Epididymitis is an inflammatory process in the epididymis. This organ is directly involved in the formation of sperm. His disease, in the absence of adequate treatment, can lead to the most serious consequences, including infertility.
Most often, epididymitis affects men and adolescents aged 15-30 years, as well as older people over 60 years of age.
In addition, the reasons for the development of epididymitis can be:
- complications after infectious mumps (so-called mumps);
- hypothermia;
- constant difficulty urinating;
- complications of tuberculosis.
Indications
Surgical treatment is indicated in the following cases:
- Abscess of the epididymis or testicle.
- Accumulation of pus.
- Lack of results from antibiotic treatment.
- Acute form of the disease.
- Infertility due to obstruction of the appendage.
Contraindications
It is not recommended to perform surgery in case of exacerbation of chronic diseases and allergic reactions to medications and painkillers.
Prevention
There is no specific prevention of orchiepididymitis. As general preventive measures, we can recommend:
- Use barrier contraception during casual sexual intercourse.
- Practice a healthy lifestyle (rational nutrition, quitting smoking, abusing alcoholic beverages, playing sports, conditioning the body).
- Have a regular sex life.
- Avoiding sitting for long periods of time.
- Boosting immunity.
- Timely treatment of STIs ( prostatitis , urethritis ), infectious diseases.
- Avoid hypothermia.
- Avoid injury to the scrotal organs.
How does epididymitis manifest?
The most common symptoms of this disease are swelling, pain and swelling of the scrotum, as well as redness on the affected side.
Ultrasound of the scrotum
- Cost: 3,000 rub.
More details
Epididymitis also manifests itself:
- the appearance of bloody impurities in the semen;
- temperature rise to 38-39 degrees Celsius;
- discomfort and pain in the groin and lower abdomen;
- pain and burning during ejaculation or during urination;
- discharge from the opening of the urethra;
- increased pain in the scrotum during movement or defecation;
Symptoms
Acute orchiepididymitis on the right and acute orchiepididymitis on the left manifests itself with a high temperature (39-40°), a sharp pain syndrome radiating to the lower abdomen/lower back, aggravated by walking. Associated symptoms include weakness, general weakness, myalgia . On examination, there are signs of local inflammation - the scrotum on the side of the disease increases significantly in size, the folds are smoothed out, the skin of the scrotum becomes tense/shiny, and erythema is often present. When touched there is a sharp pain. Dysuria is typical ; patients complain of pain when urinating. In most cases, there is discharge from the urethra, often purulent and with an unpleasant odor.
In the absence of adequate and timely treatment, especially against the backdrop of weakened immunity, acute serous inflammation may transform into purulent epididymo-orchitis , which manifests itself as severe general intoxication with damage to the genitourinary system, and is also accompanied by the risk of developing a bilateral process.
With the transition to a chronic process, the severity of symptoms of orchiepididymitis decreases: a prodrome is characteristic, moderate pain in the scrotum, which intensifies with movement or palpation. The scrotum is compacted, and there is a discharge of impurities/red blood cells with an unpleasant odor in the semen. Patients complain of decreased libido .
Testicular anatomy
The testicle is a paired oval-shaped glandular organ that is responsible for the production of testosterone and sperm. The weight of the testicles rarely exceeds 30 grams. They are located inside the scrotum and are covered with white tissue, which visually divides the organ into 300 small parts. All parts have approximately 2-3 seminal canals. They contain Sertoli cells, which are responsible for the production of healthy sperm. Between the channels are Leydig cells, which stimulate the production of testosterone. In order for sperm to leave the testicles, it travels a long way through the efferent, convoluted, straight and accessory canals.
Consequences and complications
In the absence of adequate/timely therapy, the risk of impaired spermatogenesis and the development of difficulties in sperm transport increases. The risk of infertility increases significantly with bilateral orchiepididymitis, which is manifested by insufficient production of the male sex hormone ( testosterone ) and, as a consequence, androgenic insufficiency, manifested by decreased libido (sexual desire), insufficient erection, decreased performance, and decreased muscle mass.
