The first signs of the development of varicose veins are often attributed to ordinary fatigue, a trip to the doctor is ignored, and they continue to lead their usual lifestyle, aggravating the condition of the veins. Complications with varicose veins develop very quickly. Mostly those who require surgical intervention come to the specialist. Until this moment, everyone is trying to cure themselves with the help of tinctures and tablets.
How not to bring yourself to a deplorable state and take the necessary measures in time? First, you need to understand when you need to see a doctor. Secondly, go to the doctor as soon as you realize it’s time. This is not a case where you should wait a little and see what happens to the veins. Any delay can cost you dearly. The article contains descriptions of the signs of different types of varicose veins, which will help determine whether you suspect the disease.
Why do varicose veins appear?
If you know the causes of varicose veins, you can protect yourself in time by taking preventive measures.
Heredity. If one of your relatives suffers from varicose veins, then there is a chance that you will have it too. Varicose veins themselves are not inherited, but you may inherit structural features of the veins or, for example, a tendency to be overweight, which will affect the occurrence of problems with the veins.
Pregnancy. During pregnancy, a woman's body produces an increased amount of progesterone, which relaxes the walls of the veins. They can't do their job and the blood stagnates. Also during pregnancy, a woman’s body weight increases and the amount of circulating blood increases, which increases the load on the veins.
Overweight. Large body weight creates a constant load on the lower limbs. It is more difficult for the veins to supply blood to the heart and lungs, the blood stagnates, and the veins dilate. As a result, venous expansion of the veins occurs.
Wearing uncomfortable clothes and shoes. If the shoes are too narrow and tight, it prevents blood from circulating normally in the legs. The same goes for clothes that are too tight.
Elderly age. Age-related negative changes occur in the walls of blood vessels. They lose their elasticity, the vessels stretch and blood accumulates and stagnates in them.
Is it possible to cure varicose veins at home?
At home, it is allowed to use auxiliary methods for treating varicose veins, which alleviate symptoms. They use ointments from pharmacies or self-prepared ones, baths and lotions based on herbs, compresses, drink decoctions and infusions to improve blood flow and relieve swelling. Below are some recipes.
Chestnut tincture
Take about 200 g of ripened and peeled chestnuts. Pass through a meat grinder or grind with a blender. Fill everything with a liter of vodka, put it in a dark corner and leave for a couple of weeks. To make the product smell good, add a couple of drops of peppermint oil. In the evening, lubricate the legs with the tincture to get rid of heaviness and itching, strengthen blood vessels, and prevent their fragility. It is also recommended to make a compress from the tincture. If there is no chestnut, it is replaced with nutmeg, the recipe remains the same. Tincture with musk nuts can not only be used to rub sore feet; it is recommended to drink 20 drops a day. After the bottle is finished, a new tincture is made. But there should be a pause of 2 weeks between taking the next portion.
Calendula-based ointment
An infusion is made from calendula flowers - pour a tablespoon of boiling water, put on fire, cook for a couple of minutes, leave for 3 hours in a thermos. Strain the infusion and add it to some kind of fat; lanolin, Vaseline, badger fat are suitable. For the smell, it is recommended to add a drop of aromatic oil (rose, bergamot, citrus, sage, lavender, etc.) Rub the ointment in the morning and evening, with gentle movements from the bottom of the leg to the knee, until completely absorbed. Thyme, hop cones, and nettle are also added to the calendula infusion.
Chamomile oil
Medicinal chamomile flowers are placed in a half-liter glass jar of a dark shade so that the container is filled to the top. Pour in half a liter of any type of vegetable oil, for example, from olives, corn, hemp. Leave for a month, shaking or stirring from time to time. After this, the oil infusion is filtered. For scent, add a couple drops of tea tree, mint, lavender, and grapefruit aroma oil. Apply chamomile oil to the foot early in the morning and late in the evening, while simultaneously doing a light massage. You can also make night compresses from the infusion.
