Keratitis
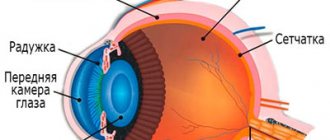
is an inflammation of the cornea, the transparent part of the outer layer of the eye. At its core, the cornea is a transparent lens in front of the pupil and is one of the refractive media of the eye. In addition, the cornea is extremely strong, which allows it to perform a protective function, and extremely sensitive - the slightest contact with the cornea of a foreign body causes a reflexive closure of the eyelids and increased lacrimation. This is how the body protects the cornea and eye from damage. And, as a rule, this protection works - keratitis is not the most common ophthalmological disease. Among inflammatory diseases of the eye, keratitis accounts for only 5%.
General information
The cornea is a relatively dense, transparent layer that protects the front, exposed surface of the eyeball. Both the shape of the cornea (it should be as flat, smooth, spherical as possible) and its transparency are of key importance, since any optical interference - turbidity, inhomogeneous inclusions, scars, etc. - distorts the normal refraction of light and/or reduces its intensity on the way to the retina inevitably affects the quality of the final visual image. Unlike some other inflammatory processes of the eye (blepharitis, conjunctivitis), which may not significantly affect visual acuity, with keratitis there is almost always a decrease in visual function. That is why it is extremely important to begin treatment as soon as possible, before irreversible scar changes form on the main optical axis of the eye.
Our services in ophthalmology:
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with an ophthalmologist (primary) | 3 900 |
| Appointment with a surgical doctor (repeated, for complex programs) within 3 months after the initial one | 2 000 |
| Ultrasound scanning of the anterior segment of the eye | 1 000 |
| Removal of foreign bodies of the cornea, conjunctiva | 2 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Types and types of keratitis
In publications you can often find a division of keratitis into exogenous (caused by external influences) and endogenous (caused by internal factors present in the body). However, such a classification seems too general and not entirely successful; It is unclear, for example, to which class allergic keratitis associated with wearing contact lenses should be classified: on the one hand, the allergic reaction is caused by internal immune disorders, on the other, by an external, artificial object.
According to the dynamics of development and type of course, acute and chronic keratitis are distinguished; as a variant of the second type, recurrent keratitis is sometimes considered separately.
The depth of spread of the inflammatory process is essential: superficial keratitis is much less dangerous than deep keratitis, in which the inner corneal layers are scarred.
According to the degree of severity, keratitis is usually divided into mild, moderate and severe; according to the localization of inflammation - central and peripheral.
However, the most convenient and intuitive is the etiological classification, where keratitis is grouped according to the direct causes of the inflammatory process.
Prevention methods
The prognosis of the disease largely depends on how quickly it was diagnosed and how carefully the patient follows the treatment recommendations received from the ophthalmologist. Early stages of keratitis are cured with good effect, the likelihood of relapse is minimal. Severe forms require constant medical supervision and surgical correction to maintain the ability to see.
It is much easier, as ophthalmologists note, not to treat an already formed pathology, but to avoid it. To do this, it is recommended to follow simple preventive measures to prevent the infection from activating or entering the body. Among them:
- avoiding situations in which there is a risk of eye injury;
- the use of special safety glasses if a person’s work involves repairs, construction, or welding;
- careful adherence to hygiene rules when using contact lenses, refusal to wear other people's lenses that may be infected with the herpes virus;
- compliance with precautions when working with substances that can leave a burn on the cornea;
- hardening of the body, which helps increase immunity, preventing the activation of the pathogen in the body;
- protecting yourself from overheating, hypothermia, infections and other unpleasant pathologies that can provoke an exacerbation of herpes.
There is also a vaccine that helps fight the infectious agent. It is recommended to introduce it in early autumn, before the onset of severe cold weather. It is the cold season that often causes exacerbations. Before vaccination, the patient is recommended to take a course of antiviral drugs.
