition) and exogenous factors (occupational, etc.). Simply put, external factors most often include various allergens that affect the body constantly or for a long time. To internal, endogenous – genetic predisposition. It has been proven that if there is a person with eczema in the family, the risk of the disease in relatives increases significantly. If one of the parents (mainly the mother) is ill, the risk of developing eczema in a child is approximately 40%; if both parents are ill, it is almost 60%
The most common factors that provoke eczema:
- chronic allergies;
- disturbances in the functioning of the endocrine system;
- psycho-emotional triggers.
They also additionally identify factors that can weaken the body’s immunity and thereby provoke the development of eczema. This:
- chronic inflammatory processes;
- secondary immunodeficiencies;
- diseases of the digestive system;
- foci of chronic infection in the body.
Among the possible causes of eczema are psychosomatics: constant stress, various disorders of the autonomic system, anxiety and depression. Patients often exhibit functional changes in the activity of the central nervous system, a predominance of the activity of unconditioned reflexes over the activity of conditioned ones, as well as an imbalance between the activity of the sympathetic and parasympathetic parts of the autonomic nervous system.
Types of eczema
Experts distinguish the following types of pathology:
- True or idiopathic. The patient has symmetrical foci of inflammation and pigmentation, and symptoms appear in exposed areas of the skin. Over time, erosions develop on which exudate accumulates. As healing occurs, peeling of the skin occurs.
- Microbial. This form of pathology develops against the background of traumatic injuries, fungal, viral and bacterial infections. Infiltrate often accumulates under the skin. Failure to comply with personal hygiene rules provokes an accelerated spread of lesions throughout the body.
- Seborrheic. This pathology is characterized by damage to skin areas on the scalp. The affected areas have typical redness, peeling and itching. In some cases, the course of the disease is complicated by swelling and weeping cracks.
- Professional. It occurs due to the patient’s constant contact with various allergens: dust, chemicals, cleaning products, etc. Very often small vesicles appear in various parts of the body.
- Getting wet. At the beginning of this disease, pink spots of various shapes and sizes appear on the skin, swelling and the formation of subcutaneous exudate are also observed. Next begins the cortical stage and exfoliation. The main feature is the presence of a rash at all stages of the disease.
- Dyshidrotic. This pathology affects the sweat glands of the feet and hands and is characterized by the formation of serous blisters and seasonal exacerbation. As a rule, there are pronounced vesicles with a dense shell. There is severe itching and peeling.
- Allergic. It occurs as a result of the body's hypersensitivity to external and internal stimuli. Accompanied by rashes, itching and dry skin. Large crusts form in place of the opening bubbles, sometimes the process is accompanied by a burning sensation.
Prevention of eczema on fingers
To prevent the development of the disease or prevent the development of repeated relapses, it is necessary:
- maintain immunity levels.
- exclude allergens.
- adhere to the rules of personal hygiene.
- use protective equipment when in contact with chemicals and other substances that contain aggressive components.
- lead a healthy lifestyle - avoid hypothermia, give up bad habits.
- use hypoallergenic cosmetics and detergents.
- follow the doctor's instructions.
- treat concomitant diseases.
- avoid hypothermia.
- exclude allergens.
- pay increased attention to personal hygiene.
By following these simple preventative tips, you can avoid illness or speed up your recovery.
Stages of the disease
If we talk about the features of the course of the disease, then there are usually three stages of its development:
- Spicy. It is characterized by the appearance of vesicles on swollen skin, point erosions with weeping, serous crusts, etc. The rashes are multiple in nature.
- Subacute. This stage is characterized by erythema, redness and scaling.
- Chronic. It is characterized by infiltration and strengthening of the “skin pattern”, the appearance of pigmentation.
Symptoms of eczema
Depending on the cause of the disease and the location of the inflammation, symptoms can vary significantly. Most often, patients experience the following manifestations of skin eczema:
- At the erythematous stage, red inflammatory spots appear, which gradually merge with each other.
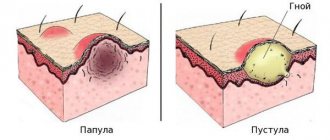
- At the papular stage, bright red nodules with clear boundaries are formed.
- At the vesicular stage, bubbles with transparent contents appear.
- At the stage of weeping, the bubbles open, point erosions are formed with the release of exudate.