Severity of acute epididymitis
The transition of the pathology to the acute stage is accompanied by pronounced symptoms. There are 3 stages in total: mild, moderate, severe:
- Mild – lasts up to 3 days. An ultrasound reveals an enhanced vascular pattern, and a blood test shows an increase in leukocytes to 12,000.
- Moderate – lasts up to 6 days and has severe symptoms, including an increase in body temperature to 39 degrees Celsius and pain. Ultrasound examination reveals inflammation and hypoechoic neoplasms up to 10 mm.
- Severe – lasts more than 7 days and is accompanied by severe symptoms. A blood test shows a leukocyte count of up to 25,000, which indicates a strong inflammatory process (body temperature rises to 40 degrees Celsius). The accumulation of pus is maximum, the epididymis is significantly enlarged.
Tests and diagnostics
The clinical diagnosis is made on the basis of anamnesis, the results of an objective examination of the scrotal organs and data from laboratory and instrumental examinations. Examination for orchiepididymitis includes:
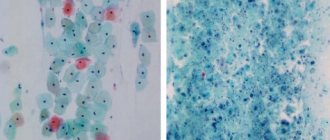
- Laboratory research methods: bacteriological examination of urine, biochemical blood test, CBC, OAM, urethral smear, bacteriological examination of sperm/prostate juice (with determination of sensitivity to antibiotics).
- PSA blood test.
- PCR (if necessary).
- Instrumental research methods: ultrasound of the scrotum, urethroscopy.
It is mandatory to examine not only the patient, but also his sexual partner.
Our doctors
Mukhin Vitaly Borisovich
Urologist, Head of the Department of Urology, Candidate of Medical Sciences
34 years of experience
Make an appointment
Kochetov Sergey Anatolievich
Urologist, Candidate of Medical Sciences, doctor of the highest category
34 years of experience
Make an appointment
Khromov Danil Vladimirovich
Urologist, Candidate of Medical Sciences, doctor of the highest category
35 years of experience
Make an appointment
Perepechay Dmitry Leonidovich
Urologist, Candidate of Medical Sciences, doctor of the highest category
40 years of experience
Make an appointment
Main classification
The classification of epididymitis according to the nature of the disease is divided into 2 types - acute and chronic stage. According to the degree of damage - one-sided (left or right) and two-sided (damage to two epididymis at once). Depending on the nature of the inflammatory reaction, there are:
- Specific form. The inflammatory process is caused by syphilis, tuberculosis or gonorrhea.
- Non-specific form. It occurs due to the action of bacteria, chlamydia, fungi, and viruses (influenza, herpes, etc.).
The infection enters the appendage in different ways: through the blood (hematogenous route), through the lymphatic vessels (lymphogenous), through the urethra (canalicular). There is also a secretory pathway, which is characteristic of specific infections. In this case, there are various causes of inflammation of the appendages. In addition to the infectious factor, there are others:
- Infectious-necrotic. Twisting of the appendage of the appendage leads to the occurrence of an inflammatory process, as well as the proliferation of pathogenic bacteria. Penetration of sperm into the epididymal tissue causes the development of granulomatous epididymitis. This pathology is characterized by a lack of response to antibacterial therapy.
- Stagnant. This factor is caused by various reasons: constipation, interrupted sexual intercourse, frequent masturbation, hemorrhoids, frequent erections without ejaculation.
- Traumatic. Appears due to injuries to the scrotum, after surgery or after the use of specialized medical instruments (catheters, use of an endoscope for cystoscopy, etc.).
Men should be wary of taking certain types of medications that can lead to the development of drug-induced epididymitis. Typically, this disease is caused by taking Amiodarone, a drug that is used to treat pathologies that cause irregular heart rhythms. Accordingly, the higher the dosage, the more the risk of damage to the appendages increases.
What is the treatment for epididymitis?
A urologist deals with the elimination of pathology. In the acute stage and rising temperature, hospitalization is carried out with strict maintenance of bed rest. Locally apply cold compresses to the scrotum and fix it in its normal position. The diet is normalized, spicy and sour foods are excluded. Next, physiotherapy, antibiotics and vitamins are taken. If pus has formed, then an opening and cleaning is performed. In extreme cases, the appendage is removed to prevent the spread of infection.
