Decoding the results is the competence of a pediatrician, therapist or specialist, since it is important not only to analyze the numbers, but also to compare deviations from the norms of different indicators, to compare the information obtained during examination and history taking. To have an overview and be prepared when you see your doctor, learn what blood elements are tested in the laboratory, how to interpret the results, and what abnormalities may mean.
Types of leukocytes
The leukocyte formula reflects the ratio of five main types: lymphocytes, monocytes, neutrophils, basophils, eosinophils. Different types of white blood cells are different in structure and purpose. Depending on whether they contain granules that are capable of perceiving color, leukocytes are of two types: granulocytes, agranulocytes.
Granulocytes include:
- basophils - can perceive alkaline color;
- eosinophils – acidic;
- neutrophils - both types of dyes.
Agranulocytes include:
- two types of lymphocytes (B- and T-lymphocytes);
- monocytes.
What do granulocytes say?
Part of the leukocytes are granulocytes, which get their name due to the presence of granules. There are three types of cells: neutrophils, eosinophils and basophils. The types of granulocytes differ from each other due to the color of the granules and the structure of the nucleus.
The granules store immune substances that are important for protecting the body. Thanks to them, cells participate in inflammatory processes. The job of granulocytes is to absorb proteins and chemicals. Granulocytes also digest them.
The cells mature in the bone marrow, where the resulting quantity is stored for another 3-4 days. Mature cells enter the blood, where they circulate for 6 hours. After the end of the cycle, granulocytes enter the tissues, where they perform their functions.
The largest number of leukocytes are neutrophils, of which there are always about 1010 in the blood. If a bacterial infection enters the body, neutrophilia begins - an increased amount of neutrophils in the blood. The number of cells that appear depends on the number of harmful bacteria.
The duration of stay of neutrophils in the body is only 4 days, which is why still immature cells (band cells, metamyelocytes, and others) enter the body. This phenomenon is called a “shift of the leukocyte formula to the left.” With neutropenia (reduced number of neutrocytes), the body is less protected from infections.
About 5% of leukocytes are eosinophils, the number of which depends on adrenal hormones. In the morning there are the largest number of them. They are stored in the layer under the mucous membrane of the gastrointestinal tract. A quantity above the norm indicates that the following processes are occurring in the body:
- Infestation with parasites;
- Allergy;
- Autoimmune processes.
Medical offers to sign up for diagnostics and tests. In our laboratory it is possible to take all types of tests in Tula. Tel. for recording.
The smallest number (less than 1%) are basophils. They play a role in the release of histamine during allergic reactions. It is these cells that are responsible for itching, redness, irritation and bronchial spasms.
Depending on the location of basophils in the body, the following reactions differ:
- Bronchial asthma;
- Rashes
- Hives;
- Quincke's edema (swelling of the larynx).
Functions of white cells
Lymphocytes. T lymphocytes destroy foreign microorganisms and cancer cells. B lymphocytes are responsible for producing antibodies.
Monocytes. They participate in phagocytosis, directly neutralizing foreign bodies, as well as the immune response and tissue regeneration.
Eosinophils. Capable of active movement and phagocytosis. They actively participate in the formation of inflammatory and allergic reactions, capturing and releasing histamine.
Basophils. They ensure the migration of other types of leukocytes into tissues to the site of inflammation and take part in allergic reactions.
Neutrophils. The main purpose is phagocytic protection, that is, the absorption of foreign bodies. In addition, they release bactericidal substances.
Normal leukogram values
The leukocyte formula of the blood of healthy adults is as follows:
| Kinds | Content % | Absolute value (number of cells X 10?/l) |
| Lymphocytes | 19-37 | 1,2-3 |
| Monocytes | 3-11 | 0,09-0,6 |
| Band neutrophils (immature) | 1-6 | 0,04-0,3 |
| Segmented neutrophils | 47-72 | 2-5,5 |
| Basophils | 0-1 | 0-0,065 |
| Eosinophils | 0,5-5 | 0,02-0,3 |
Changes in the leukogram are usually denoted by terms with specific endings. As the level increases, endings such as “oz” (“ez”) or “ia” are added to the name of a particular type of leukocyte. For example: lymphocytosis, eosinophilia, monocytosis, etc. When the level of leukocytes decreases, it is customary to add the ending “singing” to the name: lymphopenia, neutropenia, eosinopenia, etc.
In this case, a distinction is made between relative and absolute change. In the first case, we are talking about a deviation from the norm in the percentage of leukocytes. In the second, they talk about a deviation from the norm both in percentage terms and in absolute terms, which is understood as a change in the total number of cells per unit volume of blood.
Leukocytes differ in their structure and purpose
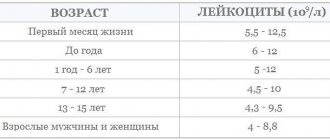
It should be said that the leukocyte formula depends on age. This must be taken into account when assessing it during examination and diagnosis of diseases in children.
The norm of lymphocytes in the blood in adults and children
Unfortunately, there are often situations when lymphocytes in the blood can deviate from the norm - increase or decrease. This can happen in various situations. Before we talk about when the number of lymphocytes changes in the blood, we need to talk about how much is their normal component.
