Conventionally, all inhalations can be divided into two groups:
- Natural - when a person inhales clean mountain or sea air. This type of inhalation can be classified as therapeutic and prophylactic methods of therapy. This group has a mild therapeutic effect on the mucous membranes and is most effective for chronic diseases of the respiratory system, and also helps strengthen the immune system.
- Artificial. This is the inhalation administration of drugs into the upper respiratory tract using inhalers (nebulizers).
A nebulizer is a special portable device for inhalation. The word itself is of Latin origin: “nebula” translated from this ancient language means cloud or fog. These devices transform liquid medicinal substances using compressed air into aerosols or cold vapor (fog). It is then sprayed into the upper and lower respiratory system.
Inhalations can be recommended for almost all types of cough, but it is necessary to take into account which drug will be selected by the doctor. It may be different for each specific disease. [1]
Contraindications to inhalation are:
- Increased body temperature, more than 37.5 degrees.
- Cough accompanied by purulent sputum.
- Nosebleeds.
- Allergic reactions or intolerance to the components included in the solution.
- Arrhythmia.
- Severe diseases of the cardiovascular and respiratory systems.
Benefits of inhalation:
- A gentle and safe method of treatment.
- Significant reduction in the period of illness.
- Facilitating the process of sputum secretion.
- Reducing the risk of pathological processes at all stages of the disease.
- Reducing the severity of cough.
- Possibility of using natural herbal ingredients.
How are nebulizers different?
There are several types of nebulizers:
- Compressor
- Ultrasonic
- Membrane
Each has its own pros and cons. An important task of the nebulizer is to deliver the drug to the site of inflammation in the upper and lower respiratory tract. Ultrasonics can destroy medicinal active substances, and the effectiveness of treatment decreases. For home use, it is better to choose compressor or membrane ones. The former are more expensive and weigh more, but they do not require additional parts and are easy to clean. The latter are convenient to take on a trip, they are silent, but you need to buy consumables for them.
For children under 5 years of age, inhalations are performed while sitting using a special mask, which should fit tightly to the nose and mouth. Starting from 5 years old, children, as well as adults, breathe through a mouthpiece, which is included with the mask. You should inhale air through your mouth through the mouthpiece and exhale through your nose. After inhalation, rinse the mask, mouthpiece, and tubes with running water and soap, and dry thoroughly.
What are inhalers and how do they work?
There are many types and models of inhalers in the pharmacy chain, all of them have a similar design. Currently, three main types of inhalers are used in medical practice: steam, ultrasonic and jet. The last two are united by the term “nebulizers” from the Latin word nebula - fog, cloud. They generate not vapors, but a stream of aerosol consisting of microparticles of the inhaled solution.
The inhaler includes a main unit that generates a stream of air that creates a medicinal aerosol of the required dispersion. In the main block there is a chamber in the form of a plastic glass with a volume of 5-10 ml, into which the medicinal solution is poured.
The container contains a damper with two outputs, one of which leads to the device itself, and the second is the output. A tube, mouthpiece or mask is attached to this hole, into which an aerosol of medium and low dispersion is supplied. Coarsely dispersed solutions lead to rapid breakdown of the device and a decrease in the effectiveness of treatment. Nebulizers may include special mouthpieces, children's masks, nasal attachments, sprayers, and a mouthpiece.
Indications and contraindications
Typically, inhalations are prescribed for obstructive bronchitis, bronchial asthma, chronic obstructive pulmonary disease, and croup syndrome.
“The nebulizer is used only to deliver a medicinal substance to the mucous membrane of the respiratory tract,” says Anastasia Shledovitz, a pediatrician at the Fantasy children’s clinic, “so there are not many main indications for its use: bronchodilators for bronchial obstruction, inhaled hormones for croup syndrome and combination drugs for bronchial obstruction. asthma. Self-prescribing these drugs can be harmful, especially for young children.”
If you have a runny nose, sinusitis, sore throat, adenoids, or redness of the throat, inhalation is not recommended.
“Often in children during the adenoid period, cough and runny nose can drag on and go beyond the normal course of ARVI, that is, last more than 10 days,” says Oleg Abramov, an otolaryngologist and head of the center for operative surgery at GMS Hospital. — Such a cough should be treated with proper drug therapy aimed at reducing snot. Inhalations with saline or hormonal agents will not have any effect in terms of cough relief.”
Inhalations are most often prescribed for a sudden cough. The course of treatment usually ranges from 1 to several days. For “residual cough” after ARVI, which occurs after sleep and when leaving a warm room into a cold one and vice versa, treatment is usually not required.
“If a child or adult has been coughing for more than three weeks due to mucus draining down the back wall of the throat,” adds Oleg Abramov, “this requires consultation with an ENT doctor to conduct an endoscopic examination and identify the cause that may lead to this.”