Therapy for this disease should be carried out under the close supervision of a urologist. The doctors at the CELT clinic have extensive practical experience and an impressive amount of knowledge, which means they will help you get rid of this pathology in the shortest possible time.
Modern medicine uses conservative and surgical methods to treat inflammation of the epididymis. Conservative methods are relevant in the absence of suppuration and high intoxication, when the symptoms are not so pronounced. Blockage of the seminiferous tubules, accumulation of pus, increased body temperature and acute pain during ejaculation are the main indications for surgery.
List of sources
- Akkaliev M.N. Acute orchiepididymitis: modern aspects of etiology, diagnosis and treatment. Literature review // Science and Healthcare. 2021. No. 2. P. 159-175.
- Inflammatory diseases of the genital organs in men. Guidelines. Ed. M.P. Kogan and G.G. Selezneva. Rostov-on-Don; 2011.
- Bashembaev Kh.M., Nazarkulov E.N. Choice of treatment method for patients with acute inflammatory diseases of the epididymis and testicle // Bulletin of the Almaty State Institute for Advanced Medical Studies. 2010. No. 2 (10). pp. 35-37.
- Naber K.G., B. Bergman B., Bishop M.K. Recommendations of the European Association of Urology for the treatment of urinary tract infections and infections of the reproductive system in men // Clinical microbiology and antimicrobial therapy. 2002. No. 4, Volume 4. P. 347-363.
- Vorchalov M.M. An integrated approach to the treatment of acute epididymo-orchitis: dissertation. ...cand. honey. Sci. Saint Petersburg. 2013. P. 140.
Conservative treatment of acute and chronic epididymitis
Therapeutic treatment is prescribed if:
- There are no accumulations of pus.
- There is no exacerbation of pathology.
- No hematomas formed.
- Tests reveal mild or moderate stage of epididymitis.
The duration of treatment is from 1 to 4 weeks, depending on the infection or virus that triggered the development of the disease. The specialist performs tests for reaction to antibiotics, after which he selects a drug based on the client’s individual characteristics. 2 antibiotics or antimicrobial drugs may be prescribed at once for synergy and better results.
Causes of inflammation
Inflammation of the appendages in men: the causes can be very diverse.
All causes of the disease are usually divided into 4 factors:
- The infectious factor is associated with the penetration of nonspecific (bacteria, viruses, fungi, mycoplasma or chlamydia) or specific (gonorrhea, syphilis and tuberculosis) infection into the epididymis through the blood, lymphatic vessels or through the urethra and seminal product. There is another way for infection to enter the epididymis - infection from distant areas due to sore throat, sinusitis and furunculosis.
- The infectious-necrotic factor is caused by torsion of the appendage of the epididymis, as well as as a result of sterilization (sperm cells penetrate into the tissue of the epididymis, causing inflammation).
- The stagnation factor is associated with impaired blood flow in the pelvic organs - blood stagnation, or as a result of excessive blood filling. The cause of “stagnation” can be interrupted sexual intercourse, masturbation with an erection, constipation, hemorrhoids, excessive sexual activity, as well as prolonged cycling.
- The traumatic factor is directly related to injury to the scrotal organs, after surgery, as well as after medical manipulations on the reproductive organs, such as catheterization, bougienage or cystoscopy.
Inflammation of the epididymis in men is associated with one of the factors:
- decreased immunity due to severe pathology - HIV, diabetes, hepatitis, oncology
- disruption of urine outflow is a favorable condition for the development of bacterial infection
- hypothermia
- overheating of the scrotal organs.
Surgical treatment of acute and chronic epididymitis
Lack of results with conservative treatment and severe stage of epididymitis are the main indications for surgical intervention. There are 5 types of operations:
- Orchiectomy is the complete removal of the testicle and epididymis in the most severe cases.
- Epididymectomy - removal of the inflamed appendage.
- Puncture from the scrotum - allows you to normalize the pressure in the scrotum and eliminate pain.
- Partial resection of the appendage – resection of an area with a large accumulation of pus.
- Incision - opening microabscesses and cleaning the appendage.
The choice of surgical treatment is made by the attending physician based on the medical history and data obtained during diagnosis.