Herpetic keratitis is a disease that develops slowly but steadily. If you ignore it for a long time, you can face significant inconvenience, and sometimes even lose your vision partially or completely. A timely visit to the doctor when the first suspicious symptoms appear will help protect against complications. The main thing is to follow the ophthalmologist’s treatment recommendations after the infection has been accurately diagnosed!
Causes of the disease
The main factors of corneal inflammation include:
- eye injuries, incl. chemical, physical, mechanical damage (foreign body, ultraviolet burn from the blinding light of an electric welding arc, intense solar radiation, etc.);
- infections (viral, bacterial, fungal);
- allergic reactions, incl. severe seasonal, drug, onchocerciasis allergies.
Actually, onchocerciasis keratitis, although it is more often classified as allergic, is essentially parasitic, since the allergenic toxin is produced by helminths from the filaria family. Similarly, the very common infectious-allergic keratitis when wearing contact lenses is most often caused not by the lenses as such, but by non-compliance with the rules of hygiene and care for them, as a result of which the cornea becomes infected.
More rare forms are neurogenic keratitis, keratitis due to hypo- or vitamin deficiency, as well as idiopathic keratitis (for example, the so-called filamentous), the causes of which have not yet been reliably established.
Symptoms and signs
Almost all types and types of keratitis are characterized by the so-called. corneal syndrome, including increased lacrimation, increased sensitivity to light and uncontrolled closure of the eyelids (blepharospasm). As a rule, redness is pronounced, the vascular network becomes noticeable, and in severe cases, neovascularization (vascular neoplasms) occurs. The pain can be quite intense. The corneal layer swells, the surface loses its smoothness and often ulcerates (sometimes with a tendency to peel off), and infiltrates appear. Cloudiness of the cornea becomes one of the main symptoms and complaints with keratitis, since the opacity or translucency of the cornea has an extremely negative effect on the acuity and clarity of vision.
Keratitis is often accompanied by concomitant symptoms, the severity of which varies from mild to moderate discomfort (dry nasal and oral mucosa, headache, difficulty swallowing) to severe complications from the periodontium, gastrointestinal tract, etc. Various types of keratitis are characterized by their own specific features.
Clinical picture
The clinical picture of keratitis is a series of manifestations specific to this disease, which have received a special name - corneal syndrome.
It includes symptoms:
- increased lacrimation;
- photophobia;
- narrowing of the palpebral fissure, it is impossible to open the eye completely;
- eye pain;
- sensation of a foreign object in the eye;
- redness of the eye.
In severe cases, the inflammatory process spreads to other parts of the eye and affects the sclera and iris. Another possible complication is ulceration at the site of inflammation. It can lead to perforation, in which infection enters the deep structures of the eye.
Viral keratitis
Keratitis caused by viruses is often accompanied by a blistering rash. The pathogenic agent can be almost any aggressive virus (measles, chickenpox, adenoviruses), but most often it is the herpes virus. As is known, over 95% of the population is infected with herpes infection, and in most cases, herpes occurs latently, in an asymptomatic form, and is activated only when immune resources are weakened, general exhaustion of the body and other unfavorable conditions. In this case, inflammation of the cornea is usually preceded by typical herpetic symptoms - rashes on the lips or other mucous membranes. With herpetic keratitis, as a rule, swelling and the appearance of fuzzy, vague infiltrates predominate.
Diagnostics
Diagnosis of herpetic keratitis begins with examination. The presence of characteristic blisters suggests a lesion caused by herpes. Since the disease can be sluggish, without characteristic manifestations, the diagnosis is clarified using laboratory and instrumental studies. To detect the pathogen, scrapings are taken from the affected tissues or tear fluid.
Laboratory diagnosis of ophthalmoherpes includes:
- Study of scrapings from the conjunctiva using fluorescent antibodies.
- Linked immunosorbent assay.
- Blood or tear fluid test for antiherpetic antibodies.
- Polymerase chain reaction (PCR) of biological fluids that detects the virus.
Instrumental examination helps to assess the extent and depth of anatomical changes. Instrumental diagnostics include anterior optical coherence tomography, biomicroscopy and fluorescein test.
