Rheumatoid arthritis
(RA) is a systemic autoimmune inflammatory disease of the connective tissue of the joints. Pathological processes lead to the development of irreversible changes. One or more joints may be affected. As a rule, the small joints of the hands and feet are affected, as well as the knees, elbows, jaws, hips and joints of the cervical spine.
As the disease progresses, the joints lose their mobility and the patient’s quality of life decreases. What makes the situation worse is that the cause of the disease has not yet been established. It is not yet possible to stop the process. In total, up to 1% of the world's population is affected by rheumatoid arthritis, of which 3/4 are women. The average age of onset of the disease is 40 years. The disease manifests itself during periods of severe emotional stress, under the influence of unfavorable environmental conditions, after trauma, or infection. RA is characterized by early disability in 70% of cases. The main causes of death are infectious complications and renal failure.
tests
Causes of rheumatoid arthritis
Currently, there is no reliable data on the causes of the disease. There are several most likely versions supported by most of the medical community. The most popular of them is that RA is caused by several factors present in the patient’s medical history at the same time.
- Genetic predisposition to autoimmune disorders.
- Presence of MHC class II antigen (noted in most patients).
- Infectious agents: paramyxoviruses, hepatoviruses, retroviruses.
- The presence of antibody titers to the Epstein-Barr virus (found in 80% of patients).
Thus, the risk of developing rheumatoid arthritis is higher in women aged 35 - 40 years and older. Increases the chances of having close relatives with a similar diagnosis, as well as previous diseases such as measles, hepatitis B, lichen, herpes, mumps.
Any changes in the immune system, which begin an attack on one’s own connective tissue, can activate the pathological process. Among the triggering factors are frequent hypothermia, hyperinsolation (sunstroke), prolonged intoxication, viral and bacterial infections. May be affected by medications, disruption of the endocrine glands, long-term stress and depression.
Development of rheumatoid arthritis
When exposed to one or more factors in the body, an inadequate response of the immune system is triggered. Defender cells - lymphocytes stop diagnosing and destroying foreign microorganisms, their own healthy cells become their target. Substances are produced that cause erosive and destructive damage to the synovial membrane of the joints.
RA moves through the following stages:
- Synovitis. Cells of tissue origin (synoviocytes) begin to perform the function of macrophages, i.e., digest the remains of dead cells and foreign particles. As a result, pro-inflammatory cytokines are produced, causing activation of T-helper cells - cells that stimulate enhanced immune function.
- Osteoporosis. Reduced bone density is caused by activated macrophages and monocytes through the production of proinflammatory cytokines, including IL-1. This cytokine activates osteoclasts, which dissolve and destroy mineral compounds and collagen.
- The composition of blood and synovial fluid changes. The level of plasma cells producing immunoglobulins increases. The concentration of IgM and IgG to the altered Fc region of IgG increases (rheumatoid factors).
- Proliferative stage. At this time, pathological processes cause damage to cartilage tissue and bones. Capillaries of synovial tissue proliferate. Synoviocytes lead to the formation of pannus, an aggressive granulation tissue prone to tumor-like growth with invasion into cartilage and the articular part of the bone.
The last, proliferative stage is characterized by the formation of erosions. Without treatment, these processes can occur several months after the onset of the disease. Increased angiogenesis promotes the germination of blood vessels into cartilage and the penetration of bacteria deep into the cartilage tissue.
Classification
According to ICD-10, the disease is systematized into the following groups:
1. Seropositive RA:
- Felty's syndrome.
- RA with involvement of other organs and systems.
- Unspecified forms.
2. Youth RA.
3. Other RAs:
- Seronegative type.
- Still's disease.
- Rheumatoid bursitis.
- Rheumatoid nodule.
- Other specified and unspecified arthritis.
According to clinical manifestations, the disease is divided into the primary stage (less than 6 months have passed since the onset of the disease), early (from 6 months to a year), advanced (from 1 year) and late (more than 2 years). Rheumatoid arthritis is distinguished by the degree of loss of functionality, immunological factors, disease activity, and instrumental characteristics.
For doctors, immunological characteristics are of greatest importance. The presence of rheumatoid factor in the blood or the presence of anti-CCP (seropositive and seronegative RA). The results of tests that reveal these values allow you to correctly plan therapy.
Results of rheumatic factor analysis
Based on the results of the analysis, we can conclude that the rheumatic factor increases:
- slightly increased – from 15 to 50 IU/ml;
- elevated – 50-100 IU/ml;
- significantly increased – above 100 IU/ml.
By the amount of rheumatic factor, the severity of the autoimmune process can be determined.
The analysis is very important, since its result will show the presence and intensity of autoimmune processes and will allow you to quickly select the most effective treatment.
Symptoms
The initial stage of the disease has virtually no obvious symptoms. Over time, slight stiffness appears in the affected joints. As a rule, it occurs in the morning, as the secretion of glucocorticoids decreases. It is difficult for the patient to move, movements are inhibited. Sometimes you need help getting up. But after 30 minutes - an hour everything returns to normal. The clinic can be rolled out over several months or even years, gradually intensifying.
