ICD-10 code: N94 - Pain and other conditions associated with the female genital organs and the menstrual cycle (N94)
Modern devices are equipped with a special warning system, which draws the owner’s attention to the fact that somewhere there is a malfunction.
In the complex human body, the alert function is extremely finely tuned. As soon as damage occurs at any point, the alarm siren immediately goes off - pain.
This is certainly an important and useful mechanism, because it protects us from dire consequences by encouraging us to take action. But... if in the device, by pressing a special reset button, we can turn off the alarm signal and at a time convenient for us to begin eliminating the breakdown, then in the body there is no such button.
Pain syndrome, being one of the manifestations of the protective mechanism of the human body, is the scourge of humanity. Having fulfilled its alert function, it does not turn off on its own, causing suffering and creating problems for its owner.
This is the most important signal about tissue damage and the development of a pathological process, a constantly operating regulator of homeostatic reactions, including their higher behavioral forms. However, this does not mean that pain has only protective properties.
Under certain conditions, having played its informational role, pain itself becomes part of a pathological process, often more dangerous than the damage that caused it.
Thus, a useful defense mechanism turns into a scourge of humanity.
Therefore, painkillers are not just an attempt to make life more comfortable, but a vital tool in preventing the development of other serious disorders.
Algodismenorrhea classification ICD-10
N94.0 - Pain in the middle of the menstrual cycleN94.1 — Dyspareunia (Excludes: psychogenic dyspareunia (F52.6)N94.2 — Vaginismus (Excludes: psychogenic vaginismus (F52.5)N94.3 — Premenstrual tension syndromeN94.4 — Primary dysmenorrheaN94.5 — Secondary dysmenorrheaN94.6 — Dysmenorrhea, unspecifiedN94.8 — Other specified conditions related to the female genital organs and the menstrual cycleN94.9 — Conditions related to the female genital organs and the menstrual cycle, unspecifiedAlgodismenorrhea - what is it?
Doctors often have to deal with complaints of abdominal pain. In 30% of cases, abdominal pain is spastic in nature. A striking example is algodismenorrhea.
The cause of algodismenorrhea is spasm of the smooth muscles of the uterus. It should be noted that algodismenorrhea is very common in the practice of obstetrician-gynecologist.
Painful menstruation occurs in 31-52% of women aged 14-44 years, and in about 10% of them the pain is so intense that it interferes with the ability to work, forcing them to interrupt work or other activities. That is why leading European experts consider algodismenorrhea not only as a medical, but also as a social problem.
Video reviews of consultations and services of a gynecologist in our clinic
Ekaterina, 35 years old. Clinical examination
Katerina V. - pregnancy management
Irina, 25 years old, Tula
Anastasia, 30 years old - treatment by a gynecologist, pregnancy management
.
Gynecologists at our clinic
Gaponova Natalia Mikhailovna
Obstetrician-gynecologist, ultrasound diagnostics doctor
Main areas of practical activity: treatment of infectious and inflammatory diseases of the pelvic organs, ovarian dysfunction, menstrual irregularities, correction of menopausal disorders, minimally invasive treatment methods in gynecology, intimate surgery. Pregnancy management, female infertility.
Kulik Svetlana Vladimirovna
Obstetrician-gynecologist, ultrasound diagnostics doctor
In 2000, she graduated from the medical faculty of the Volgograd Medical Academy. Has additional professional retraining in gynecology-endocrinology, operative hysteroscopy, ultrasound diagnostics in obstetrics and gynecology.
Work experience in the specialty is 12 years.
Ivanova Natalya Vladimirovna
Obstetrician-gynecologist, doctor of the highest category, candidate of medical sciences
In 1983 she graduated from Voronezh State Medical Institute named after. N.N. Burdenko. Areas of professional interests: recurrent miscarriage, plastic surgery of the labia minora and majora, vaginal restoration after traumatic childbirth.
32 years of experience in the specialty.
Kavun Irina Sergeevna
Obstetrician-gynecologist, ultrasound diagnostics doctor
In 1987 she graduated from the medical faculty of the Yaroslavl State Medical Institute. Doctor of the highest category. Has professional retraining in ultrasound diagnostics in obstetrics and gynecology, surgical obstetrics and gynecology, endoscopy.
Work experience in the specialty is 25 years.
Smirnova Lyudmila Evgenievna
Obstetrician-gynecologist. Candidate of Medical Sciences. Doctor of the highest category.
