Antibiotics are used for infectious diseases caused by bacteria. They either destroy pathogenic microorganisms (bactericidal drugs) or limit their proliferation (bacteriostatic antibiotics), leaving the immune system to fight the infection itself.
In order for antibiotics to be effective, you must follow certain rules for taking them.
Antibiotics are prescribed by the doctor
Only a specialist can choose the appropriate drug from the huge number of items produced by the pharmaceutical industry. When prescribing a medicine, the doctor takes into account the disease, age and condition of the patient, the presence of concomitant pathologies, and the side effects of the drug. And if the doctor prescribed you an antibiotic, you need to take it.
Today there are two extreme points of view regarding antibiotics. Some consider them an absolute evil and refuse treatment. Others, on the contrary, are ready to swallow antibiotics for any cold. Both are wrong.
Yes, indeed, this group of drugs is far from harmless, and while killing pathogenic microbes, they also destroy beneficial microflora. But in case of severe infections, you cannot do without them. By refusing to take the pills, you risk ending up in a hospital, where you will be given the same antibiotics, but by injection or through an IV, and in much larger doses.
Those who try to treat a runny nose with antibiotics (and this is a viral infection that antibiotics have no effect on) will not get rid of the disease, but they may suffer from the side effects of the drug.
Can only be used as prescribed by a doctor
It is very important to take antibacterial agents only in cases where you cannot do without them. It is unacceptable to take medications on your own initiative. Indications for the use of antibiotics include various symptoms of infectious diseases that cannot be treated on your own:
- Prolonged high temperature.
- Purulent processes.
- Exacerbations after pathologies of a bacterial nature.
- Disturbance in the structure of the circulatory system. There is an increase in the level of white cells, an increase in ESR and other characteristic signs indicating inflammation.
It is worth remembering that antibacterial agents are not effective against viruses. Therefore, this pharmacological group is not prescribed to patients to combat influenza, ARVI, and intestinal infections.
Antibiotics must be taken strictly according to the schedule
Your doctor will tell you your dosage regimen. In addition, each drug has instructions that describe in detail when (morning, evening, before/after meals) and how many times a day the medicine should be taken. Antibiotics should be taken at the same time, and the intervals between doses should be equal. Usually the drug is taken 1-2-3-4 times a day, which means the intervals should be 24-12-8-6 hours. This is the period of time the pill works, then its effect ends, and if you miss the time of taking it, the bacteria will begin to multiply intensively, poisoning the body. In addition, microorganisms may develop resistance to this antibiotic.
Accounting for medications used
It is advisable to keep records of all antibiotics used. Namely, it is worth recording the duration of the course, the name of the medicine, when it was taken and for the treatment of what disease. This is recommended not only for children, but also for adults.
During use, you need to take into account the body’s reaction to the drug, the development of possible side effects, and allergies. This will help the doctor adequately assess the situation and prescribe the most effective antibacterial agent.
It is also important to warn the specialist about the use of additional drugs that have been used recently or currently.
You need to complete the full course of treatment
As a rule, if the antibiotic is effective, improvement occurs on the 3rd day of treatment. But this does not mean recovery. You should not interrupt the course, even if you feel much better. By stopping taking the medicine ahead of time, firstly, you will soon feel worse, since not all bacteria have been destroyed, and secondly, your bacteria will become resistant to this antibiotic and in the future it will no longer act on them. You will get the same result if, after feeling an improvement in your condition, you reduce the dose of the drug.
Are probiotics necessary?
Antibiotics kill bacteria, but they do not distinguish good microorganisms from bad ones. These powerful drugs destroy vital bacteria necessary for the normal functioning of the digestive and immune systems. The best way to replenish losses is to consume probiotics, which contain live bacteria that normally inhabit the intestines.
Probiotics are prescribed during and after a course of antibiotics to restore intestinal microflora and, therefore, immunity. It is important to “dilute” the intake of medications: it is advisable to take the probiotic a couple of hours before or several hours after the dose of the antibiotic. The duration of use of probiotics after a course of antibiotic therapy is determined by the doctor.
For detailed advice on how to take antibiotics correctly, please contact your healthcare provider.
How to treat a sore throat?
You can try Strepsils® Intensive, lozenges [orange] containing flurbiprofen, an anti-inflammatory drug from the group of propionic acid derivatives that has an analgesic effect.