If there is no pathology of the nasopharynx, but a persistent cough persists, it is necessary to visit a gastroenterologist, pediatrician or therapist, in some cases an infectious disease specialist.
What rules must be followed when using such devices?
Inhalations will give the desired effect after just a few procedures. However, not everyone knows how to properly inhale using a nebulizer. There are a number of rules that cannot be ignored:
- You need to start inhalation 1-1.5 hours after eating and performing serious physical activity;
- During the procedure, it is not advisable to be distracted by reading, much less talking;
- clothing should not restrict the neck area, so as not to impede breathing;
- Smoking is not recommended during inhalation therapy;
- for diseases of the nasopharynx, nose or paranasal sinuses, it is recommended to carry out nasal inhalation (it is best to inhale the aerosol through the nose), using a mask or special nozzles;
- for diseases of the pharynx, larynx, trachea, bronchi and lungs, the aerosol should be inhaled through the mouth, while breathing evenly. Taking a deep breath, you need to try to hold your breath for 2 seconds and calmly exhale through your nose;
- before inhalation, you do not need to take medications that improve sputum discharge, or rinse your mouth with antiseptics;
- After the procedure, you should rinse your mouth with boiled water cooled to room temperature. If a mask was used for inhalation, it is also necessary to rinse the face and eyes;
- Eating, drinking and talking is prohibited for 15-20 minutes after inhalation;
- Inhalations with medications should be carried out up to 3 times a day.
Yuri Alisievich, Trade portal Shop.by
What solutions can be added to the nebulizer?
Only those that have instructions in the instructions for use of the drug: budesonide, impratropium bromide, ventolin, fluimucil - an antibiotic. Sputum thinners are not recommended for children under 12 years of age due to the possible worsening of the disease. It is not recommended to add mineral water, oils, various syrups and cough solutions, herbal tinctures, baking soda due to the high risk of side effects and prolongation of the cough period.
You can read the continuation of the article by following the link to FORMA - SBER PHARMACY blog.
Who needs inhalation and when is it dangerous?
How much to breathe with the inhaler and when it is needed is determined by the attending physician. Prescription of procedures is practiced when identifying disorders such as:
- Allergic and asthmatic lung diseases with attacks.
- Bronchitis of various forms.
- Pathologies of the endocrine system.
- Cystic fibrosis.
- Respiratory tract fungus.
- ARVI, flu, rhinitis. You can breathe with an inhaler if you have coronavirus.
- Cardiovascular disorders.
- Tuberculosis.
- Occupational diseases of miners, chemists, actors.
- Pneumonia.
- Diseases of the nervous system.
How much inhalation to do and what substances to use depends on the type of cough the patient has. Therapy is indicated for dry tracheitis cough. It will help eliminate soreness and neutralize swelling of the larynx and vocal cords. For wet coughs, treatment with an inhaler thins the mucus and helps clear the bronchi.
You should not use equipment and medications yourself. Only the doctor determines whether inhalations can be done. There are a number of contraindications for therapy. Among them:
- Myocardial infarction, arrhythmia and other acute heart diseases.
- Hypersensitivity to active substances.
- Purulent sore throat.
- Fever. Answering the question whether it is possible to breathe with an inhaler at a temperature, doctors say that this is prohibited. It is not recommended to carry out therapy if the thermometer shows more than 37.5°C.
- Pulmonary failure.
- Tendency to nose and lung bleeding.
- Ischemic stroke.
- Severe hypertension.
Preparation of equipment
Before using the inhaler, you should perform a number of preparatory steps:
- Rinse the face mask, connecting hose and nebulizer chamber with clean water and dry.
- Treat elements in direct contact with the patient with an aqueous solution of chlorhexidine or miramistin.
- Assemble the device in accordance with the instructions.
- Fill the reservoir with a pre-prepared medicinal solution and place it in a vertical position.
The tank capacity for steam varieties is 70-100 ml, for compressor and ultrasonic varieties - 2-8 ml. If the maximum permissible volume is exceeded, liquid enters parts of the device that are not intended for this purpose and can damage the inhaler.
How to use an inhaler if you have a chronic illness
Inhalations for chronic respiratory diseases are the most effective treatment. This is necessary to relieve inflammation, which provokes attacks.
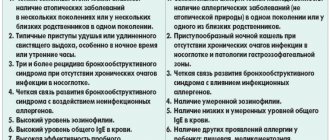
The most common attack triggers in chronic lung diseases.
For chronic diseases, inhalation is used:
- to relieve attacks and exacerbations (for emergency medical care);
- for basic treatment of patients at risk of frequent exacerbations;
- for taking medications that can only be delivered by nebulizer;
- at large doses of the drug.
