Drastop solution IM 100 mg/ml 2 ml x10
Trade name: DRASTOP
International name: Chondroitin sulfate (Chondroitin sulfate)
Pharmacological group: tissue repair stimulator
Pharmacological group for ATC: M01AX25. Chondroitin sulfate
Pharmacodynamics:
High molecular weight mucopolysaccharide that slows down bone resorption and reduces Ca2+ loss. Improves phosphorus-calcium metabolism in cartilage tissue, accelerates its restoration processes, and inhibits the processes of degeneration of cartilage and connective tissue. Suppresses enzymes that cause damage to cartilage tissue, stimulates the synthesis of glycosaminoglycans, promotes the regeneration of the joint capsule and cartilaginous surfaces of the joints, and increases the production of intra-articular fluid. Due to its structural proximity to heparin, it prevents the formation of fibrin blood clots in the synovial and subchondral microvasculature. Reduces pain and increases mobility of affected joints.
Gel, ointment: slows the progression of osteoarthritis. DMSO, which is part of ointment forms, has anti-inflammatory, analgesic and fibrinolytic effects, promotes better penetration of chondroitin through cell membranes.
Pharmacokinetics:
Gel, ointment: practically no systemic absorption.
For tablets, capsules, solution for injection, lyophilisate for preparation of solution for injection: with a single oral dose of TCmax in plasma - 3-4 hours, in synovial fluid - 4-5 hours. Bioavailability - 13%.
30 minutes after intramuscular administration it is found in the blood in significant concentrations, and after 15 minutes - in the synovial fluid. TCmax - 1 hour, then the concentration of the drug slowly decreases over 2 days.
It accumulates mainly in cartilage tissue (the maximum concentration in articular cartilage reaches after 48 hours), the synovial membrane is not an obstacle to its penetration into the joint cavity.
Excreted by the kidneys within 24 hours.
Indications for use:
Ointment and gel: degenerative-dystrophic diseases of the joints and spine - primary arthrosis, osteoarthrosis with predominantly damage to large joints, intervertebral osteochondrosis, osteoporosis, periodontopathy, bone fractures (to accelerate the formation of bone tissue).
Powder for preparing a solution for external use: to accelerate reparative processes in long-term non-healing wounds, trophic ulcers, bedsores (in the granulating stage).
Tablets, capsules, solution for injection, lyophilisate for preparing solution for injection: degenerative-dystrophic diseases of the joints and spine: primary arthrosis, osteoarthrosis with predominant damage to large joints, intervertebral osteochondrosis.
Contraindications:
Hypersensitivity, acute inflammatory processes in the wound area, widespread tissue necrosis, excessive granulation, violation of the integrity of the skin at the sites of intended application,
children's age (efficacy and safety have not been established).
Carefully:
Pregnancy, lactation period, age up to 18 years.
Tablets, capsules, solution for injection, lyophilisate for preparing solution for injection: bleeding and tendency to bleeding, thrombophlebitis.
Dosage regimen:
Externally: apply 2-3 times a day to the skin over the lesion and rub in for 2-3 minutes until completely absorbed. The course of treatment is 2-3 weeks. If necessary, the course of treatment is repeated.
Powder for preparing a solution for external use: immediately before use, add 5 ml of 0.5% procaine solution or 0.9% sodium chloride solution to a bottle containing 50 mg of powder for preparing a solution for external use. The contents of the bottle are thoroughly shaken. The resulting viscous solution is distributed on the surface of a two-layer sterile gauze napkin and applied to the wound, and a regular gauze bandage is applied on top. Dressings are performed once every 2-3 days. The duration of treatment, depending on the course, is 10-30 days.
Tablets, capsules, solution for injection, lyophilisate for the preparation of solution for injection: orally, intramuscularly.
Orally: adults - 0.75 g 2 times a day for the first 3 weeks, then - 0.5 g 2 times a day. Capsules are taken with a small amount of water.
IM: 0.1 g every other day, if well tolerated, the dose is increased, starting from 4 injections, to 0.2 g. The course of treatment is 25-35 injections. Repeated course - after 6 months.
Side effects:
Ointment, gel, powder for preparing a solution for external use: allergic reactions.
Tablets, capsules, solution for injection, lyophilisate for preparing solution for injection: allergic reactions, hemorrhages at the injection site.
Interaction:
Tablets, capsules, solution for injection, lyophilisate for preparing solution for injection: the effect of indirect anticoagulants, antiplatelet agents, fibrinolytics may be enhanced, which requires more frequent monitoring of blood coagulation parameters when used together.
Special instructions:
If the scarring of the wound edges is severe and there is excessive granulation, the drug can be used after treatment with drugs containing hyaluronidase.