If we talk about cell clones, then:
T cells make up 75% of the total number of lymphocytes;
B cells about 15%;
Natural killers are about 10%.
And speaking about the norms of lymphocytes, it must be said that at different periods of a person’s life the norms differ.
Lymphocytes begin to be produced by the bone marrow already in utero, and this process continues throughout life. The lifespan of these cells also varies - from several months to sixty years. And these will all be lymphocytes.
- Up to 1 year, the content of lymphocytes in the blood of the total number of all cells is 45-70%.
- From 1-2 years, the concentration of lymphocytes should decrease - somewhere around 39-60%.
- From 2-4 then somewhere from 33-50% of all white cells.
- From 4-10 years, already 30-50%.
- From 10-18 years old, then this is already 30-44%.
- In an adult, lymphocytes in the blood should range from 19-37%.
The table shows the values of acceptable norms of lymphocytes (individual subpopulations) in the blood of children and adults.
| Age | Proportion of the total number of lymphocytes, % | Absolute cell count, *106/l |
| CD 3+ (T lymphocytes) | ||
| Up to 3 months | 50 – 75 | 2065 – 6530 |
| Up to 1 year | 40 – 80 | 2275 – 6455 |
| 1 – 2 years | 52 – 83 | 1455 – 5435 |
| 25 years | 61 – 82 | 1600 – 4220 |
| 5 – 15 years | 64 – 77 | 1410 – 2020 |
| Over 15 years old | 63 – 88 | 875 – 2410 |
| CD3+CD4+ (T helper cells) | ||
| Up to 3 months | 38 – 61 | 1450 – 5110 |
| Up to 1 year | 35 – 60 | 1695 – 4620 |
| 1 – 2 years | 30 – 57 | 1010 – 3630 |
| 25 years | 33 – 53 | 910- 2850 |
| 5 – 15 years | 34 – 40 | 720 – 1110 |
| Over 15 years old | 30 – 62 | 540 – 1450 |
| CD3+CD8+ (T-cytotoxic lymphocytes) | ||
| Up to 3 months | 17 – 36 | 660 – 2460 |
| Up to 1 year | 16 – 31 | 710 – 2400 |
| 1 – 2 years | 16 – 39 | 555 – 2240 |
| 25 years | 23 – 37 | 620 – 1900 |
| 5 – 15 years | 26 – 34 | 610 – 930 |
| Over 15 years old | 14 – 38 | 230 – 1230 |
| CD19+ (B lymphocytes) | ||
| Up to 2 years | 17 – 29 | 490 — 1510 |
| 25 years | 20 – 30 | 720 – 1310 |
| 5 – 15 years | 10 – 23 | 290 – 455 |
| Over 15 years old | 5 – 17 | 100 – 475 |
| CD3-CD16+CD56+ (NK cells) | ||
| Up to 1 year | 2 – 15 | 40 – 910 |
| 1 – 2 years | 4 – 18 | 40 – 915 |
| 25 years | 4 – 23 | 95 – 1325 |
| 5 – 15 years | 4 – 25 | 95 – 1330 |
| Over 15 years old | 4 – 27 | 75 – 450 |
| Over 15 years old | 1 – 15 | 20-910 |
How to determine
The leukocyte formula is calculated by a laboratory assistant by viewing the blood under a microscope (leukogram count per hundred cells).
In addition, a hematology automatic analyzer is used. In case of deviations from the norm, a microscopic examination of the smear is additionally carried out, while the morphology of the cells is described and the leukogram is clarified.
The use of automatic equipment allows you to obtain the most accurate result: more than 2000 cells can be analyzed, while under a microscope - a maximum of 200. When examined using an analyzer, the result is more objective.
Automatic counting also has a drawback: the inability to divide neutrophils into segmented and band neutrophils. But in the case of a large number of young forms, the equipment records a shift to the left.
Preparing for analysis
In order for the leukogram to be the most accurate and reliable, the patient should properly prepare for the test.
- Venous blood is collected in the morning and on an empty stomach (more than 10 hours pass between the last meal and analysis). A few hours before the procedure, you are allowed to drink a glass of plain water;
- On the eve of the procedure (3 days before), it is necessary to remove fatty, smoked, spicy foods, tonics (coffee, strong tea, energy drinks) and alcoholic drinks from the diet;
- 1-2 hours before the analysis, smoking (tobacco, cigarettes, hookah), lifting weights, performing active activities and being nervous is prohibited.
After blood is taken from a vein, the material is sent to the laboratory for testing. There, a specialist determines the ratio of white cells under a microscope and compiles a leukocyte formula. Additionally, an automatic analyzer is used to obtain results.
Reasons for changes in leukogram
An increase in the level of lymphocytes (lymphocytosis) is observed in the following pathologies:
- acute viral infections: chickenpox, measles, mononucleosis, rubella;
- chronic bacterial infections: syphilis, brucellosis, tuberculosis;
- lymphomas, lymphosarcoma, lymphocytic leukemia;
- hyperthyroidism (thyrotoxicosis);
- adrenal insufficiency;
- folate deficiency anemia;
- aplastic and hypoplastic anemia.