General information
Orchiepididymitis (syn. epididymo-orchitis) is a combined inflammation of the testicle and epididymis of various etiologies. ICD-10 orchiepididymitis code: N45.9. It is one of the most common diseases of the scrotal organs, which can develop as an independent disease or appear against the background of another pathology. Recently, there has been a clear trend toward an increase in the incidence of scrotal organs of infectious and inflammatory origin (acute orchitis , epididymitis , testicular torsion , hydrocele , scrotal trauma). It has been established that nonspecific acute orchiepididymitis occurs in almost 80% of patients with testicular inflammation.
testosterone are produced in the testicles , and their maturation occurs in the epididymis. Triggers of the inflammatory process in the testicles/appendages are predominantly urethritis and prostatitis . According to various authors, the pathology is most common in men aged 20 to 40 years, there is pronounced seasonality, there is no endemicity, and no racial priorities have been identified. The disease develops primarily as a result of infection entering the testicle/epididymis through the hematogenous or lymphogenous route.
The problem is quite relevant since acute epididymitis orchiepididymitis on the right/left, being an urgent disease, requires quick diagnosis and adequate treatment. Delay/inadequate treatment of the acute process contributes to its transition to a chronic course, which can cause sclerotic/dystrophic changes in the testicle and its epididymis, causing obstruction of the vas deferens, which is accompanied by a high risk of impaired male reproductive function.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
| Ultrasound of the scrotum | 3 000 |
| Duplex scanning of scrotal vessels | 3 500 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Infertility after epididymitis
An inflamed epididymis cannot be responsible for the metabolism, maturation, accumulation and movement of germ cells, which occurs normally. It is in the epididymis that sperm accumulate for maturation, which becomes impossible when inflammation develops in them. As a result, problems with reproductive health and the inability to fertilize a woman occur. If the process is long, then connective tissue grows in the epididymis, which obstructs the lumen of the vas deferens and an obstructive form of infertility occurs when sperm cannot pass through the canals and fertilize the partner. In this case, you only have to resort to testicular puncture to obtain germ cells and carry out conception using in vitro fertilization.
Diagnosis of inflammation of the epididymis in men
At the initial appointment, the doctor asks the patient the necessary questions, collecting anamnesis. In particular, the doctor is interested in:
- nature of complaints;
- past infectious diseases;
- injuries and operations in the scrotum area;
- sexual activity;
- presence of bad habits;
- lifestyle and working conditions.
Then the urologist-andrologist conducts:
- examination, assessing the condition of the genital organs;
- digital rectal examination of the prostate gland.
Based on the results obtained, if acute or chronic inflammation of the epididymis is suspected, the following are prescribed:
- seeding of urethral discharge on the UPM;
- culture of prostate secretion on UPM;
- PCR for urogenital infections;
- microscopy of urethral discharge;
- clinical blood test;
- Ultrasound examination of the scrotal organs. Ultrasound, being a completely safe and highly informative method, allows you to carefully study the structure of the genital organs and identify pathological processes. The additional use of Doppler makes it possible to assess blood flow, which, in particular, helps to distinguish epididymitis from testicular torsion, which has similar symptoms;
Additionally, studies such as TRUS and microscopy of prostate secretions can be performed.
After recovery, a spermogram is prescribed. Analysis of the ejaculate allows us to identify a violation of the process of spermatogenesis, as well as the presence of leukocytes and pus in the seminal fluid.
Treatment of the disease
Therapy depends on the course of the disease. If it is acute, but there are no complications, then patients are treated on an outpatient basis. If there is a threat of complications, the patient is hospitalized. For drug treatment, drugs from the following groups are used:
- Antibiotics. The most commonly prescribed fluoroquinolones are effective if the disease is caused by E. coli or chlamydia.
- Non-steroidal anti-inflammatory drugs. They are used to relieve pain and relieve inflammation. Antispasmodics, analgesics and novocaine blockade are also used to eliminate pain.
- Antituberculosis drugs. Prescribed for the tuberculosis form of the disease (and only with timely detection). Treatment is quite long - can reach 1 year (with a suppressed immune system).
The treatment regimen is determined solely by the attending physician. The choice of drugs depends on the causative agent of the disease: sore throat, influenza, tuberculosis, sexually transmitted infections, etc.