Compress based on wormwood
Take a package of kefir or fermented baked milk, 3 tablespoons of dried wormwood. The grass is crushed and mixed with kefir (ryazhenka). When the grass is wet, place it on cheesecloth along with a thick liquid. Then a compress is applied to the leg, covered with wax paper on top (cellophane film is not used), and everything is fixed with several layers of bandage. Keep your legs elevated and remove the compress after half an hour. It is recommended to do the procedure twice a day. Instead of wormwood, you can take hops, chamomile flowers, string, clover, oak or birch leaves, St. John's wort, horsetail, tricolor violet flowers, yarrow. Combinations of different plants give a good effect. To improve the effect of the compress after the procedure, it is recommended to lie down for a while with your legs raised up. All of the herbs listed can be infused and used to make a foot bath. The water in such a bath should be warm, the duration of the procedure is about 25 minutes. It relieves fatigue, swelling, reduces skin itching and pain.
Traditional recipes for internal use
Various herbal infusions improve blood flow in the veins well. The following herbs are used:
- Clover
- in succession
- Leaves and berries of lingonberries, viburnum, strawberries, raspberries
- Coltsfoot
- Calendula
- Japanese Sophora
- Melissa
- Schisandra
- Hawthorn
The grass is dried, then crushed and made into a mixture of different types of plants. Then take 3 tablespoons, pour a liter of boiling water, leave overnight in a thermos and drink 1/3 glass before meals.
Varicose veins are well treated with bee pollen and honey. Pollen should be consumed internally. Honey can also be eaten, but it still makes good compresses. It is recommended to add infusions of various herbs to honey.
How to understand that varicose veins are developing on the legs
Many people believe that the first signs of varicose veins are spider veins, swollen areas of veins and other external manifestations. But the pathology is very insidious and for a long time disguises itself as ordinary fatigue of the lower extremities, without revealing itself from the outside.
Get an online consultation
right now.
Get
Signs of the development of varicose veins that you need to pay attention to:
- Frequent muscle cramps. Since the blood does not circulate in the required mode through the veins, it stagnates and, as a result, oxygen starvation of the tissues. These factors lead to seizures.
- Unhealthy skin color on legs. Lymph and blood do not circulate well in the affected areas of the lower extremities. The skin color here becomes lighter with dark spots. As the disease progresses, these spots begin to become red, swollen, and itchy. If treatment is not started, the likelihood of trophic ulcers increases significantly.
- The legs and ankles begin to itch for no reason . In the vessels that are adjacent to the skin, transformations occur due to stagnation of blood and lymph. Metabolic products are not removed from these areas properly, which leads to itching, burning, peeling of the skin of the legs and its excessive dryness.
- Tingling, numbness of the limbs. At the initial stage of varicose veins, the feet may become numb for no reason. The patient will feel a tingling sensation. These symptoms arise due to poor functioning of the joints and tissue hypoxia. Normal motor activity is disrupted because the tissues lack interarticular fluid. If numbness becomes regular, then you should not postpone a visit to the doctor.
- Swelling . When the valve does not work at full strength, fluid accumulates in the intercellular space and swelling occurs. People prone to varicose veins are recommended to measure the volume of their legs in the morning and in the evening. A reason to sound the alarm and visit a phlebologist will be a change in indicators of 1 cm upward in the evening.
- Pain in the legs after a static position. If a person sat or just stood for a long time, and after that the lower limbs began to hurt and “hum,” then it is worth paying special attention to this factor.
At the final stages, dilated veins clearly appear on the skin of the lower extremities against a background of swelling and pain. During the period of decompensation in the last stages of varicose veins, signs of thrombophlebitis and trophic ulcers may appear.
Diagnostics
Diagnosis of varicose veins, the symptoms of which are described above, poses the following tasks:
- Determining the presence of pathology in each individual patient. It often happens that people who do not have varicose veins are confident in their presence, and vice versa. However, only an experienced phlebologist, based on an external examination and a series of comprehensive studies, can make an accurate diagnosis.
- Establishing the type characteristic of venous pathology. The doctor determines exactly which veins have undergone pathological damage, and also establishes the extent of this damage and possible or already occurring consequences.
- Prescribing the correct course of treatment. Based on the diagnosis and the characteristics of each specific organism, the attending physician makes a choice in favor of one or another treatment or a set of therapeutic measures.