Lymphocytopenia can develop for the following reasons:
- acute infections;
- lymphogranulomatosis;
- systemic lupus erythematosus;
- renal failure;
- immunodeficiency;
- radiation sickness (acute form);
- taking corticosteroids.
An increase in the level of neutrophils in the blood (neutrophilia) is observed in the following conditions:
- bleeding is acute;
- intoxication;
- bacterial diseases in acute forms;
- taking corticosteroids;
- tissue necrosis.
The content of neutrophils decreases for the following reasons:
- bacterial infections: typhoid fever, brucellosis, tularemia;
- viral infections: measles, hepatitis, rubella;
- toxic effects to which the bone marrow is exposed: drugs, ionizing radiation;
- autoimmune diseases;
- hypersensitivity to medications;
- Benign chronic neutropenia is hereditary.
Monocytosis, in which the level of monocytes in the blood is increased, may indicate the following disorders:
- subacute, chronic infections caused by bacteria;
- hemoblastoses;
- systemic autoimmune diseases: rheumatoid arthritis, lupus erythematosus, sarcoidosis;
- parasitic infections.
A low level of monocytes is assessed in combination with lymphocyte indicators, which is important when diagnosing pulmonary tuberculosis.
Basophilia (increased levels of basophils in the blood) is observed in chronic myeloid leukemia and erythremia.
An increased level of eosinophils is observed in the following conditions:
- allergies;
- Loeffler's endocarditis;
- scarlet fever;
- parasitic infections;
- chronic skin diseases: eczema, psoriasis;
- eosinophilic leukemias;
- recovery phase of infectious diseases.
Causes of low eosinophil levels (eosinopenia) may include:
- typhoid fever;
- increased adrenocorticosteroid activity.
Lymphocytes are higher than normal in children
In children 4-5 days and 4-5 years of age, physiological lymphocytosis is observed in the blood, which does not require treatment. The child’s condition remains completely normal, the lymph nodes do not enlarge. This situation is due to the restructuring of the child’s hematopoietic system.
However, an increased lymphocyte count in children may be caused by:
- Leukemia;
- Bronchial asthma;
- Infection: influenza, ARVI, sore throat and others;
- Purulent-inflammatory processes;
- Viral diseases: lichen, whooping cough, malaria, varicella (chickenpox), measles, viral hepatitis and others.
Lymphocytes can also be elevated during other diseases, with various individual characteristics of the body. The exact reasons can only be determined after a full examination.
Leukogram shift
Modern automatic blood analyzers quickly and accurately calculate the complete leukocyte formula, which greatly facilitates diagnosis
When the leukogram is deciphered, nuclear shifts are taken into account. These are changes in the ratio of mature and immature neutrophils. In the blood formula, the different forms of neutrophils are listed in order from young to mature (from left to right).
There are three types of shifts: left, left with rejuvenation, and right.
With a left shift, myelocytes and metamyelocytes are present in the blood. This change occurs through the following processes:
- acute inflammation: pyelonephritis, prostatitis, orchitis;
- purulent infections;
- acidosis;
- bleeding is acute;
- poisoning with toxins;
- high physical activity.
With a left shift with rejuvenation, forms such as myelocytes, metamyelocytes, promyelocytes, myeloblasts, and erythroblasts can be found in the blood. This is observed in conditions such as:
- leukemia (chronic, acute);
- erythroleukemia;
- metastases;
- myelofibrosis;
- coma.
Video about the types and functions of leukocytes:
With a decrease in the number of band (immature) neutrophils and an increase in the level of segmented (mature forms containing 5-6 segments), they speak of a right shift. With such a change in the leukogram, we can talk about the following pathologies and conditions:
- liver and kidney diseases;
- megaloblastic anemia;
- consequences of blood transfusion;
- radiation sickness;
- vitamin B12 deficiency, folate deficiency anemia.
The degree of shift is assessed using a special index, which is determined by the ratio of the total number of all young neutrophils (myelocytes, metamyelocytes, promyelocytes, band neutrophils) to mature segmented ones. The norms for healthy adults are in the range of 0.05-0.1.
Is it possible to normalize the number of lymphocytes?
Physiological changes in blood composition return to normal after the elimination of the infectious focus, signs of inflammation, withdrawal of medications, and removal of intoxication in case of poisoning.
Natural ginseng root
During the recovery period after an infectious disease, to support the immune system, you can take herbal remedies such as tinctures of ginseng, eleutherococcus, aloe, and honey. These are weak immunomodulatory agents. Vitamin-mineral complexes and a diet rich in proteins help normalize hematopoiesis.
If lymphopenia or lymphocytosis is associated with chronic diseases, then long-term treatment will be required, possibly blood transfusion. It is not recommended to independently choose medications that affect the immune system.
The effect of cytostatic and radiation therapy for malignant neoplasms is based on the destruction of atypical cells. But, unfortunately, blood cells also disappear at the same time. Modern treatment regimens provide for a minimal effect on hematopoiesis. Only a specialist doctor can control the prescription of medications.