Avoid contact of ointment and gel with mucous membranes and open wounds.
Description connected via INN
Instruction update date 10/27/2015
Manufacturer: SCRompharm Company SRL, Romania
Marketing Authorization Holder: World Medicine Ltd, UK
Release form: solution for intramuscular administration 100 mg/ml, ampoules
Dispensing conditions: by prescription
State data registration: LP-003472 dated 02/26/2016
Status of the registration certificate: expiration date 02/26/2021
The effectiveness of Drastop in the treatment of chronic back pain
The results of a study of the effectiveness and tolerability of chondroitin sulfate (Drastop) in the complex treatment of patients with chronic back pain are presented. All patients (n = 50) received standard therapy, including nonsteroidal anti-inflammatory drugs and muscle relaxants. Patients of the main group (n = 30) were additionally prescribed Drastop in the first three days, 1 ml every other day, then 2 ml every other day, for a total of 25 injections. The control group (n = 20) did not receive treatment with chondroprotectors. The groups were comparable in terms of clinical manifestations of dorsopathy, age, and examination results. After the therapy, the patients of the main group decreased the severity of pain, increased mobility of the spinal column and improved functional capabilities, and the positive effect increased within two months after the end of treatment. Drastop did not have a negative impact on the subjective status of patients. Its use was not accompanied by the occurrence of side effects. The drug was well tolerated, improving the clinical course of the disease and increasing the effectiveness of the therapy.
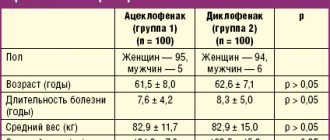
Table 1. Severity of pain syndrome according to the visual analogue scale
Table 2. Dynamics of Oswestry questionnaire indicators
Introduction
Back pain is one of the most common complaints in the clinical practice of doctors of various specialties. According to various sources, 49–90% of the population experiences at least one episode of back pain during their lifetime [1]. In the majority of patients, pain resolves in a short time (up to two weeks). Thus, an analysis of the effectiveness of treatment of 280 patients on an outpatient basis showed that the average duration of pain in radiculopathy was 13.8 days, and in nonspecific dorsopathies – 11.2 days [2]. However, repeated episodes of back pain developed in 20–44% of such patients within a year, and in the future – in more than 3/4.
Back pain leads to significant socio-economic losses associated with temporary disability, as well as in 10% of cases with disability [3].
Acute lumbar pain is most often caused by a non-life-threatening disease, but diagnostic algorithms are based on the need to exclude specific causes, since such situations require emergency treatment, otherwise the prognosis for recovery is significantly worse [4]. Inadequate treatment of even nonspecific back pain with a favorable prognosis worsens the prognosis, causes its chronicity, and reduces the patient’s quality of life.
The reasons for the development of dorsopathies are very diverse. Risk factors include genetic predisposition, female gender, middle age, various anamnestic spinal injuries, inadequate physical overload, activities associated with staying in a forced and unphysiological position for a long time, smoking, excess weight, physical inactivity, etc. [5]. Most often, vertebrogenic dorsopathies are based on spinal osteochondrosis - a degenerative-dystrophic process in the intervertebral discs, involving the bodies of adjacent vertebrae, intervertebral joints and ligaments [6].
Initially, the process affects the nucleus pulposus of the intervertebral disc, which, due to loss of moisture, ceases to perform physiological functions and loses elasticity. Under the influence of various mechanical factors, sequesters can form, and the nucleus begins to protrude in the direction of the fibrous ring of the disc. Over time, cracks appear in the annulus fibrosus. A defective disc can sag into the lumen of the spinal canal (forming disc prolapse), and fragments of the nucleus pulposus, penetrating through cracks in the annulus fibrosus, form disc herniations. The described processes in at least one spinal segment contribute to the development of reactive changes on the part of neighboring vertebrae and intervertebral joints, as a result of which the functional state of the entire spinal column begins to suffer. Along with this, the pathological process may involve the ligamentum flavum, which will begin to thicken and put pressure on the root and membranes of the spinal cord. Subsequently, stabilization may occur due to disc fibrosis [6].
With all the variety of factors contributing to the development of dorsopathies, most often two main aspects lead to the formation of this pathology: dysfunction of the trophic systems and overload of the spinal motion segments [5, 6]. Limited overloads of spinal motion segments develop against the background of exogenous (overloads in everyday life, at work) and endogenous (constitutional features of the musculo-ligamentous apparatus) reasons. All these factors underlie the destruction of cartilage tissue involving the intervertebral discs and intervertebral joints.