- Assessment of the level of effectiveness of therapy, which is carried out by the attending physician during the elimination of the disease or after the patient’s complete recovery.
The main methods for diagnosing VV include:
- Plethysmography.
- Thermography.
- Magnetic resonance imaging.
- Ultrasound angioscanning.
- Computed tomography.
- Clinical studies: conversation with the patient, his external examination and manual examination.
- Radionuclide phlebography.
- Intravascular ultrasound.
- X-ray phlebography.
Most often, it is enough for a professional specialist to conduct a clinical examination and ultrasound angiography in order to diagnose varicose veins in the legs. At the Yuzhny clinic, you can undergo a full examination in order to make an accurate diagnosis by an experienced phlebologist. Our specialists work closely with clients, clearly explaining to each of them the specifics of the disease and possible ways to combat it.
Why is reticular varicose veins considered a mild form?
Varicose veins of the lower extremities have a separate type - reticular varicose veins. It is common mainly among women and is considered a mild form of varicose veins because in this case only the thin veins dilate.
Reticular varicose veins are often called cosmetic, since the main symptoms are external manifestations in the form of spider veins on the calves and thighs. Reticular varicose veins occur most often due to wearing high-heeled shoes, severe physical activity and taking hormonal pills.
Despite the fact that reticular varicose veins are mild, they need to be treated to avoid possible complications. Treatment of pathology of this type is carried out with the help of ointments, gels, venotonic nature, drug therapy, laser. Traditional surgical operations performed with a laser, especially a scalpel, are very rarely used.
What are the symptoms of pelvic varicose veins?
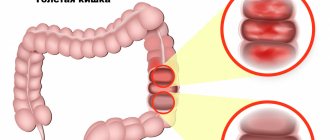
If venous blood stagnates in the pelvic area, this can lead to the appearance of varicose veins in this area. It can stagnate due to sedentary work, mechanical compression of the veins by the enlarged uterus, and uncontrolled use of hormonal drugs. The cause of the appearance of dilated veins in the pelvic area can also be poor nutrition, constipation, hernias, problems in the genitourinary area, pathologies in the pelvic organs, nervous disorders and insomnia.
Most often the disease occurs in women. Pregnant women and menopausal women are at risk. The pathology manifests itself as pain in the perineal area, which becomes more intense after hypothermia or a long stay in a sitting position. Also, venous tubercles form in the perineal area, the process of urination becomes painful, and unpleasant sensations are observed during and after sexual intercourse.
All these signs require immediate contact with a specialist, because without adequate therapy, varicose veins of the small pelvis are aggravated by complications: thrombosis, thrombophlebitis, trophic ulcers. Pathology is diagnosed mainly by ultrasound examination, if there are no external signs yet.
RISK FACTORS FOR VARICOSE DISEASE DEVELOPMENT
Heredity and its role in the development of varicose veins have not been unambiguously confirmed. One of the main counterarguments to the presence of a genetic predisposition is the different incidence of varicose veins in ethnic Africans and their fellow tribesmen who emigrated to the United States and Western European countries. At the same time, in comparison with settled fellow tribesmen, the incidence of varicose veins, which does not exceed 0.5%, among emigrants there is a significant increase in the incidence of 10-20%. In this regard, the obvious conclusion is that environmental factors, lifestyle characteristics and nutrition prevail in the pathogenesis of varicose veins.
Pregnancy is traditionally considered one of the main risk factors for the development of varicose veins, which explains, in particular, the more frequent (3-4 times) incidence in women. It is generally accepted that the main provoking factors are an increase in BCC (circulating blood volume) and compression of the pregnant uterus by the retroperitoneal veins. Meanwhile, the results of epidemiological studies indicate that only the second and subsequent pregnancies lead to a significant increase in the incidence of varicose veins by 20-30%. Moreover, the first signs of the disease appear already in the 1st trimester of pregnancy, when a sharp increase in the volume of blood volume or an enlargement of the pregnant uterus has not yet occurred.
Obesity is a proven risk factor for varicose veins. At the same time, an increase in body mass index to 27 kg/m2 and above leads to an increase in the incidence of the disease by 33%.