Strepsils® Intensive lozenges [orange] help reduce swelling, eliminate difficulty swallowing and combat pain, discomfort and irritation in the throat. It can be used for viral, bacterial and fungal diseases. 10
Antibiotics for viral diseases
Often, general practitioners prescribe antibiotics to their patients, such as Cetrin, at the first symptoms of the disease. They are taken in combination with antiallergic, antiviral and anti-cold medications. The question arises: “Do experts really not see the difference between a viral and bacterial infection?” Naturally, they see it. It is also clear to everyone that few people, after receiving a diagnosis of ARVI, will remain in bed and undergo treatment.
In reality, complications should not appear. A healthy body with a strong immune system is able to overcome seasonal diseases in 4-6 days. The patient must provide the body with all the necessary conditions: maintain bed rest, drink as much water as possible, ventilate the room.
In reality, few people follow these rules. Many continue to go to work and do household chores, which is why the illness can drag on for several weeks. As a result, active proliferation of microbes occurs in the body. Antibiotics then help prevent the spread of bacteria.
Individual selection of combinations
Sometimes a combination of medications is required, due to which synergism occurs - an increase in the pharmacological effect. The combination of drugs with each other, taking into account the dosage and type of action on the pathological process, allows you to increase the effectiveness of the treatment. At the same time, you can take both different types of antibiotics and a combination of antibiotics with other drugs. But only a doctor selects a regimen and draws up a treatment plan.
Independent experiments “shouldn’t I also take this pill, it helped my friend” can lead to unpredictable consequences.
Follow the instructions. If you drink it with water
Tea, coffee, orange, apple and any other juices, milk and dairy products - in most cases, all this is not suitable for washing down antibiotics intended for oral administration. These drinks speed up the elimination of the drug and may reduce the effectiveness of treatment. 5 Juices also contain various acids that can react with medications and cause unwanted reactions.6
It is most rational to use water when taking medications, unless otherwise indicated in the instructions. Be sure to read it before starting treatment. Tea and coffee are also undesirable because they contain caffeine, tannins and catechins, which can alter the absorption and pharmacological action of many drugs.7
The dangers of taking antibiotics
At the beginning of the 20th century, penicillin was considered a real miracle. Today it is used extremely rarely. It practically stopped acting on bacteria. Over time, they have evolved, grown stronger, and can now fight back. Following penicillin, many other new drugs cease to be effective. The longer you take them, the faster microbes will be able to adapt to them and improve their protective functions.
The paradox of the 21st century: the most dangerous, serious and difficult-to-treat diseases can be found in the cleanest hospitals, and not in garbage dumps. Cholera and plague are no longer a threat. The worst thing now is hospital-acquired staphylococcus. He was able to adapt to everyday sterilization; antimicrobial weapons do not react in any way. It is now called a superbug.
Every time you take antibiotics, bacteria receive some kind of information and the opportunity to adapt to their action. If you take antibiotics incorrectly, then very soon a person will feel defenseless. This may be due to incorrect determination of the required dosage or an incomplete course of treatment. As a result, after a while the disease will return again, but the medicine will no longer be effective. Even if a person does not allow bacteria to spread inside, they can always attack from the outside.
Laxatives
After using a laxative once or twice, some people prone to constipation begin to take these medications regularly. However, this should not be done: gradually the body gets used to the stimulants of peristalsis, and the natural contractions of the intestines come to naught. As a result, the functioning of the gastrointestinal tract, and then other organs, is disrupted. It is important to remember: a laxative is a means for emergency one-time assistance, which should never be abused.
Back to list Previous article Next article
Directions for use and dosage 10
Adults and children over 12 years of age: Slowly dissolve one tablet every 3-6 hours.
Maximum daily dose: 5 tablets.
The duration of treatment is no more than 3 days. If symptoms persist or worsen after taking the drug for 3 days, you should stop treatment and consult a doctor.
Before using the drug, read the instructions.
You can also use Strepsils® Intensive spray for topical use dosed with flurbiprofen. The drug penetrates the throat tissue and acts on the cause of pain – inflammation. Helps relieve sore throat. The interval between doses of the drug is up to 6 hours. It is recommended to take 1 dose of the drug every 3-6 hours, but no more than 5 doses within 24 hours. eleven
What you need to know about taking antibiotics?
