Surgeon
Bohyan
Tigran Surenovich
Experience 36 years
Surgeon of the highest category, Doctor of Medical Sciences, member of the International Association of Surgeons, Gastroenterologists and Oncologists
Make an appointment
Hemangioma is a benign vascular formation that appears due to an embryonic disorder in the development of blood vessels. The tumor appears on any part of the skin and looks like a red, purple or bluish spot rising above the surface of the skin. Most often detected at birth or formed during the first weeks of life. Treatment is surgical and conservative.
General information about the disease
Hemangioma appears in children as a birthmark. This change is the result of a vascular malformation. The detection rate of hemangiomas in newborns reaches 3%. In 10% of cases, the problem is detected in the first year of a child’s life. Statistics confirm that this is the most common benign soft tissue tumor in pediatrics. The detection rate reaches 50% of cases. The problem is 3-5 times more common in girls. Hemangioma in adults manifests itself in exceptional cases with inadequate treatment in childhood.
A benign tumor progresses rapidly. It grows rapidly on the surface of the skin and in depth. As it grows, the defect can destroy surrounding tissues and lead to impaired vision, hearing, and breathing. When a hemangioma is injured, there is a risk of infection and the formation of ulcerative deformities on the surface.
The causes of hemangioma have not been fully studied. It has been established that the pathology is a consequence of changes in the formation of the vascular system at the embryonic stage. The following factors can influence this process:
- a pregnant woman taking certain medications;
- past viral diseases;
- unfavorable environmental conditions.
Since hemangioma on the skin is more often detected in girls, there is a connection between the tumor and hormonal regulation, but it is not the main factor.
Forecast
Possible consequences of the disease
Hemangiomas can cause necrosis (death) of tissue, so the lesion becomes an entry point for infection.
The addition of a purulent process can cause sepsis. With hemangioma of bones, their destruction is possible. In addition, the process can contribute to blood clotting disorders and the formation of blood clots. Malignancy is possible - degeneration of hemangioma into cancer. With timely consultation with a doctor, the neoplasm is successfully treated in 100% of cases Source: What a pediatrician needs to know about infant hemangiomas. Zakharova I.N., Kotlukova N.P., Roginsky V.V., Sokolov Yu.Yu., Zaitseva O.V., Maykova I.D., Idrisova G.R., Pshenichnikov I.I.: Medical Council , 2021.
The main types of the disease and its symptoms
Depending on the morphological characteristics, the following types of hemangiomas are distinguished:
- simple (capillary). It has clear boundaries, red or purple-blue color. It turns pale when pressed, and then restores the shade;
- cavernous (cavernous). Lumpy, nodular formation located subcutaneously. It is characterized by a soft elastic consistency, which is explained by the structure - inside there are cavities filled with blood;
- combined. It has a cutaneous and subcutaneous part. Clinical manifestations are characteristic of the capillary and cavernous type;
- mixed. A tumor with a complex structure, containing elements of vascular, nervous, connective and lymphoid tissues. Color, consistency and appearance vary depending on the fabrics included.
Tumors are single and multiple in nature, and can be small or large. In 95% of cases in pediatrics, simple forms are diagnosed. Symptoms of hemangioma appear only externally; rarely the patient complains of itching and discomfort in the affected area.
Treatment and examination of a child with hemangioma provides:
- pediatrician;
- surgeon;
- dermatologist.
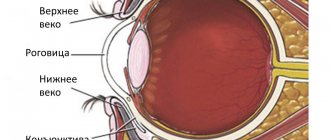
Additionally, consultation with an ophthalmologist, otolaryngologist, urologist, dentist and pediatric gynecologist is indicated. In order to determine the depth of spread and evaluate the structure, an ultrasound scan of the affected area is performed. The complex evaluates the speed of blood flow in the tumor itself and the vessels supplying it.
The prognosis for patients is favorable. The tumor may regress on its own. A soft tissue tumor that does not have indications for surgical removal does not need to be eliminated. The decision on the treatment scheme or dynamic control method is always made by the doctor.
Are you experiencing symptoms of hemangioma?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Are red moles dangerous?
In themselves, these formations are harmless and are not precancers.
If you have a lot of red moles on your body, the cause may be a serious liver or pancreas disease. Pay attention to this - this is a reason for examination.
Problems may arise in case of traumatization of hemangiomas. Even fairly small formations threaten heavy bleeding, which is not easy to stop.
Clinical case
Patient L, 26 years old, presented with a traumatized mass in the axillary region. According to her, she tore off a convex hemnagioma with the edge of a rigid corset of a wedding dress almost a few minutes before the start of the wedding ceremony. The hemangioma bled very heavily and a large blood stain appeared on her white dress. She had to wear the witness's jacket over her wedding dress. It was in such a strange outfit that the wedding took place.