There is no fundamental difference in the technique of using an inhaler compared to the treatment of ARVI and influenza.
How to perform inhalations
Before use, prepare the nebulizer: pour the inhalation solution into the nebulizer chamber. Do not place it on its side as this may cause the medicine to spill out.
It is recommended to carry out inhalation while sitting, in a relaxed position.
- Press the power button.
- Cover the mouthpiece tightly with your lips.
- During inhalation, breathe slowly and deeply.
The duration of inhalation and the volume of medication are prescribed by the doctor.
How to carry out inhalations.
Equipment and drugs for inhalation
Inhalations are of the following types:
- Steam. Breathe over potatoes, a kettle or other source of steam. This helps warm the nasal passages and throat. It is not necessary to use medical inhalers and medications. Sometimes medicinal herbs are added to boiling water, for example, St. John's wort, chamomile, eucalyptus.
- Dry. The patient breathes in the medicine in powder form. Special sprayers are used.
- Heat-moist. Performed using a compressor. Patients breathe moist, hot air.
- Aerosol. The drug is sprayed through a nebulizer or can.
- Oily. Hot vegetable oil is poured into the inhaler. The substance relieves inflammation and irritation of the mucous membrane.
Why does a dry cough appear?
First, it’s worth defining the very concept of a dry cough. Its main differences from the productive one are the absence of mucous secretions and localization. A dry cough forms in the larynx, and a wet cough forms inside the chest.
Under the influence of an inflammatory process, allergy or virus, the back wall of the larynx becomes irritated. A signal is sent to the brain that triggers the cough reflex to clear the airways. As a result, irritation of the mucous membrane of the larynx intensifies, which leads to the formation of another wave of coughing. It turns out to be a vicious circle.
When a dry cough appears, it is important to identify its cause in order to select adequate treatment. The symptom may occur when the larynx becomes inflamed or when the virus enters the lower part of the respiratory system. Sometimes in this way the body reacts to external irritants, internal pathologies, and allergens. Cough medications and treatment methods should be selected by a doctor after diagnostic procedures.
Inhalations with bromhexine
What does bromhexine help with?
Bromhexine is a mucolytic and expectorant drug. The drug is used for bronchitis, pneumonia, laryngitis, pharyngitis, tuberculosis, bronchial asthma. It can be used for both dry and wet coughs. It is advisable to start taking bromhexine in the early stages of the disease to get the best effect.
Cough preparations by group
Is it possible to do inhalations with bromhexine?
According to the instructions, bromhexine is taken orally, and there is no official information that it should be used for inhalation, but sometimes it is used by inhalation at home.
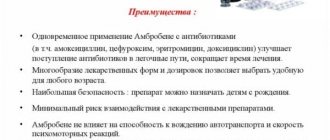
The closest analogue of bromhexine, ambroxol (Ambrobene, Lazolvan, etc.), is sold specifically in the form of a solution for inhalation. In any case, before using this or that drug, be sure to consult a specialist.
Which bromhexine is suitable for inhalation?
As an example, let’s take the form: bromhexine drops 8 mg/ml. Before inhalation, it must be diluted with distilled water in a 1:1 ratio.
If you take another solution of bromhexine, where the dose of the drug is 4 mg per 5 ml, then the total volume for an adult will be 20 ml. Whereas the inhaler chamber usually has a maximum capacity of 5 ml.
Bromhexine solution for inhalation
Dosage for preparing the solution:
- adults: 8 mg, which corresponds to 1 ml of bromhexine drops;
- children over 10 years old: 4 mg;
- children from 6 to 10 years old, 2 mg;
- children under 6 years of age in a dose of up to 2 mg;
- Toddlers should not use this form due to the high concentrations of substances it contains.
Inhalation is carried out twice a day. Course of treatment: 5 days.
How to prepare the solution
Dilute the drug with distilled water (water for injection) in a 1:1 ratio. Then the prepared solution is heated to a temperature of 36-38 degrees, but no more and no less, because high and low temperatures of the solution negatively affect the inflammatory process. At a temperature of 25-28 degrees it is an irritant for the bronchi due to the cold factor. And if the solution is 39-40 degrees, then it has a detrimental effect on the components of the medicine: such a temperature destroys the medicine.
Read in this article:
- Why does a dry cough appear?
- How do inhalations work on dry cough?
- When can and cannot use a nebulizer?
- What drugs are inhaled?
- Rules for the procedure
- Nebulizers for inhalation for dry cough
- How to deal with dry cough effectively and safely?
A dry cough is often a companion to ENT diseases, colds and other pathologies. Such an obsessive symptom causes discomfort and can be truly debilitating. But there are quite effective methods for treating such conditions.