Author of the article: Lavrishchev Alexander Alexandrovich, therapist
1. What are the purposes of antibiotics and what are they not for?
Antibiotics are medications that inhibit the growth and/or reproduction of bacteria in your body. They are not effective against viral infections, nor for those conditions where the infection is an apparent thing. For example, some people after a myocardial infarction may develop a condition similar to pneumonia (inflammation of the lungs), but this is not associated with infection - in this case, the patient's immune system will attack the lung tissue that it was originally supposed to protect: the use of an antibiotic is pointless, it is necessary other groups of drugs.
2. How to take an antibiotic correctly?
First of all, the best antibiotic is the one you didn't take. Of course, you will encounter bacterial infections from time to time in your life, and sometimes you will need help dealing with them. However, today in our country it is customary to prescribe antibiotics “right and left,” which clearly contradicts common sense. Therefore, when choosing a good doctor for yourself, you are choosing a medicine in which antibiotics are used less often in general, and not because they are somehow terrible, but because the reasons for their use are not so common. Secondly, each course of antibiotic treatment must be strict in duration: even if you feel better the very next day of taking the drug, continue treatment exactly until the day the doctor prescribed for you. Usually this is 5-7 days of treatment, but it can be more or less. The fact is that if the course of treatment is interrupted, the bacteria inside you may become resistant to the drug and the next time you need the help of this medicine, it will not be effective. You can also pass on antibiotic-resistant bacteria to another person, which entails unnecessary risks: for example, the doctor will not immediately understand that the medicine is not helping, and the person will be sick longer. The problem of bacterial resistance to antibiotics is so pressing for the entire planet that scientists are sounding the alarm because the industry is unable to produce new antibiotics, and people's lives are at risk. Thirdly, the remaining nuances of taking an antibiotic depend only on the instructions of your attending physician: he will recommend that you take the drug before or after meals, indicate the number of doses of the drug on each day of use, and so on.
3. What should I take with the antibiotic?
It would be more correct to say that you shouldn’t drink it. Of course, you should not take the antibiotic with alcohol. There are also nuances with other drinks: in pharmacology there is another drink that can play a cruel joke on you, and it is not very obvious at first glance. This is grapefruit juice. The fact is that grapefruit juice contains substances that affect liver enzymes involved in the neutralization of drugs. Therefore, when taking certain medications and grapefruit juice at the same time, the medications may not work as intended by doctors - for example, they may be quickly eliminated from the blood, or, on the contrary, remain there longer than usual, which can lead to poisoning. Otherwise, you should use plain water at room temperature to take medications. By the way, special forms of administration have been developed for some antibiotics - they are called “Solutab” (for example, “Flemoxin Solutab”); at the same time, you can swallow the tablet and wash it down with water, or you can dissolve the tablet in water and drink the resulting solution (a pleasant or acceptable taste - scientists have taken care of this), which is very convenient for small children and older people, as well as for those who may have difficulty swallowing tablets. Solutab forms work as effectively as, for example, intravenous injections of the drug, so the need for antibiotic injections at home today is a relic of the past.
4. Do I need to take prebiotics and antifungals at the same time?
NO NEED. From a scientific point of view, prebiotics (medicines that contain cultures of live bacteria that inhabit the intestines) work only in television advertising and in the wallets of pharmacy owners: the bacteria that you take from the prebiotic are also killed by the antibiotic, and that in patients taking prebiotics diarrhea does not develop - this is the merit of scientists and pharmacologists who come up with antibiotics and make them safer. If you take a prebiotic, your chance of getting diarrhea is exactly the same as if you didn't take it. Please keep in mind that such diarrhea will not be treated with prebiotics, but (!) with other antibiotics - so just consult your doctor. As for antifungal drugs, many patients have an established opinion that they will definitely develop thrush in response to taking an antibiotic - and indeed, sometimes this happens. However, there are many pitfalls here: first, antifungal drugs are one of the most toxic drugs today, and second, thrush is not some kind of infection following an antibiotic. This is a disease of your immunity, which normally should itself suppress the activity of fungi, so you need to deal with the immune system, and not endlessly take not the safest drugs.
5. What to do if you miss a pill?
Modern antibiotics are typically taken once a day, so take your dose as soon as possible after you remember you missed it. If you need to take an antibiotic several times a day, just take the next dose of the drug.