The high incidence of varicose veins in industrialized countries is to some extent due to dietary habits. A high degree of food processing and a decrease in raw vegetables and fruits in the diet has led to a constant deficiency of plant fibers necessary for the remodeling of the venous wall and chronic constipation, which causes a permanent increase in intra-abdominal pressure.
Lifestyle has a significant impact on the development and course of varicose veins. In particular, the adverse effects of prolonged static loads with heavy lifting or immobile standing and sitting have been proven. In Asian countries, the more frequent use of chairs and armchairs among the Europeanized part of the population led to a significant (3-4 times) increase in the incidence of varicose veins compared to people traditionally sitting on mats.
Dyshormonal conditions are involved in the pathogenesis of varicose veins. Their role has been progressively increasing in recent years, which is due to the widespread use of hormonal contraception, the popularization of hormone replacement therapy during the premenopausal period and in the treatment of osteoporosis. It has been proven that estrogens and progesterone, as well as their derivatives, reduce the tone of the venous wall due to the gradual destruction of collagen and elastic fibers.
How to determine the appearance of varicocele
Varicocele is a purely male type of varicose veins, which is an expansion of the veins of the spermatic cord. Signs of varicocele include nagging pain and a feeling of heaviness in the groin area, shrinkage of one of the testicles, enlarged veins under the skin, and frequent urination.
Why does pathology occur:
- the valves of the spermatic cord veins do not work well;
- there is not enough connective tissue forming the venous wall;
- the valves of the spermatic cord and testicles are underdeveloped;
- disruptions in the process of formation of the inferior genital vein in the womb.
If a man has high abdominal pressure, often experiences constipation, spends a lot of time sitting or standing, or exposes his body to excessive physical activity, then the risk of varicocele increases significantly. This disease has three degrees of severity: at first the veins can only be palpated in a standing position, at the second stage the lumps can be palpated while lying down, and at the third stage the swollen veins of the spermatic cord on the testicle are visible to the naked eye.
The stage when the testicles are covered with numerous clusters of veins is considered final and requires emergency treatment. After all, neglected varicocele very often becomes the cause of male infertility, thrombosis, thrombophlebitis and other complications. Pathology is diagnosed using an external examination, ultrasound, MRI or CT. Adult patients are often prescribed a spermogram to determine sperm activity and exclude asthenozoospermia.
What are internal varicose veins
With internal varicose veins, it is not the superficial, but the deep veins that are affected. The usual external signs in the form of bulging veins and vascular networks are often absent. The pathology is manifested by soreness of the lower extremities, which is often mistaken for banal fatigue. Elderly people are susceptible to internal varicose veins, whose deep veins transform due to age-related changes, become less flexible and elastic, and the valve system suffers from wear and tear. If the pathology is not treated, ulcers form on the lower extremities, which are difficult to heal.
Symptoms depending on the stage of the disease
Of course, it should be noted that the stage of development of the disease, the rate of progression, and existing complications (such as decompensation of venous outflow, thrombosis, varicothrombophlebitis, trophic ulcers), which are purely individual for each patient, are of great importance. Depending on the above, the optimal treatment option is selected.
The leading symptoms of varicose veins of the lower extremities are: swelling of the legs at the end of the working day, reticular veins - visually dilated saphenous veins, telangiectasias (in colloquial language - “spider veins”). For a long time, varicose veins manifest themselves only as a cosmetic defect - the presence of reticular veins, varicose veins (varix, lat. - node), however, it should be noted that the further development of varicose veins leads to the appearance of much more formidable symptoms and complications, such as pain, swelling of the feet and legs, and in advanced stages can lead to pigmentation of the skin of the legs (usually the internal surfaces), trophic ulcers, thrombosis, and varicothrombophlebitis.
Team of Doctors
Internal varicose veins are very difficult to recognize in the initial stages. Therefore, everyone who has a genetic predisposition to this disease is recommended to undergo a preventive ultrasound at least once a year. Since the deep veins are surrounded on all sides by muscles, it is impossible to detect their deformation during visual inspection
What does varicose veins of the foot look like?