Cartilage tissue is one of the types of connective tissue that looks like a gel. The thickness of the cartilage is determined by the type of joint and its functional purpose and ranges from 1–7 mm. Articular cartilage is a highly specialized cartilaginous tissue covered with perichondrium, which ensures the sliding of articular surfaces against each other, as well as equal distribution of load under local influence, which reduces the traumatic effect during movement. The cartilage tissue of the intervertebral discs consists of movable parallel-directed collagen bundles (up to 97%), which, gradually loosening, pass into hyaline cartilage. In addition to collagen fibers, the intercellular substance of cartilage tissue, or extracellular matrix, consists of water (up to 70%), hyaluronic acid and proteoglycans (about 10–20%). The composition of this matrix determines the properties of articular cartilage. The structure of proteoglycan determines its high hydrophilicity, which, combined with low viscosity, makes it an ideal structure for counteracting joint loads. When assessing the function of articular cartilage, it is necessary to pay attention to the fact that it provides elasticity, stability under load, and elasticity during movement.
Cartilage is nourished passively from the synovial fluid and vessels of the underlying bone. As the body ages, the concentration of proteoglycans and the associated hydrophilicity of the tissue in cartilage decreases. The process of formation of chondroblasts and young chondrocytes slows down. To date, it has been proven that the metabolism of cartilage tissue is anaerobic in nature. This explains the low intensity of metabolic processes in mature tissue, therefore the compensatory capabilities of cartilage tissue are very limited, and defects in articular cartilage are practically not compensated, but are only replaced by fibrous cartilage, which has a low density. Changes in collagen, the main substance, a decrease in the number of elastic fibers in ligaments and tendons, muscle atrophy, and the growth of connective tissue in them aggravate functional disorders in the joints [7].
The main goals of treatment and rehabilitation of patients with dorsopathies include relief of clinical manifestations of the disease (relieving pain, increasing mobility of the spinal column), improving self-care and quality of life. To resolve these issues, a wide range of means are used, both medicinal (non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, B vitamins, drugs that improve nerve fiber conduction, vasoactive drugs) and non-medicinal (various types of physical therapy, physiotherapy, reflexology, manual therapy, shock wave therapy) [5, 7, 8]. When the pain syndrome becomes chronic, those methods of therapy and rehabilitation that can prevent exacerbation of the disease and slow down the processes of degenerative-dystrophic progression in the spinal column come to the fore. Among them are various methods of physical therapy that allow the formation of an adequate muscle corset, correction of psychological status, and training in the correct motor pattern [8, 9].
NSAIDs play an important role in relieving pain in spinal diseases [9, 10]. According to the results of a meta-analysis, NSAIDs are effective for both acute and chronic back pain [9] and should therefore be used as first-line therapy. It should be noted that NSAIDs are especially effective in the early stages. For acute pain, non-narcotic analgesics and muscle relaxants are also prescribed [9]. When pain is chronic, when central pathophysiological mechanisms are activated, NSAID monotherapy is not always effective [9, 10]. Long-term use of analgesic and anti-inflammatory drugs may reduce the severity of discomfort, but will not delay the destruction of cartilage tissue, and therefore will not slow down the further progression of the disease. A patient taking analgesics, which reduce pain, often exceeds the permissible load on the spinal column, which can aggravate destructive changes and contribute to the rapid progression of the disease [10]. Therefore, when the disease is chronic, the most promising is considered to be a combination of drug therapy (NSAIDs, muscle relaxants, chondroprotectors, antidepressants) with physical therapy, manual and cognitive behavioral psychotherapy [10].
Structure-modifying (chondroprotective, chondromodulating) agents can influence the course of the disease by correcting metabolic disorders of hyaline cartilage. Chondroprotectors promote the regeneration of cartilage tissue by restoring chondrocytes and connective tissue. Chondroprotective drugs suppress the activity of enzymes that lead to disc degeneration and simultaneously stimulate regeneration processes. Their use slows down degenerative processes in the spine and reduces the risk of chronic pain. Preparations with structure-modifying properties include chondroitin, glucosamine, combined preparations of chondroitin sulfate and glucosamine, soybean and avocado unsaponifiables, hyaluronic acid preparations, strontium ranelate, ginger (standardized preparation of Zingler officinale
and
Alpinia galanga
) and estrogens [9]. The most studied and used today are chondroitin and glucosamine.
Chondroitin sulfate is a group of compounds that have different molecular weights and specific gravity. Their mechanism of action is based on the ability to store water inside the cartilage in the form of water cavities, creating adequate shock absorption and softening shocks, which increases the strength of the connective tissue. The effectiveness of chondroitin sulfate has been proven in various studies [5].