Engaged in the diagnosis and treatment of diseases of the female reproductive system and pregnancy management. He is engaged in scientific work.
Work experience 16 years.
Buga Marina Vladimirovna
Obstetrician-gynecologist, ultrasound diagnostics doctor
In 1987 she graduated from the medical faculty of the Kazan State Medical Institute. Has retraining in gynecology-endocrinology, ultrasound diagnostics in obstetrics and gynecology. Specializes in the treatment of diseases of the female reproductive system.
Work experience in the specialty is 25 years.
Clinical manifestations
The leading clinical manifestation of algodismenorrhea is cramping pain in the lower abdomen and in the sacral region. Possible irradiation to the groin, anus and thigh area.
Pain syndrome can appear a few days before menstruation, appear throughout the entire period, and even continue for several days after menstruation.
During this period, a woman may experience irritability, depressive symptoms, decreased performance, and drowsiness.
Sometimes psycho-emotional disorders manifest themselves in the form of anorexia or bulimia, odor intolerance, etc.
Algodismenorrhea can also be accompanied by autonomic disorders. Disorders from the gastrointestinal tract are common, which manifest themselves as nausea, vomiting, bloating, heartburn, dry mouth, etc. Urination may also become more frequent.
From the side of the autonomic-vascular system, disorders can lead to fainting, headaches, heart rhythm disturbances and pain in the heart, feelings of coldness and numbness in the limbs, etc.
In addition, disruptions in the functioning of the endocrine system occur, which manifests itself in the form of edema, polyuria, severe weakness, sweating, etc.
The pathology is characterized by increased tone of the sympathetic-adrenal system, and sometimes the parasympathetic.
An allergic component associated with increased sensitivity to one's own sex hormones is often observed. After a spastic attack, an increased content of eosinophils is observed in the blood, against the background of leukopenia and lymphocytosis.
Thus, it can be argued that algodismenorrhea affects a number of vital processes and leads to systemic disturbances in the functioning of the body.
Pathogenesis
Regardless of the etiology, the pathogenetic process is based on excessive synthesis of prostaglandins (PGs).
It is also worth considering that PGs increase the sensitivity of nerve fibers, which is caused by an increase in pressure in the uterine cavity with excessive contractility of the myometrium.
Due to a sharp increase in the production of PGs (primarily E2a and E2), they accumulate in the endometrium and cause platelet aggregation, vasoconstriction, irregular contractions of myometrial fibers and lead to the development of endometrial ischemia.
Thus, the mechanism of pain during algodismenorrhea is correlated with the processes during acute myocardial ischemia - arterial spasm and bleeding of muscle tissue.
The synthesis of PG is controlled by cyclooxygenase (COX), the activity of which, in turn, is regulated by sex hormones - estrogens and progesterone.
Diagnostics
Bacterial vaginosis
To diagnose algodismenorrhea, as well as to identify other gynecological pathologies, physical, laboratory and instrumental methods are used. A correctly collected anamnesis and information about the history of the development of the disease play a vital role in the diagnosis of algodismenorrhea.
Of the laboratory methods, a standard set is used: UAC, OAM, BAK. Next, an instrumental examination is carried out. The most informative method is ultrasound.
If indicated, hysteroscopy and laparoscopy can be performed to detect small foci of external endometriosis, varicose veins of the pelvic organs and ruptures of the broad ligaments.
Diagnosis of pathology is based on clinical manifestations, anamnestic data and the results of laboratory and instrumental studies. During the examination, the doctor pays attention to such signs as the presence of acne and stretch marks on the skin, excess hair growth, and manifestations of connective tissue dysplasia. The mammary glands are examined. In adolescent girls, pubertal development assessment (BMI, waist circumference) and vaginal-abdominal examination are performed.
Vaginal discharge
Laboratory diagnostic methods:
- microscopy of a smear from the vagina and cervical canal;
- cytological examination of a smear from the endo- and exocervix for atypical cells;
- blood test to determine the level of sex hormones (estradiol, progesterone);
- blood serum analysis for the content of microelements (Ca, Fe, Mg, etc.);
- determination of the level of tumor marker CA-125 in the blood (used in the diagnosis of endometriosis);
- if you suspect a secondary nature of algodismenorrhea associated with inflammatory processes in the organs of the female reproductive system - examination for STIs,
- general clinical blood test, study of the level of C-reactive protein in the blood plasma.
If necessary, consultation with other specialists is possible.