Primary symptoms also include:
- periodic joint pain;
- loss of appetite;
- increased fatigue.
Second stage
characterized by rapid cell division and thickening of the synovial membrane. There is symmetrical swelling of the joints, the skin in the affected areas has an increased temperature. Sudden pain is also observed, intensifying with active movement. To complete the process, they need the same amount of rest time that was spent moving.
Third stage
― active phase of inflammation involving cartilage and bones. The affected joints begin to deform, which leads to increased pain and loss of motor function.
Rheumatoid arthritis often has concomitant joint diseases, and vague symptoms make differential diagnosis difficult. Among the most beneficial combinations are rheumatism, osteoarthritis and other systemic pathologies of connective tissue. The only specific manifestation of rheumatoid arthritis can be called nodules, so-called subcutaneous formations on the extensor surface. They can be detected by palpation.
Extra-articular manifestations of RA
Pathological processes caused by rheumatoid arthritis that occur outside the joints occur in a third of patients. These symptoms also complicate diagnosis and influence the choice of treatment tactics. Among them:
- Cutaneous vasculitis (ulcerative-necrotic, livedoangiitis, infarction of the nail bed).
- Sjogren's syndrome (damage to the salivary and lacrimal glands).
- Eye lesions (scleritis - inflammation of the deep layer of the eye, episcleritis - inflammation of the connective tissue of the eye).
- Interstitial lung disease (inflammation of the alveoli, pulmonary capillaries and other tissues).
As a result of inflammation accompanying rheumatoid arthritis, pathologies of the cardiovascular, respiratory, and nervous systems may occur. The most serious complication is AA amyloidosis, which causes kidney failure.
Separately, it is worth highlighting various associated diseases that are not directly caused, but are associated with RA. These are coronary heart disease, thromboembolism, anemia, psychoneurological disorders, among which depression deserves attention. Like any other autoimmune disease with chronic inflammation, rheumatoid arthritis affects psychological well-being. The patient is recommended to undergo psychological courses and a comprehensive, comprehensive examination.
When a child needs a biochemical blood test:
* Yellowness of the skin and/or mucous membranes is a suspicion of hepatitis or stagnation of bile in the gallbladder.
* Colorless stools - possible hepatitis (sometimes occurs without jaundice) or a disease of the gastrointestinal tract (for example, pancreatitis).
* Vomiting and diarrhea - often associated with pancreatitis or viral hepatitis A.
* Strong thirst and hunger, rapid weight loss and fatigue, frequent urination - indicates diabetes.
* Poor appetite and weight gain . It is not necessary that the child is sick, but he needs a comprehensive examination.
* Nausea, abdominal pain, repeated indomitable vomiting and a pronounced odor of acetone from the mouth are signs of diabetic ketoacidosis (complications of diabetes mellitus - a life-threatening condition) or an acetonemic crisis in neuro-arthritic diathesis.
Read more about neuro-arthritic diathesis here
Diagnostics
First of all, the doctor studies the clinical criteria for rheumatoid arthritis. The disease should be suspected in patients with symmetrical polyarthritis. Damage to the wrist, II and III metacarpophalangeal joints is important. It is necessary to exclude hepatitis C. Pay attention to the presence or absence of changes in skin color in inflamed joints, the presence of deformities of the limbs, tenosynovitis of the flexors or extensors of the fingers. Diagnostics also includes laboratory and instrumental results.
Laboratory research
The tasks of the laboratory include blood tests for RF, anti-CCP, ESR, and CRP. The most progressive analysis is the titer of antibodies to ACCP, anti-CCP, anti-CCP.
- RF - analysis for antibodies to human gamma globulin is detected in 70% of RA patients. However, the indicator is not critical, since titers can be detected in other viral diseases and connective tissue pathologies. An RF test confirms rheumatoid arthritis in combination with a positive ACCP test.
- ACCP is a test with high sensitivity reaching 86%. In combination with the RF titer, it indicates RA. However, it is necessary to exclude hepatitis C, since ACCP and RF titer may occur with this viral infection.
Additional tests include a biochemical blood test to determine the activity of inflammation. A general blood test to detect anemia, an immunological test to determine the presence of rheumatoid factor (IgM antibodies).
Instrumental diagnostics
- X-ray examination. In the first months of the disease, radiography can only show soft tissue swelling. Marginal erosions, osteoporosis, and narrowing of the joint space are detected by the end of the first year of the disease or later.
- Magnetic resonance imaging. The most informative research method at the moment. It allows you to identify early signs of inflammation, detect erosions and lesions of the subchondral bone.
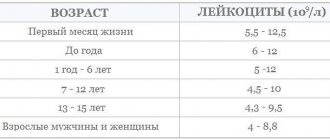
- Examination of synovial fluid. The procedure is carried out for exudative changes in the joints, to differentiate RA from arthritis of another nature. Cloudiness and yellowish color of the synovial fluid indicate the development of rheumatoid arthritis. The leukocyte count increases to 50,000/µl.