The pharmacological effect of the use of chondroitin sulfate is determined not only by chondroprotective, but also by anti-inflammatory and analgesic effects, which also stimulates the regeneration of cartilage tissue. The pharmacodynamic feature of chondroitin sulfate is the ability to prevent the destruction of macromolecular structures of normal tissues and activate regeneration processes in interstitial tissue and articular cartilage, which explains its analgesic effect. The anti-inflammatory mechanism and the regeneration mechanism are based on the suppression of hyaluronidase activity and activation of hyaluronic acid synthesis.
Among the chondroprotectors, which include chondroitin sulfate, which affects phosphorus-calcium metabolism in cartilage tissue, Drastop should be noted. Drastop is indicated for primary and secondary osteoarthrosis of various localizations (coxarthrosis, gonarthrosis, arthrosis of small joints), osteochondrosis and spondylosis. Summarizing the experience of using Drastop in clinical practice, we conducted an observation using Drastop and further assessing the dynamics of the clinical symptoms of widespread osteochondrosis, the severity of pain and the quality of life of patients.
Purpose of the study
To determine the possibilities of using Drastop as a metabolic and analgesic agent in patients with back pain against the background of traditional therapy, including NSAIDs and muscle relaxants, and to assess its tolerability.
Material and methods
The study included 50 patients with chronic pain syndrome in the lower back lasting at least three months under the conditions of informed consent. The pain syndrome was not due to specific causes (infectious lesions, oncopathology, systemic lesions). Degenerative-dystrophic changes in the spine were confirmed by the results of radiography, computed tomography or magnetic resonance imaging.
The main group included 30 people (18 women and 12 men, average age 39.4 ± 9.8 years). In 15% of patients, protrusion of the intervertebral disc without root compression was found, in 26% - facet joint syndrome, in 12% - radiculopathy caused by disc herniation. The control group consisted of 20 patients (seven men and 13 women, mean age 41.7 ± 9.3 years). There were no significant differences between the groups in such indicators as age, duration of the disease, or severity of symptoms.
All patients in both groups were allowed to take NSAIDs at a stable dose in combination with muscle relaxants. In addition, patients in the main group were administered Drastop intramuscularly according to the following regimen: in the first three days, 1 ml every other day, then 2 ml every other day, for a total of 25 injections.
The effectiveness of the drug was assessed using a visual analog scale and the Oswestry questionnaire before the start of the study, after completion of the injection course and two months after the end of treatment. Statistical data processing was performed using the statistical software package Statistica 6.0 using the Mann–Whitney test for two unrelated samples.
Results and its discussion
During treatment, patients in both groups noted some reduction in pain and improvement in condition, but in the group of patients receiving Drastop, the severity of positive changes was more pronounced (Table 1). The therapeutic effect of the drug appeared already at the end of the course of injection therapy and continued to increase for two months after the end of treatment.
Before the start of therapy, almost all patients noted disturbances in all subscales of the Oswestry questionnaire, reflecting the quality and completeness of life (habitual daily activities, self-care, mobility, quality of sleep, sexual life). In addition to reducing the severity of pain, the use of the drug also led to an improvement in the quality of life, normalization of sleep, an increase in the volume of daily activities, and a more active lifestyle (Table 2).
According to the Oswestry questionnaire, patients showed positive dynamics in their general health (physical, psychological and social components), as evidenced by an improvement in the performance of everyday activities such as dressing, personal care, getting up, personal hygiene, and walking. Moreover, the positive effect increased within two months after the end of treatment. No side effects were observed during the use of Drastop.
Our study of the effectiveness of Drastop showed that in patients with chronic back pain, the drug helped reduce the severity of pain, increase the mobility of the spinal column and improve functionality. The sufficient analgesic effect, which was obtained over a short period, indicates that the components of Drastop have not only structure-modifying, but also anti-inflammatory properties [5].
One of the results of the observation was a significant decrease in the degree of impairment of functional abilities of patients during treatment, assessed on the Oswestry scale. This is of great importance for the speedy return of patients to normal daily physical activity and prevents chronic pain syndrome [5]. It is known that chronic back pain, prolonged bed rest, and refusal of physical activity negatively affect the restoration of activation and the weakening of the severity of pain.
conclusions
Treatment with Drastop contributed to a significant reduction in the severity of pain in patients with chronic back pain. The analgesic effect continued to increase within two months after the end of treatment. With the use of Drastop, a significant improvement in the motor functions of patients was also noted, which is important for the prevention of chronic pain syndrome. Drastop can be recommended as an effective remedy as part of complex therapy for chronic back pain.