About algodismenorrhea
Algodysmenorrhea is a menstrual disorder that accompanies painful sensations during the first days of menstruation in the lower abdomen, lower back and sacral area, occurring against a background of general malaise.
Most often, cramping or aching pain is characteristic. Weakness, sweating, nausea, headaches, swelling, dizziness, bowel irregularities and decreased performance are likely. There are two types of algodismenorrhea:
- Primary - not associated with diseases of the internal genital organs, occurs in adolescence 1 - 1.5 years after the onset of the first menstruation (menarche). Most often it manifests itself in girls who are emotionally unstable, overly sensitive, asthenic in build and underweight.
- Secondary - most often diagnosed in women after 30 years of age against the background of pathological processes in the pelvic organs (endometriosis, developmental anomalies, chronic inflammatory and non-inflammatory diseases of the internal genital organs, after complicated childbirth, traumatic abortions, surgical interventions, etc.)
Treatment
When a patient complains of algodismenorrhea, the doctor’s task, first of all, is to relieve the painful episode and prevent repeated painful attacks.
Treatment of this condition should be complex and etiopathogenetic. After consultation with an endocrinologist and clarification of the patient’s hormonal status, hormone therapy may be prescribed.
Considering the obligatory inflammatory component of the pathogenesis of algodismenorrhea, the prescription of NSAIDs is mandatory. Treatment is carried out for a long time. For several months, along with the use of a general complex of drug therapy, pain-relieving drugs are prescribed.
Let us recall that the basis of the pain syndrome in algodismenorrhea is smooth muscle spasm. Therefore, the drugs of choice are antispasmodics, which are recommended to be taken 1-2 days before the onset of menstruation and throughout the entire period.
Antispasmodics have a direct myotropic effect on smooth muscles, helping to relieve painful spastic contractions and eliminate vasoconstriction, which is one of the factors in the development of uterine ischemia.
Treatment of algodismenorrhea
Treatment of algodismenorrhea is prescribed by a doctor after a gynecological examination, ultrasound of the pelvic organs, and hormonal analysis. Sometimes additional examination of the urinary system, digestive organs, and circulatory organs may be required. This will allow us to most accurately determine the cause, form and prescribe effective treatment.
After receiving diagnostic tests, the patient is prescribed a comprehensive and effective treatment with a careful selection of medicinal and non-medicinal agents that are most suitable for her. Highly qualified specialists at our DeVita clinic will help you determine the duration of the course of treatment, a set of necessary measures, and accurately calculate the dosage of medications.
The specialists of our DeVita clinic will provide you with timely and highly qualified assistance and will help you get rid of algomenorrhea in a short time . You can always make an appointment with a doctor at the DeVita clinic without waiting in line at a time convenient for you. Untimely treatment or self-treatment of algodismenorrhea can lead to serious consequences, progression of the disease, and infertility.
Which antispasmodic to choose?
According to the mechanism of action, antispasmodics are divided into two classes:
✅ Myotropic antispasmodics - directly affecting biochemical processes in smooth muscle cells, or selectively acting on individual smooth muscle organs. Modern representatives of this group are papaverine and drotaverine.
✅ Vegetotropic antispasmodics - disrupt the transmission of nerve impulses in the autonomic ganglia or the endings of the autonomic nerves. They are derivatives of the belladonna alkaloid – scopolamine.
Of the modern antispasmodics of the group of selective anticholinergics, drugs based on scopolamine butyl bromide are the most widely used in the world.
The treatment of primary and secondary dysmenorrhea has fundamental differences. The first is treated with NSAIDs, gestagens, and combined oral contraceptives.
Anti-inflammatory drugs such as indomethacin, diclofenac, nemisulide, ketoprofen, ibuprofen, meloxicam, acetylsalicylic acid, etc. are used. The use of combination drugs is acceptable.
When prescribing NSAIDs, the gynecologist observes the patient for three menstrual cycles, assesses the effectiveness of therapy and, if necessary, adjusts the dosage. If the results are good, the woman is scheduled for a follow-up visit in six months. If such tactics are ineffective, the patient is indicated for hormone therapy with monitoring of the effectiveness of therapy every 3 months for a year.
Women of childbearing age who require contraception are recommended to take COCs with drospirenone or dienogest. These drugs are taken until the woman decides to become pregnant, and if there are no such plans, for an indefinite period until the onset of menopause. After this, a transition to hormone replacement therapy is possible.
In some cases, a treatment option may be the installation of an intrauterine device. After hormone withdrawal, the effect may persist for some time, but sooner or later the symptoms of dysmenorrhea may still return.