At the very beginning of the development of pathology, one feels heaviness and fatigue in the legs by the end of the day. Next, aching pain may appear, a sensation as if the leg is bursting, and the foot swells. All these symptoms may go away on their own after rest. But you shouldn’t put off going to the doctor. If varicose veins of the feet are not treated at the initial stage, the disease will begin to progress. First, spider veins and spider veins will appear, then varicose veins will also affect large veins. At this stage, the pain becomes constant, the legs begin to swell more, and muscle spasms appear.
Prevention
Varicose veins on the legs, which are treated today using various methods, can be avoided by following preventive measures. Due to the fact that the risk of developing VV is much higher in women, it is they who need to not ignore the prevention of this disease. However, men should also not ignore preventive measures aimed at preventing the development of varicose veins in the legs. Key activities include:
- The use of local preparations (gels, ointments, creams) that help strengthen the walls of blood vessels, optimize the functioning of valves, reduce the risk of blood clots, eliminate swelling and heal wounds.
- The use of knee socks, tights, stockings and elastic bandages that have a compression effect. This is an excellent tool in the fight against varicose veins. These products can be purchased in specialized stores after consultation with a doctor, which is necessary due to the relative difficulty in independently determining the required type of compression garments.
- Specific exercises performed on a daily basis. They are able to stop even the dilation of blood vessels that has already begun. It should be borne in mind that if you have a tendency to BB, you will have to give up heavy physical activity, but in no case should you ignore an active lifestyle. For example, light jogging, swimming, yoga and skiing help maintain healthy leg veins.
- Preventive tablets for varicose veins are recognized as a more effective method of preventing VVs than the use of local drugs. However, any oral medication should be used only as directed and under the strict supervision of a competent specialist.
In order to prevent the situation from worsening, you should stop self-medicating at the first manifestations of the disease and consult a doctor. This will make it possible to make a correct diagnosis in a timely manner and prescribe adequate treatment, which will stop the progression of the disease and reduce to zero the risks of developing other pathologies.
Complications due to varicose veins
If treatment for varicose veins is not carried out or is carried out insufficiently, then sooner or later complications arise. These include venous thrombosis. A blood clot forms in the lumens of the vessel, which leads to thrombophlebitis. The vascular walls become inflamed, and the blood clot plays the role of a time bomb, because at any moment it can break off and clog vital arteries. Thrombophlebitis progresses especially quickly after infectious diseases, during air travel, difficult childbirth and complex surgical interventions.
Deep vein thrombosis of the lower extremities occurs very quickly. Literally within a few hours, inflammation occurs on the vein, the lower leg increases in size, swells, and acquires a bluish tint. At the slightest physical exertion, a person feels acute pain, but rest does not bring complete relief.
Trophic ulcers occur due to disruption of blood flow in tissues, resulting in necrosis and tissue rejection. First, severe swelling and burning of the skin appears. The legs become as if wet due to lymph seeping out; small ulcers first appear on the skin, which subsequently develop into large, non-healing wounds.
Very often, complications of varicose veins manifest themselves in the form of venous bleeding, which is sometimes impossible to stop without medical intervention. If a person with varicose veins has been injured in the area of bulging veins, lifted an unbearable weight, or overexerted in sports, then the likelihood that the thinned vein may burst increases.
Treatment methods for varicose veins of the lower extremities
There are various methods for treating varicose veins - surgical intervention, conservative methods (compression therapy, medication, physiotherapy) and modern non-surgical methods such as laser treatment, radiofrequency ablation of veins, sclerotherapy, phlebectomy.
1. Operation
Traditional surgery today is rarely prescribed and for certain indications. First of all, this is explained by the fact that the removal of a vein itself is accompanied by significant trauma, the possible appearance of hematomas, a long postoperative period and prolonged pain.
2. Conservative treatment
Depending on the stage and severity of the venous disease, one or another type of treatment is selected. Conservative treatment methods are required at any stage of the disease - as additional therapy or as primary therapy, depending on the degree of damage to the blood vessels. Conservative treatment methods include physical therapy, compression treatment of varicose veins and drug treatment of varicose veins of the lower extremities.