Treatment information
Previously, when a hemangioma was detected in childhood, a wait-and-see approach was adopted; doctors hoped that the tumor would resolve on its own before reaching puberty. Over time, this statement became irrelevant due to the low frequency of reverse development. In only 5% of cases, hemangioma in children disappears from the skin without consequences, in 2% of cases this occurs before the age of 5.
Today, hemangioma is treated using the following methods:
- physical removal;
- surgical resection;
- drug therapy.
The list of popular methods of physical removal includes cryodestruction, laser irradiation, sclerotherapy and electrocoagulation. The described methods allow you to painlessly remove soft tissue tumors. Complete disappearance takes from several months to several years. Scars may remain on the skin.
The surgical method is rarely used in modern practice. It is used for small hemangiomas in adult patients. Most often, tumors located in invisible areas of the body are excised. The cosmetic effect is questionable; scars remain on the surface of the skin.
Drug therapy is based on the use of hormonal and antitumor drugs. It is often used at the preparatory stage to reduce the area of hemangioma. Complete resorption due to drug therapy occurs rarely, in no more than 2% of cases.
Our clinic specialists will help you choose an effective treatment method and get rid of hemangioma on the skin. Doctors will conduct an examination and determine the most effective treatment regimen, and establish a prognosis for the possibility of self-relief. Examination using new equipment is the key to successful therapy. The experience of doctors will allow you to choose the best scheme for eliminating hemangioma, allowing you not to fear possible consequences.
Why do hemangiomas appear?
The exact causes of hemangiomas have not yet been identified; It is generally accepted that their appearance can provoke disruption of intrauterine development of the fetus due to a viral illness of the mother or oxygen starvation. Additional risk factors for the formation of congenital hemangioma:
- multiple and/or late pregnancy;
- increased amount of estrogen in the mother;
- her sedentary lifestyle;
- unbalanced diet;
- alcohol or nicotine intoxication of the fetus;
- his low birth weight.
In adults, the cause of neoplasm can be a hereditary predisposition, diseases of the cardiovascular system, excessive ultraviolet radiation, and increased levels of the female hormones estrogen.
Answers to frequently asked questions
What does a hemangioma look like?
Externally, the tumor is a red or bluish spot that merges with the skin or rises above its surface. The size of the spot in diameter ranges from 1-2 cm to 10-20 cm. The tumor has different shapes. In children, temperature asymmetry appears; the defect is always warm to the touch.
Is it necessary to remove the hemangioma?
A skin hemangioma must be removed if it causes discomfort, itches or bleeds. It is necessary to remove the tumor if it is located in difficult places that are constantly rubbed by clothing.
Can a soft tissue tumor go away on its own?
It is not always necessary to remove hemangioma surgically. The tumor can regress on its own. There are several stages in the extinction process. It begins with the formation of a pale spot in the center of the tumor, then the shade changes and becomes normal towards the periphery. The process of disappearance is long, up to several years.
Why is hemangioma dangerous?
If treated incorrectly and untimely, complications may occur that pose a threat to human life and health:
- germination with subsequent destruction of nearby organs;
- destruction of bone and muscle tissue;
- spinal cord compression;
- ulceration of the tumor, infection;
- malignancy;
- development of pathologies of the vascular system;
- cosmetic defect.
How are hemangiomas treated?
The main method of treatment is surgical. In addition to cosmetic reasons, there are medical indications for this:
- rapid growth and threat of malignancy of the tumor;
- disruption of the normal functioning of organs - for example, if there is a tumor on the eyelid or tongue;
- impaired blood circulation – if the tumor is on a large vessel;
- infection and bleeding – for example, when on the genitals.
The priority is gentle, minimally invasive methods for removing hemangioma or vascular surgery methods to reduce blood flow in it. The excised tissue is sent for histological analysis.
If the neoplasm is small, it is possible to use electrocoagulation, radio wave or laser surgery, or cryodestruction with liquid nitrogen. For some forms of hemangiomas, sclerotherapy is effective - “gluing” damaged capillaries by injecting special solutions Source: Hemangiomas and vascular malformations. Modern theories and therapeutic tactics. Goncharova Y.A.: Child’s health, 2013.
For slow-growing tumors with a low risk of malignancy, conservative drug therapy with drugs from the group of beta-adrenergic receptor blockers is possible Source: Wong A., Hardy K., Kitajewsky A. Propranolol causes functional changes in hemangioma stem cells and hemangioma endothelial cells // Abstract book. ISSVA the 19th International Workshop on Vascular Anomalies. — 2012. – p. 245.. In some cases (if the tumor does not grow, does not bother, or there is a tendency towards its reverse development), they resort to wait-and-see tactics.