- Sol. Drotaverini 40 mg intramuscularly;
- Sol. Ketorolaci 30 mg intramuscularly.
Causes of algodismenorrhea
The causes of algodismenorrhea, namely the development of its primary form, are most often:
- Mechanical: abnormalities in the development of the uterus, abnormal position of the uterus, leading to difficulty in the normal outflow of menstrual blood;
- Endocrine: the cause of spastic contractions of the uterine muscle, causing prolonged spasm, is an increase in the synthesis and slowdown of the breakdown of prostaglandins;
- Neuropsychogenic: often there is an individual decrease in the threshold of pain sensitivity, denial and non-acceptance of oneself as a woman and mother;
- Constitutional: is infantilism. There is hypoplasia of the uterus, poor development of the myometrium, the ability of the organ to stretch during menstruation decreases, as a result of which the pressure on the walls of the uterus increases, which causes irritation of the nerve fibers and the occurrence of pain.
The most common causes of secondary (symptomatic) algodismoneria are:
- External endometriosis is the spread of the inner layer of the uterine cavity (endometrium) outside the uterine cavity: external genital endometriosis, endometrioid cysts of the ovaries, cervix, etc.
- Adenomyosis is the spread of the endometrium into the body of the uterus.
- Uterine fibroids. Myoma prevents the outflow of menstrual blood, the uterus begins to contract more intensely, the pressure in its wall increases, the nerve fibers are irritated, and prostaglandins are released, causing pain.
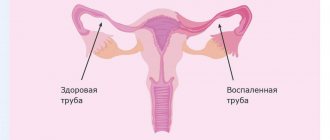
- Inflammatory diseases of the internal genital organs. Especially chronic, long-term ones provoke the formation of adhesions and disruption of the correct location of the uterus in the pelvis.
- Installation of an intrauterine device helps stimulate the production of prostaglandins.
- Anomalies in the development of the genital organs. A rudimentary uterine horn with an active endometrium, a doubling of the uterus with hypoplasia of one of them, and atresia of the cervical canal of the cervix lead to difficulty in the outflow of menstrual blood.
- Traumatic childbirth, abortion, surgical interventions on the uterus and appendages.
The cause of algodismenorrhea in this case is a rupture of the posterior leaf of the broad ligament of the uterus or varicose veins of the small pelvis.
HOW TO MAKE CRITICAL DAYS EASIER
Menstruation is a monthly process in a woman’s body when a fairly strong hormonal imbalance occurs.
This is a very painful process that entails rapid and unexpected mood swings, unpleasant physical pain and irritability. In fact, you can help yourself without exposing yourself to unpleasant sensations.
A decoction of raspberry leaves has beneficial properties. It will ease bleeding and help withstand blood loss.
Raspberry leaves are rich in minerals, vitamins and rare alkaloids, which regulate the body's metabolism and muscle tone.
A special pillow will improve the quality of your sleep, it will help relax the muscles of the neck and shoulders, and will reduce pain in this area, which is typical during critical days. Primrose oil or coconut oil is guaranteed to help get rid of cramps and cramps. You need to take them constantly or a week before your period.
During menstruation, you need to follow proper nutrition, since salty, fatty and sweet foods only worsen your well-being. It is also better to include foods containing vitamins A, B6, C and an increased amount of complex carbohydrates in your diet.
If possible, red foods, coffee and chocolate should be excluded from the diet. If cystic acne occurs, you need to introduce foods containing calcium, beets, carrots, cabbage, garlic and artichokes into your diet. Try not to be nervous on critical days, treat yourself to something pleasant, for example, a new purchase or a surprise. Take more walks in the fresh air.
The use of tampons very often leads to pain and cramping, so it is better to use sanitary pads.
One of the excellent methods of getting rid of physical discomfort during menstruation is yoga (for those who do it), or relaxation, or light exercise. First, take a bath, relax and do some exercises.
Cobra pose, bridge or fetal pose are most suitable to engage the pelvic and abdominal muscles and relieve muscle tone, in turn, exercises have a positive effect on a woman’s body during menstruation. As you know, during physical exercise the body releases the hormone endorphin, and it acts as a kind of analgesic.
The uterus is a muscle that, when contracted, causes pain; Try doing a deep pelvic massage by placing a rolled towel under your lower back, this will help relieve pain. And, of course, taking herbs will ease your condition.
Keep in mind that if you experience very severe pain during your period, this may be due to serious gynecological diseases, in which case consult a doctor.