2.1. Physiotherapy
This method involves performing pressotherapy. This procedure is aimed at removing excess fluid from the lower extremities, formed against the background of chronic venous insufficiency and initial venous edema.
Like any other conservative method, physiotherapy does not imply the elimination of affected vessels and their areas; it reduces the manifestation of varicose veins. With the help of physiotherapy, venous and lymphatic outflows are improved, microcirculation is improved, and discomfort in the lower extremities, such as pain and cramps in the calf muscles, disappears.
2.2. Compression treatment of varicose veins
Compression therapy is used to apply pressure to the superficial and deep veins. The fastest outflow of blood occurs at the very bottom, in the legs - the veins are narrowed there, and the outflow of blood is the fastest. External pressure helps the blood flow and, as a result, the valves work more efficiently.
Compression treatment is used without fail as an additional therapy for all modern methods of treatment, less often - as the main method of treatment (in cases of the very initial stage of the disease and for its prevention).
Compression garments help relieve symptoms of varicose veins such as swelling, fatigue of the lower extremities, and a feeling of heaviness.
2.3 Drug treatment of varicose veins of the lower extremities.
Drug therapy involves taking medications that can improve the structure and function of the venous walls. However, the veins will remain tortuous and dilated; it is impossible to completely cure varicose veins with the help of medications, creams and ointments. Increased tone of the venous walls with the help of medications is not able to correct the improper functioning of the valves. Medicines (venotonics), ointments, creams reduce swelling and pain symptoms, and are also prescribed for the prevention of thrombosis and healing of trophic disorders.
With the help of conservative treatment, it is impossible to prevent the further development of venous disease and cure the patient.
3. Modern technologies and methods of treating varicose veins of the lower extremities
Today, medicine has made great strides forward; traditional operations remain far in the past; they have been replaced by modern methods of treating varicose veins without surgery. These include gentle methods such as radiofrequency ablation of veins, sclerotherapy, phlebectomy and laser treatment of varicose veins.
3.1 Radiofrequency ablation of veins (RFA of veins)
This is modern technology and one of the most effective ways to treat varicose veins of the lower extremities. RFA has great advantages over any other method of treating varicose veins. The procedure is a modern alternative to traditional surgery and is performed under local anesthesia. The essence of the method is to introduce a special conductor into the affected vein that produces thermal radiation. With the help of radiofrequency radiation, a thermal effect occurs on the walls of the affected area of the vein; the structure of the damaged vessel is destroyed, the vein is excluded from the general blood flow system. The operation lasts from 30 to 60 minutes and does not require hospitalization.
The procedure is absolutely safe for the patient and most effective. Important advantages of this method are the elimination of incisions (the operation involves a small puncture) and the fastest possible recovery after the procedure - after 15-20 minutes the patient can go home.
3.2
Sclerotherapy
This method involves the treatment of varicose veins of the lower extremities by gluing the walls of blood vessels, in other words, closing the vein. A drug in foam or liquid form is injected into the lumen of the vein, which glues the vein together. This method does not require any damage to the skin and is virtually painless. The procedure lasts about 30 minutes, and afterward compression therapy is required - compression garments or bandages help the process of gluing the veins.
With the help of sclerotherapy, both capillary networks and large veins are removed; This method eliminates postoperative scars and defects.
3.3 Phlebectomy
The method involves removing the altered vein. Phlebectomy is used in cases where the disease has gone beyond the initial stages, is severe, and other methods become ineffective.
The procedure is carried out through small incisions of a few millimeters and lasts about two hours; This implies hospitalization of the patient for 1-2 days. Further compression therapy is also required.
3.4 Laser treatment of varicose veins of the lower extremities (ELVE)
The endovasal laser coagulation (EVLC) method is one of the most common methods of treating varicose veins and involves the thermal effect of a laser beam on the vein walls. A light guide inserted into a vein acts on it with a laser beam, resulting in gluing of the venous vessel.
The procedure does not require general anesthesia and lasts about 40-60 minutes. Further compression therapy is mandatory.
The method of treating varicose veins is determined by the doctor, who first conducts all the necessary studies and, based on them, selects the most preferable method of treating the disease.