- At the cortical stage, grayish-gray crusts are found, under which the skin heals.
- At the peeling stage, crusts and scales are removed from the surface of the skin.
Symptoms of the disease go away with the elimination of provoking factors. However, the healed area of skin has an uneven color and dense texture.
What other symptoms may indicate the development of eczema:
- The scaly layer at the border of the scalp. Develops with seborrheic eczema. At the initial stage, it manifests itself as single yellowish nodules that quickly grow. Subsequently, a scaly layer forms along the border of the hair.
- Round rashes on hands. Appear in almost 80% of cases of eczema development. At the initial stage they have a rounded shape, but over time they lose it.
- Rashes with clear edges. Most often found on the legs. They can be seen with varicose veins, the rashes have a round shape and pronounced borders.
Symmetrical rashes on the body. They are located all over the body and often peel off. At the initial stages they look typical - they are bubbles with liquid, later areas of thickened skin with severe peeling appear.- Callus-like rashes on the palms. Such formations, especially in places atypical for calluses, also indicate eczema. Bubbles form, but due to the thick skin they may not open.
- Bubbles in the armpit with a hair in the center. Rashes with a hair in the center are a sign of sycosis - damage to the hair follicles. As a rule, such rashes are accompanied by itching and redness.
- Lumps on the face and hands. Such formations do not ooze or crust, and often appear on the face.
- Itchy redness on the arms and legs. Indicate true or microbial eczema. Accompanied by multiple vesicles.
- Suppuration around the wounds. With the development of microbial pathology, purulent crusts and skin hyperemia appear.
The symptoms of eczema are often similar to atopic dermatitis. However, it is worth understanding that pathologies also have significant differences. Dermatitis usually occurs in childhood, while eczema is found in adults and even elderly patients. Another difference is that the first pathology is most often localized on the elbows and knees, neck and face, while eczema can be located on any area, but more often on the hands and legs. Dermatitis occurs suddenly and often disappears. Eczema appears regularly and is often the immediate result of exposure to a specific allergen.
Diagnosis of eczema
The diagnosis is made based on examination and questioning of the patient. In some cases, additional tests may be prescribed to differentiate eczema from other skin diseases. With true eczema, the clinical picture of the disease is typical. In other cases, symptoms may be similar to atopic dermatitis, toxicerma and allergic contact dermatitis.
The diagnostic process may include:
- general blood analysis;
- tissue scraping for examination under a microscope;
- allergy tests to identify the source of allergies;
- histological examination of tissues.
Treatment is prescribed only after confirmation of the diagnosis and determination of the existing type of pathology.
Features of treatment
The key to treating eczema is to identify and minimize triggers. In addition, systemic or local therapy is prescribed, as well as various physiotherapeutic procedures:
- Systemic therapy. It is based on taking antihistamines, which help prevent an acute allergic reaction. Sedatives, glucocorticosteroids and a number of hormonal drugs are also used.
- Local therapy. May include the use of retinol ointment, anti-inflammatory and antiseptic agents. Therapy is selected taking into account the identified form of eczema and the causes of its occurrence. For example, treatment for a virus or fungal infection may be required.
- Physiotherapy. As a rule, it includes ozone therapy, magnetic therapy and laser therapy. In difficult cases, it is possible to treat eczema lesions using cryotherapy. Medicinal and mud baths, exposure to ultraviolet radiation, etc. are often prescribed.
Preventive measures
Diet and lifestyle play an important role in preventing the development of new exacerbations. The diet should exclude any foods that can trigger allergic reactions. Typically this is:
- red berries;
- citrus;
- Fish and seafood;
- chocolate;
- dairy products.
Patients are also advised to give up alcohol and smoking.
Personal hygiene is also important. If eczema of the feet, legs, arms and face develops, it is recommended to avoid scented soaps. Water-based creams can be used to moisturize the skin.
And most importantly, improper treatment of skin diseases can trigger eczema. This means you should not self-medicate. If any rashes and redness appear, do not delay a visit to a dermatologist, because this can be the key to a quick and successful recovery.
If you are faced with the symptoms of eczema and do not know how to get rid of such a disease, then the dermatologists of our KallistoMed clinic are ready to help in this matter. We will be waiting for you at the reception - sign up using the website or by calling the numbers provided!