A fluorescein test is performed to identify ulcers or films on the cornea and assess the area and extent of the lesion. After applying the solution to the eye, the ophthalmologist examines the tissue using a slit lamp with a blue filter.
Bacterial keratitis
Keratitis can be caused by a variety of pathogenic microorganisms, primarily cocci (Staphylococcus aureus, Streptococcus, Gonococcus) and Pseudomonas aeruginosa. A rare and very dangerous infection, even resulting in blindness, is acanthamoeba infection (named after the causative agent Acanthamoeba), which can exist, in particular, in the gap between the contact lens and the surface of the cornea. With the development of the so-called creeping corneal ulcers caused by gonococcal, tuberculosis, syphilitic and other bacterial infections, the risk of rapid and irreversible loss of vision is also very high.
Treatment of the disease
Almost all special sources emphasize the dangers of self-diagnosis and self-medication. The fact is that it is almost impossible for a non-specialist to distinguish incipient keratitis from “ordinary” conjunctivitis, and the bacterial form, for example, from a fungal one. Meanwhile, therapy in each case should be aimed at eliminating the primary pathogenic factor.
Thus, viral infections require stimulation of the immune response with interferon preparations (or medications that promote its production in the body) or antiviral agents. These include: Oftalmoferon, Poludan, Acyclovir, etc.
For bacterial infections, treatment with antibiotics is necessary, and their choice, dosage, and duration of treatment should correspond as closely as possible to the type and sensitivity of the pathogen. Typically, ophthalmologists prescribe medications in the form of Vitabact, Levomycetin, Tsipromed eye drops or ointments (Tetracycline, Floxal, Tobrex, Erythromycin eye ointment).
Fungal infections of the cornea usually require much longer treatment compared to other forms, and include specific antimycotic drugs based on fluconazole, natamycin, amphotericin, etc.
The main method of relieving allergic reactions are drugs that suppress the secretion of histamine and reduce the reactivity of H1 receptors. The most well-known and widely used antiallergic drug since the mid-90s remains loratadine (and numerous generic medications based on it). Basic antiallergic drops: Opatanol, Lecrolin, Allergodil.
As additional therapy aimed at relieving general inflammatory symptoms, vasoconstrictors, moisturizers, hormonal and non-steroidal anti-inflammatory drugs can be prescribed. Physiotherapeutic methods (laser irradiation of the cornea, electrophoresis of drugs) are actively used.
However, the main factors of therapeutic success in the treatment of keratitis, which allow preserving vision and preventing chronification of the process, the development of severe complications, and involvement of the deep layers of the cornea, are:
- timely seeking help, refusal to attempt self-medication;
- reliable differential diagnosis in order to establish the causes of inflammation, the type of pathogen, the severity and localization of the process;
- adequate etiopathogenetic therapy aimed at eliminating the pathogenic factor.
By contacting our ophthalmology center, you are guaranteed to receive high-quality diagnostics and effective treatment of diseases by recognized specialists using high-tech equipment! Remember: keratitis is a serious disease that can lead to the most severe consequences, including permanent loss of vision.
Surgical interventions
Conservative therapy is the basis for the treatment of herpes keratitis, but it is not always effective. In some cases, the disease, despite the medications used, continues to progress, and vision rapidly deteriorates. Then surgery is recommended. Two methods are used.
Scraping
The technique is the simplest and most common. Using a special device, the doctor carefully cleans off the epithelium affected by the disease. Cleaned areas are treated with an antiseptic solution. Then their healing is observed.
Keratoplasty
A complex operation that is a last resort. It is performed if conservative therapy with scraping does not have the desired effect. During the operation, the affected area of the cornea is removed, and the donor part of the organ is carefully sutured in its place.
Before keratoplasty, the patient must undergo examinations, as before a full-fledged surgical operation. The manipulation is performed only after the exacerbation of herpes keratitis has passed. During the period of exacerbation, intervention is not done, since donor tissue may be damaged and rejected.
| A quick solution to the problem is a last resort. |
It is used if the patient has advanced his disease, and there is no hope of correcting the situation using conservative methods.