To ensure the effectiveness of treatment, after its completion, a control study is prescribed - ultrasound, tomography or dermatoscopy. To consult with a specialized specialist in St. Petersburg, fill out the online form.
Sources:
- What a pediatrician needs to know about infantile hemangiomas. Zakharova I.N., Kotlukova N.P., Roginsky V.V., Sokolov Yu.Yu., Zaitseva O.V., Maykova I.D., Idrisova G.R., Pshenichnikov I.I.: Medical Council , 2016
- Infantile hemangioma: classification, clinical picture and methods of correction. Sheptiy O.V., Kruglova L.S.: Russian Journal of Skin and Venereal Diseases, 2021.
- Hemangiomas and vascular malformations. Modern theories and therapeutic tactics. Goncharova Y.A.: Child’s health, 2013.
- Sires V. Systemic corticosteroid use in orbital lymphangioma /V. Sires, C. Goins, R. Anderson // Ophthal. Plast.Reconstr.Surg. — 2001. Mar. - Vol. 17(2). — P. 85 — 90.
- Wong A., Hardy K., Kitajewsky A. Propranolol causes functional changes in hemangioma stem cells and hemangioma endothelial cells // Abstract book. ISSVA the 19th International Workshop on Vascular Anomalies. — 2012. – p. 245.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Zolotov Sergey Alexandrovich
- Candidate of Medical Sciences, surgeon, specialist in laser surgery.
- From 2003 to 2009 completed training at the State Budgetary Educational Institution of Higher Professional Education "Russian National Research Medical University" named after. N.I.Pirogov Ministry of Health of Russia.
- From 2009 to 2011, he completed his residency at the Moscow State Budgetary Healthcare Institution, Research Institute of Emergency Pediatric Surgery and Traumatology, specializing in Pediatric Surgery.
- In 2011, he completed training under the program of additional professional education of doctors in laser medicine at the State Scientific Center for Laser Medicine of the Federal Medical and Biological Agency of Russia. From 2011 to 2014, he studied full-time graduate school at the Moscow State Budgetary Healthcare Institution Research Institute of Emergency Pediatric Surgery and Traumatology.
He has extensive experience in removing various benign formations of the skin and subcutaneous tissue using laser surgical methods.
More than 5 years of experience in surgery.
Price list for medical services of the laser surgery department
Consultation
| Name | Cost in rub. |
| Initial consultation | 2 000 |
Research
| Name | Cost in rub. |
| Cytological examination | 500 |
| Histological examination | 2 800 |
Anesthesia
| Name | Cost in rub. |
| Application anesthesia | 500 |
| Infiltration anesthesia | 500 |
| Conduction anesthesia | 1 500 |
Bandages
| Name | Cost in rub. |
| Adhesive bandage | 300 |
| Aseptic dressing | 500 |
| Bandage with medicines | 1 000 |
Removal of formations using laser radiation
| Anatomical zone | Cost in rub. for 1mm in maximum diameter |
| Scalp | 500 |
| Hands, forearms, feet, legs | 500 |
| Neck, chest, abdomen, back, armpits, shoulders, hips, crotch | 600 |
| Forehead, temporal region, ears, postauricular region | 600 |
| Eyebrows, nose, nasolabial triangle, chin, cheeks, cheekbones, red border of lips | 700 |
| Lower upper eyelids | 850 |
| Ciliary edge of the eyelids | 1 000 |
| External genitalia - single elements* *per 1 mm. 600 rub. | 1 000 |
Removal of papillomas with a diameter of up to 2.0 mm
| Name | Cost in rub. for a unit |
| Neck, chest, abdomen, back, armpits, shoulders, hips, crotch | 300 |
| Lower upper eyelids | 500 |
| Ciliary edge of the eyelids | 1 000 |
Scar treatment
| Name | Cost in rub. |
| Drug injection into the scar | 1 200 |
| Laser dermabrasion (resurfacing) per cm² | 1 200 |
Removal of vascular formations using laser radiation*
| Name | Cost in rub. |
| Photodestruction of the vessels of the wings of the nose | from 5 000 |
| Photodestruction of cheek vessels | from 10 000 |
*exact cost depends on capillary density, repeated stage of vessel destruction minus 30%
Treatment of ingrown toenails using laser radiation
| Name | Cost in rub. |
| Marginal resection of the nail plate | 6 000 |
| Removal of hypergranulations | 1 900 |
| Nail plate removal | 3 500 |
| Complex plastic surgery for ingrown toenails | 8 500 |
Removal of lipoma, atheroma
| Name | Cost in rub. |
| Lipoma removal | 18 000 |
| Removal of atheroma up to 5 mm | 6 000 |
| Removal of atheroma from 5 to 10 mm | 12 000 |
| Removal of atheroma more than 10 mm | 18 000 |