pharmachologic effect
The drug has chondrostimulating, regenerating, anti-inflammatory and analgesic effects. Participates in the construction of the basic substance of cartilage and bone tissue. Has chondroprotective properties; enhances metabolic processes in hyaline and fibrous cartilage and subchondral bone; inhibits the activity of enzymes that cause degradation (destruction) of articular cartilage; stimulates the production of proteoglycans by chondrocytes; influences phosphorus-calcium metabolism in cartilage tissue, stimulates its regeneration, and participates in the construction of the basic substance of bone and cartilage tissue. It has anti-inflammatory and analgesic properties, helps reduce the release of inflammatory mediators and pain factors into the synovial fluid through synoviocytes and macrophages of the synovial membrane, and suppresses the secretion of lykotriene and prostaglandins. The drug prevents connective tissue degeneration and reduces calcium loss, accelerating bone tissue restoration processes.
Chondroitin sulfate slows the progression of osteoarthritis and osteochondrosis. Promotes the restoration of the joint capsule and cartilaginous surfaces of the joints, prevents the collapse of connective tissue, and normalizes the production of joint fluid.
The clinical effect is manifested by an improvement in joint mobility and a decrease in pain intensity, while the therapeutic effect persists for a long time after the end of the course of therapy. When treating degenerative changes in joints accompanied by secondary synovitis, the effect is observed within 2-3 weeks from the start of the course.
Possessing structural similarity to heparin, it can potentially prevent the formation of fibrin thrombi in the synovial and subchondral microcircular bed.
For what diseases are chondroprotectors used?
Glucosamine and chondroitin preparations help protect joints from “starvation” and chemically aggressive substances that accumulate in them as a result of inflammation. For this reason, they are recommended for adjuvant therapy of osteochondropathy - diseases that cause necrosis of spongy bone tissue (bone heads). Chondroprotective drugs are used for the treatment and prevention of:
- osteochondrosis;
- osteoarthritis (including rheumatoid and gouty arthritis);
- spondylosis (spondyloarthrosis);
- osteoporosis;
- tendonitis (dystrophic disease of the tendons);
- bursitis (inflammation of the joint capsule)
Chondroprotectors will become indispensable assistants in the fight against joint diseases
Drugs in this group are recommended for congenital and acquired pathologies of bone tissue (for example, bone deformation), hernias and protrusions. Chondroitin sulfate has proven itself as an auxiliary substance in the treatment of keratitis (inflammation of the eye cornea). Chondroprotectors for arthrosis are prescribed at stages 1-2 of the disease.
Pharmacokinetics
Chondroitin sulfate sodium is easily absorbed when administered intramuscularly. 30 minutes after the injection of chondroitin, sodium sulfate is found in the blood in significant concentrations; after 15 minutes - in the synovial fluid.
The maximum concentration in blood plasma (Cmax) is achieved 1 hour after administration; then the concentration of the drug gradually decreases over 2 days.
Chondroitin sulfate sodium accumulates mainly in cartilage tissue (the maximum concentration in articular cartilage is reached after 48 hours); the synovial membrane is not an obstacle to the penetration of the drug into the joint cavity.
It is excreted from the body mainly by the kidneys within 24 hours.
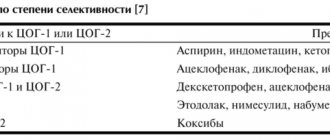
Classification of chondroprotectors
In medical sources, chondroprotectors for joints are divided by generation:
- 1st generation.
Animal and plant extracts and concentrates rich in glucosamine and chondroitin; - 2nd generation.
Preparations that contain purified glucosamine or chondroitin. They are absorbed faster and easier, and are less likely to cause allergies; - 3rd generation
. Combined products that combine glucosamine, chondroitin, sulfur preparations and other components. The composition of new generation chondroprotectors is often supplemented with anti-inflammatory drugs (ibuprofen, diclofenac), fatty acids (improves the elasticity of cartilage and protects its cells from destruction), vitamins (for better absorption of active substances and protection of cell membranes) and microelements (for building stable cartilage tissue).
New generation chondroprotectors make the patient feel better much faster and have fewer side effects.
Chondoprotectors are available in various forms. Choose what suits you.
Pills
Tablets and capsules are prescribed in courses of 3-6 months. They are especially effective for lesions of large joints or systemic diseases that affect 4 or more joints. Capsules are absorbed almost as well as liquid glucosamine, but are stored and dosed much better. The absorption of these chondroprotectors is quite high - 13-25%.
Chondroprotective ointments
Local chondroprotectors (ointments and gels) are used for arthrosis of intervertebral, small and medium-sized joints. External preparations have minimal bioavailability (less than 5%) and have virtually no effect on the structure of cartilage, especially if it lies deep under the skin. But chondroprotective ointments have a beneficial effect on periarticular tissues, relieve pain and swelling, and reduce inflammation. In the absence of an allergic reaction, they can be used continuously.