6. What are the side effects of antibiotics?
Variety. Firstly, these are allergic reactions to taking the drug, and no one is immune from this. Usually your doctor should ask you if you are allergic to a particular antibiotic, and do not forget to remind the doctor that you are allergic to antibiotics or even other drugs - sometimes this is also important when choosing an antibiotic. Secondly, some antibiotics can affect heart rhythm, so if you have arrhythmia, ask your doctor if your drug will affect your heart disease. Third, some antibiotics are more likely to cause diarrhea than others. However, modern antibiotics affect the intestines less and less, since scientists have provided various protection systems - most drugs either hardly reach the intestines, or do not act on the intestinal mucosa, where the “maternity hospitals” of your bacteria are located, so after taking the drug - your own bacteria They will restore everything themselves. Keep in mind that if you are afraid of diarrhea, antibiotic injections are more likely to cause diarrhea, since the medicine enters the bloodstream more massively, affecting all layers of the intestine along its entire length.
7. What to do if an allergic reaction develops?
Stop taking the drug and contact your doctor as soon as possible. If you feel very unwell—for example, swelling of your neck, face, mouth, and/or difficulty breathing—call 911 immediately. If you have an allergic reaction to an antibiotic, this does not mean that all antibiotics will work the same, you just need to change the drug.
8. Is it safe to take an antibiotic together with other drugs?
This should only be decided by your doctor. Most good doctors today have in their pocket access to specialized databases that help assess the interactions of a wide variety of drugs, and the risks of combining them. The only thing is that antibiotics should not be taken with sorbents - substances that supposedly absorb toxins from the intestines - such as enteral gels or activated carbon: along with the mythical toxins, these drugs will absorb the antibiotic itself, and then go down the toilet with it and your money.
9. What to do to avoid antibiotic resistance?
Antibiotic resistance is a condition in which the bacteria in your body become resistant to the action of an antibiotic, as we discussed above. Again, always take the antibiotic for as many days as your doctor prescribes. Second: do not use the same antibiotic more than once every 6 months, so if you need to take an antibiotic again less than 6 months after the last course, tell your doctor about it, and he will prescribe you a drug from a different group. LAST: Never prescribe an antibiotic yourself!
10. What are they doing now to cope with this problem?
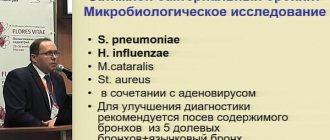
Firstly, it is now difficult to buy an antibiotic without a doctor's prescription - and this is absolutely true: antibiotics should be used only when necessary, and only a doctor can deal with this. Secondly, guidelines are constantly being published for doctors on how to properly treat a particular infection: which antibiotics should be used more often and which ones should not be used at all. Thirdly, good doctors use bacteriological research methods before prescribing you a drug - for example, the doctor will ask you to take a sputum or throat swab before a course of drug treatment. A microbiologist in the laboratory will try to isolate a bacterial culture from your biomaterial and test it for sensitivity to antibiotics - therefore, in case of possible failure, the doctor will already be armed with information on how to accurately treat the infection. The downside is that this study takes 5-7 days, and you need to be treated today. Fourthly, scientists and pharmacologists are constantly coming up with methods to protect against antibiotic resistance: they invent new molecules, and also add adjuvants to antibiotics - substances, for example, that prevent bacteria from breaking down the antibiotic.
11. What alternatives to antibiotics are there now?
There are few such alternatives, and yet they are exotic and not always available. Firstly, these are bacteriophages - viruses that destroy certain bacteria. A solution of such a bacteriophage can treat mild infections - sometimes by taking this solution orally, and sometimes by washing the affected area with it. For the nose, of course, this is very uncomfortable. In addition, bacteriophages are active strictly against certain bacteria, they are rarely found, and in general they are justifiably unpopular. It probably doesn’t make sense to treat an acute infection with them - more time will be spent searching. However, some chronic infections are treated with them, especially in people with multiple allergies to antibiotics, which, fortunately, is extremely rare. Secondly, scientists are now looking at different classes of substances that exhibit antimicrobial activity, for example, odorous substances from plants - like those found in pine needles or garlic. However, this is just a project for now. THE MOST IMPORTANT ALTERNATIVE TO AN ANTIBIOTIC IS A GOOD DOCTOR who will not prescribe you an antibiotic for no reason! Without understanding how to make your course of treatment better and easier!
Making an appointment with a general practitioner
To clarify the details, consult a qualified specialist at the Semeynaya clinic.
Single contact center
8 495 662-58-85
daily from 8 to 21
To find out more about prices for seeing a therapist or other questions, please follow the link below:
Therapy