When making a diagnosis, it is important to exclude similar diseases: microcrystalline arthritis, sarcoidosis, reactive and psoriatic arthritis, systemic lupus erythematosus, osteoarthritis and other diseases.
Norms of blood parameters
There are generally accepted standards for rheumatic complex indicators that help confirm or refute the presence of pathology in the body.
Table “Acceptable values of rheumatic tests”
| Indicators and age group | Meaning |
| ASLO | |
| In adults | From 0 to 203 U/ml |
| In children (up to adolescence) | Up to 151 U/ml |
| Rheumatic factor | |
| In adults | Up to 15 IU/ml |
| In children (up to 12 years old) | Up to 13 IU/ml |
| C-reactive protein (regardless of age) | 0 (an indicator when the rheumatic test is positive, but not more than 5 IU/ml can also be considered a negative value) |
| Albumen | |
| In adults under 60 years of age After 60 years of age | 35–50 g/l 33–49 g/l |
| In children (up to 14 years old) | 37–54 g/l |
| Total protein | |
| In adults from 15 to 60 years | 65–85 g/l |
| In older people (after 60 years) | 63–84 g/l |
| The child is under one year of age | From 46 to 74 g/l |
| From one to 4 years | 60–76 g/l |
| 5-15 years | 58–77 g/l |
Values may vary slightly depending on laboratory, equipment and starting materials for analysis. Therefore, many research institutions indicate their limit norms for rheumatic test indicators on a special form.
Treatment
Therapy is aimed at containing the progression of the disease, reducing inflammation and preventing joint deformation and loss of functionality. The following medications are prescribed:
- Non-steroidal anti-inflammatory substances. They reduce pain to some extent and slow down the progression of RA. May include inhibitors and blockers for IL-1, IL-6, TNF-alpha. They do not block the development of erosion and disease, therefore they are used as aids.
- Glucocorticoids. Prescribed in combination with anti-inflammatory drugs. Allows you to control the development of severe monoarticular and oligoarticular symptoms. Not used on a regular basis, as they often cause unpleasant metabolic effects.
- Basic drugs. Essential medications that can significantly slow the progression of arthritis. Courses of treatment range from several weeks to several months. The drugs differ in chemical composition and pharmacology. They are combined with each other to select the optimal treatment with the greatest effect. According to statistics, ⅔ of patients who completed the course experience significant improvement, more than half of them achieve complete remission. However, you should be aware of the toxicity of these drugs. The doctor and patient must weigh all the risks and conduct regular monitoring of the patient’s condition.
Thus, the main treatment includes basic drugs, especially methotrexate, biological antagonist drugs, and immunomodulatory drugs. Other methods of auxiliary therapy include physiotherapeutic procedures, therapeutic exercises, and a balanced combination of physical activity and rest. Quitting alcohol and smoking can prolong the patient's life. Joint curvature can be corrected through surgical correction.
Forecast
Rheumatoid arthritis shortens a person's life expectancy for a number of reasons. The risk of heart disease doubles. This is caused by the presence of chronic inflammation. The situation can be aggravated by concomitant pathologies, for example, diabetes, obesity, alcoholism.
With the development of AA amyloidosis, despite treatment, the average life expectancy of the patient is about 10 years from the onset of the disease. Without therapy, the period is estimated at several years. A common cause of death is kidney failure. On average, RA shortens life by 3 to 7 years due to the high risk of infections and gastrointestinal bleeding.
Drug therapy is also not perfect. It can cause concomitant diseases and become one of the factors in the development of malignant neoplasms. Criteria for poor prognosis include:
- early (up to 4 months) x-ray changes in joints;
- persistent increase in erythrocyte sedimentation rate;
- constant involvement of new joints;
- carriage of HLA-DR4 antigens.
About 10% of patients are doomed to severe disability with loss of self-care skills. Rheumatoid arthritis is most severe in women, smokers, and Caucasians.
Advantages of the laboratories of JSC "SZTsDM"
At the laboratory terminals of the Northwestern Center for Evidence-Based Medicine, you can take tests to diagnose rheumatoid arthritis and other autoimmune diseases. Among the advantages of SZTsDM JSC:
- New modern equipment,
- Qualified and friendly staff,
- Quick availability of results and convenient ways to obtain them.
Laboratories are located in Pskov, Veliky Novgorod, Kaliningrad, St. Petersburg and other cities of the Leningrad region. You can take tests at any of them without being tied to residence or registration.
How to prepare and take tests
Blood is drawn from a vein in the morning on an empty stomach, 8-12 hours after the last meal. In emergency cases and in infants - without prior preparation.
Seven days before the test, do not introduce complementary foods to your baby, but feed as usual the day before. The day before the test, in an older child, avoid eating fatty foods and physical exercise.
Are norms constant indicators?
Yes. However, numbers and units of measurement in different laboratories may differ, depending on the equipment, reagents and methods used.