Powders for the treatment of joints
Powder chondroprotectors are the rarest form of release. Glucosamine powder is well absorbed by the body (bioavailability over 26%), but is not recommended for gastrointestinal diseases. Typically, manufacturers include additional components that improve the metabolism of cartilage tissue.
Chondroprotectors in injections
Injections of chondroprotectors are most effective in comparison with other forms of glucosamine and chondroitin. They are placed intramuscularly and intraarticularly. Injectable medications are a good alternative to oral medications if the patient has gastrointestinal diseases.
An intramuscular injection of a chondroprotector can be done independently or with the help of loved ones, but injection into the joint should only be carried out by an experienced medical professional.
Intra-articular administration of CP (usually with painkillers and anti-inflammatory drugs) is considered the most effective. Chondroprotectors in injections help with synthesis disorders - when cartilage tissue stops producing substances necessary for the growth and hydration of cartilage.
Contraindications
- hypersensitivity to the components of the drug;
- bleeding and tendency to bleeding, thrombophlebitis;
- children under 18 years of age, pregnancy and breastfeeding (there are no data on the safety of the drug).
Carefully
Simultaneous use of the drug with direct-acting anticoagulants.
Use during pregnancy and breastfeeding
The use of Chondroitin sulfate during pregnancy is contraindicated. If the drug is used during breastfeeding, breastfeeding should be discontinued.
Chemical structure
Chondroitin sulfate chains are unbranched polysaccharides with no fixed length. Chondroitin sulfate consists of only two simple sugars, constantly changing one of D-glucuronic acid and N-acetylgalactosamine. Glucuronic acid combines with N-acetylgalactosamine through a β-1,3 glycosidic bond, and N-acetylgalactosamine combines with β-1,4 glucuronic acid. The chondroitin sulfate chain can contain more than 100 sugar residues, which can differ quite greatly from each other. The N-acetylgalactosamine C6 and/or C4 atoms may be sulfated. If glucuronic acid is epimerized at C5 to form induronic acid, the GAG is called dermatan sulfate.
special instructions
It is recommended to increase doses under the supervision of a physician for patients with excess body weight, gastric or duodenal ulcers, while taking diuretics, as well as at the beginning of treatment, if it is necessary to accelerate the clinical response. In case of allergic reactions or hemorrhages, treatment should be stopped.
Effect of the drug on the ability to drive vehicles and machinery
The drug does not affect the ability to drive vehicles and machinery, or the ability to engage in potentially hazardous activities that require rapid psychomotor reactions.
Indications and contraindications for taking chondroprotectors
Although chondroprotectors are useful for diseases of ligaments and even periodontal tissue, their main use in medicine is the protection and restoration of joints. Chondroprotectors for joints are made from natural products that have been part of the human diet for centuries, so side effects and contraindications are very rare.
Who needs chondroprotectors for joints?
Joint damage is common among athletes, manual workers, and people who lead a sedentary lifestyle. People with age-related changes in hormonal levels and people over 45 years of age are also at risk. The presence of autoimmune and metabolic diseases (systemic lupus erythematosus, rheumatoid arthritis, diabetes mellitus, gout), excess weight is a good reason for the preventive use of chondroprotectors.
You need to start a course of glucosamine and chondroitin:
- at stages 1 and 2 of osteoarthritis and other rheumatic diseases;
- for diseases of ligaments and tendons;
- after injuries and joint surgeries;
- for diseases with a tendency to damage joints;
- in other cases as prescribed by a doctor.
Who should not take chondroprotectors?
Absolute contraindications to taking chondroprotectors for joints are phenylketonuria (a disorder of amino acid metabolism) and individual intolerance to their components. A preliminary consultation with a specialist before taking chondroprotective agents and further observation is necessary for:
- pregnant and lactating women;
- children under 12 years of age;
- asthmatics (if breathing is difficult, the drug should be discontinued);
- diabetics (glucosamine changes glucose tolerance);
- allergy sufferers (especially those with allergies to various types of protein and shellfish);
- patients with gastrointestinal diseases in the acute phase (gastritis, gastric or duodenal ulcers);
- people with kidney disease (including cholelithiasis, urolithiasis, renal failure) and liver failure;
- patients with vascular pathologies (including varicose veins, thrombosis and thrombophlebitis) and blood clotting disorders;
- persons with oxaluric diathesis;
- patients diagnosed with malignant tumors.
Side effect
When using the drug in persons with hypersensitivity to the drug, the following disorders are possible:
- from the immune system: allergic reactions, angioedema;
- from the skin and subcutaneous tissue: skin rash, itching, erythema, urticaria, dermatitis;
- from the gastrointestinal tract: dyspepsia.