Algomenorrhea, painful menstruation: traditional medicine recipes, recommendations
More often observed in young women. Pain appears 1-2 days before the onset of menstruation and continues for the first 2 days. They can occur with inflammatory diseases of the genital organs, as well as with increased excitability of the nervous system. There may be neuropathological reasons. For example, endocrine imbalance can cause a sharp constriction of blood vessels in muscle tissue or in the mucous membrane. Symptomatically manifested in the form of pain in the lower abdomen, headache, dizziness, nausea, vomiting.
In these cases, you can use the technique of oriental massage.
Lie on your back or sit, leaning against the wall, stroke, then massage the abdominal wall from top to bottom (from the lower part of the Georgian to the lower part of the abdomen), gradually increasing the pressure until using the “drawing” massage technique only 15-20 times.
Then proceed to kneading (mainly the lower abdomen) - 15-20 times. This is followed by applying pressure with rotation in the same area - 15-20 times. Having finished treating the abdomen, you should move on to the back area.
The back massage also begins with stroking from top to bottom, from the area 10 centimeters above the lower back to the tailbone. Stroking turns into rubbing, kneading, pressing with rotation. A total of 20-30 times. This is followed by light tapping and chopping.
✅ Linear massage must be combined with acupressure.
✅ Infusion or decoction helps in these cases (5 min.) 1 tsp. chopped lovage roots. Take 1 tbsp. 3 times a day before meals.
✅ Celery juice has an analgesic effect for menstrual pain, take ½ glass in 2 doses.
✅ Common wormwood (Chernobyl) is used as an infusion of 1 tbsp. per glass of boiling water, heat for 30 minutes. take ½ glass 2 times a day.
✅ Infusion 2 tbsp. red clover in 1 tbsp. boiling water for 6 hours, covered, drink 3-4 doses before meals.
✅ For painful periods, it is useful to drink cumin tea: 1 tsp. Pour a glass of boiling water over cumin seeds and leave for 10 minutes. Drink a glass in small sips 2-3 times a day.
Algomenorrhea (Painful menstruation)
Primary algomenorrhea
Treatment should begin with non-drug methods. For painful menstruation, patients are advised to:
- learn to calm down, relax and cope with stress;
- workout;
- eliminate smoking and drinking alcohol;
- do not overcool;
- limit physical activity and sexual activity in the second phase of the menstrual cycle and during menstruation;
- If there is pain, place a heating pad on your stomach and pull your knees to your chest.
To prevent decompensation of algomenorrhea, it is important to preserve pregnancies, especially the first. Often, primary algomenorrhea goes away on its own after pregnancy and childbirth. Among the methods of physiotherapeutic treatment for algomenorrhea, electrophoresis with novocaine on the solar plexus area and reflexology are effective.
If non-drug therapy is ineffective for primary algomenorrhea, medications are prescribed. In case of primary algomenorrhea, accompanied by severe neuropsychic symptoms, it is possible to prescribe sedatives (diazepam, valerian, trioxazine). To relieve pain, antispasmodics and analgesics, non-steroidal anti-inflammatory drugs are used.
In primary algomenorrhea, the pain of menstruation significantly decreases or disappears with regular use of hormonal contraceptives, including a combination of ethinyl estradiol and levonorgestrel, or the introduction of injectable contraceptives. In case of primary algomenorrhea, a good effect is achieved by using drugs from the group of natural progestins.
During the treatment of algomenorrhea, it is recommended to keep a menstrual calendar, where you should reflect your feelings accompanying menstruation (pain, its duration, intensity, nature, localization, other symptoms) and consult a gynecologist once every three months.
Secondary algomenorrhea
Treatment consists of treating the primary disease. If the cause of secondary algomenorrhea is intrauterine contraceptives, it is recommended to remove them. For endometriosis, adhesions, and tumor lesions of the pelvic organs, various types of surgical interventions are used.
Treatment of inflammatory diseases that cause secondary algomenorrhea is carried out taking into account the identified cause and pathogen, followed by physiotherapeutic procedures and spa treatment. Also, in case of secondary algomenorrhea, symptomatic therapy is prescribed, aimed at reducing pain during menstruation (antispasmodic, analgesic, NSAIDs), weakening psycho-emotional symptoms (sedatives). When painful menstruation occurs, it should be remembered that even a mild degree of algomenorrhea indicates functional or organic disorders in the body, which are best diagnosed and treated as early as possible.