Redness, itching, and hemorrhages are possible at the injection site.
Overdose
Currently, cases of drug overdose have not been described.
Sulfation
Each simple carbohydrate may contain one or two sulfo groups, or none at all. Most often, sulfo groups are attached to hydroxy groups of 4 and 6 carbon atoms. Sulfation is catalyzed by various sulfotransferases. The degree of sulfation averages 0.8 per disaccharide.
There are the following types of chondroitin sulfate:
| Type of chondroitin sulfate | Systematic name | Disaccharide residue | Detailed description |
| chondroitin sulfate A | chondroitin-4-sulfate | Example | the sulfate group is located predominantly on the 4th carbon atom of N-acetylcholine |
| chondroitin sulfate B | dermatan sulfate | Example | the sulfate group is located predominantly on the 2nd carbon atom of induronic acid and on the 4th carbon atom of N-acetylcholine |
| chondroitin sulfate C | chondroitin-6-sulfate | Example | the sulfate group is located predominantly on the 6th carbon atom of N-acetylcholine |
| chondroitin sulfate D | chondroitin-2,6-sulfate, dermatan sulfate | Example | the sulfate group is located predominantly on 2 glucuronic acid and on the 4 carbon atom of N-acetylcholine (Chondroitin-2,6-sulfate) |
| chondroitin sulfate E | chondroitin 4,6-sulfate | Example | the sulfate group is located predominantly on the 4th and 6th carbon atoms of N-acetylcholine |
Typing by letters from A to E was used back in the days when chondroitin sulfate was isolated (isolated), but its formula was not known. The classification of dermatan sulfate as chondroitin sulfate as chondroitin sulfate B is now considered erroneous, since this molecule contains neither glucuronic nor induronic acid. The most common types are chondroitin sulfate A, B and C. Previously, the name chondroitin (sulfate-free) was used to name a chain with few or no sulfate groups; today this term is no longer used.
Functions of chondroitin sulfate
The function of chondroitin is highly dependent on the properties of the entire proteoglycan of which it is a part. Chondroitin proteoglycan has both structural and regulatory functions.
Structural function
Chondroitin proteoglycan, together with collagen, is a significant component of the extracellular substance. They exert structural integrity on tissues. Typical representatives are aggrecan, versican, brevican and neurocan.
Chondroitin sulfate, as a component of aggrecan, forms most of the cartilage mass. The densely packed, highly charged sulfate groups lead to electrostatic repulsion of the individual chains, which accounts for much of the cartilage's resistance to compression. A decrease in the amount of chondroitin sulfate in cartilage is a common cause of arthrosis.
Biological role
Chondroitin sulfate has an affinity for cartilage tissue, initiates the process of sulfur fixation during the synthesis of chondroitin-sulfuric acid, which, in turn, promotes the deposition of calcium in the bones. Stimulates the synthesis of hyaluronic acid, strengthening connective tissue structures: cartilage, tendons, ligaments, skin. It has an analgesic and anti-inflammatory effect, is a chondroprotector, and promotes active regeneration of cartilage.
A special feature of chondroitin among proteoglycans is its ability to retain water in the thickness of cartilage in the form of water cavities, creating good shock absorption and shock absorption, which ultimately increases the strength of connective tissue. An important effect of chondroitin is its ability to inhibit the action of specific enzymes that destroy connective tissue, including lysosomal enzymes released as a result of the destruction of chondrocytes (elastase, peptidase, cathepsin, interleukin-1, etc.)
The natural intake of chondroitin sulfate and other chondroprotective substances was through the consumption of tendons, skin and cartilage of animals, especially fish. Due to the decreasing proportion of these products in the modern human diet (sometimes with a complete exception), as well as with metabolic disorders, excessive functional stress and especially an age-related decrease in the activity of synthetic processes, chondroitin sulfate must be supplied ready-made (or in the form of synthesis precursors) from the outside including with food.
Protein binding
In living organisms, chondroitin sulfate is bound to a protein, both being part of the same proteoglycan.
The binding of chondroitin sulfate chains is carried out by the serine residue of the hydroxy group of a particular protein. It is unknown how proteins are selected to bind to glycosaminoglycans. Glycosylated serine residues often follow glycine residues, and acidic amino acid residues are located nearby. The binding agent of the GAG chain is always the same sugar chain of three carbohydrates: Ser-O-Xyl-Gal-Gal -GlcA -...
Each carbohydrate is bound by a specific enzyme, which makes multi-level control of GAG synthesis possible. Xylose is bound to the endoplasmic reticulum by proteins, while the remainder of the carbohydrate is transferred to the Golgi apparatus.