General blood test - where do they come from?
From a finger or from a vein. Previously, the practice of collecting capillary blood (that is, from a finger) was widespread. Today, this technique is being replaced by assessment of the composition of the venous fluid. In large laboratories, only the second method is used. And there is an explanation for this.
It is difficult to assess the real picture from a drop of the main physiological fluid. It is simply not enough to assess, for example, hemoglobin. Therefore, if you want to get an accurate result rather than an approximate one, go to a laboratory where the blood is taken from a vein.
pixabay.com/
How is blood taken and is preparation needed for the procedure?
Donating blood is a simple and virtually painless procedure that even infants can easily tolerate. Biological material for general examination is taken mainly from a finger, but to check against an extended list of parameters and in some other cases, doctors prescribe venous puncture.
To prevent infection and take clean material, the nurse wipes the pad of one of the fingers of the left hand with a swab soaked in alcohol. Immediately after this, a tiny incision about 3 mm deep is made with a special instrument, a scarifier. The blood protruding from the incision is collected with a collection pipette and poured into a tall tube. A small portion of the liquid is smeared onto a glass slide.
If a doctor prescribes a venous puncture, a rubber tourniquet is placed on the patient's forearm to slow down the blood flow below the dressing. Then the puncture site on the inner surface of the elbow is disinfected with alcohol, after which a hollow needle is inserted into the vein. Through it, blood from the vessel fills a special test tube, and a small amount of biomaterial is applied to a glass slide.
No special preparations are required for the procedure. The only thing doctors can ask is not to have breakfast before collecting biomaterial, since eating food can distort the results obtained.
In some cases, the analysis has to be done several times over a set time period, including to track the effectiveness of the prescribed treatment. To obtain the most accurate data for comparison, repeat blood donation is carried out approximately in the same period of time as the first time.
General blood test - what is included
The analysis can be brief and detailed. The first evaluates three criteria.
Hemoglobin. A pigment responsible for transporting oxygen to organs and tissues. Decreased levels can be observed with anemia, bleeding, kidney damage, and oncology. Elevated levels indicate thickening of the blood, disturbances in the functioning of the heart, and dehydration of the body.
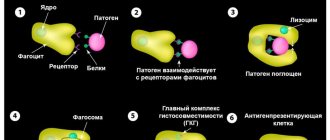
Leukocytes. These are white cells, a change in the number of which indicates an infectious or inflammatory process. There are five types of leukocytes working in our body, and all of them protect the body from negative external factors and aggressions. Thus, lymphocytes “jump” during inflammation, eosinophils during an allergic reaction, monocytes during autoimmune diseases and tumors. Based on the “leukocyte formula” picture, a doctor can diagnose a whole range of diseases.
ESR. Erythrocyte sedimentation rate indicator. If it is high, it means that there is inflammation or infection in the body. In women, ESR increases on the eve of critical days, in the first trimester of pregnancy. A low level indicates a previous illness.
Merely assessing these factors is enough to diagnose inflammation, the presence of infection and the tendency to clots.
pixabay.com/
Times change
Changes are visible already at the stage of blood sampling: if previously the doctor collected blood in several test tubes with reagents, a glass capillary and made a smear on the glass, now very small volumes are used - from 12 to 150 μl [15] of blood is enough to examine it for all parameters.
Let's take a look into a modern hematology laboratory. Wow! Everything is cluttered with equipment, and the laboratory assistant is nowhere to be seen... Maybe he went off to make himself some coffee? He won't make it in time! The blood test will be ready in a minute, and the device will give the result in the form of a paper tape with numbers and abbreviations, behind which all sorts of parameters are hidden.
Modern hemoanalyzers are divided into several classes, depending on what they can do. Each subsequent class is a new stage of evolution - faster, more accurate, more perfect. The use of a combination of technologies works wonders: if the first analyzers could determine eight blood parameters and did not distinguish between types of leukocytes [16], then the latest devices are able to differentiate up to seven populations of leukocytes [17] and in total examine more than 40 blood characteristics.
As Arthur C. Clarke said, “Any sufficiently advanced technology is indistinguishable from magic.” Indeed, the most detailed results in such a short period of time cannot but surprise. But all magic is based on physical laws. And although names like electrical impedance, light scattering and photometry are a little intimidating at first glance, now we will understand what principles underlie each analysis technology.
Population census
In the middle of the last century, Wallace Coulter made a revolution by patenting the technology of automatic cell counting. One of the leaders in the production of hematology analyzers, the Beckman Coulter company, is named after him [18]. The aperture-impedance method (or Coulter method) is based on the registration and analysis of impulses that occur when a cell passes through an aperture from one container to another, each of which contains an electrode. When there is no cell in the hole, current flows freely through the electrolyte between the electrodes under the influence of an electric field. To direct the cells to the aperture, a pump is used that pumps out liquid from one container, and the formed elements rush into it. Passing through the aperture, the cell displaces a volume of electrolyte equal to its volume from one container to another. In this case, a pulsed change in resistance (impedance) occurs - the cell membrane creates an obstacle to the free flow of current. At the same time, the current strength recorded by the meter also changes. The number of generated impulses corresponds to the number of formed elements, and the height of the impulse is proportional to the volume of the cell [19]. Using information about the number and volume of formed elements, the device can calculate hematocrit, the average concentration of hemoglobin in an erythrocyte, the width of the distribution of cells by volume and many other parameters [15].
Divide and rule
Differentiation of leukocytes into populations can be carried out using a Coulter counter, but a problem arises - different types of leukocytes are similar in volume and similar pulse amplitude does not always allow one to accurately determine the cell type. What should I do? To solve this problem, combinations of reagents are selected that change the size of cells to varying degrees so that it becomes possible to separate them [15].
But the most common method of differentiation is flow cytometry [20]. The method works as follows: cells in the flow are alternately irradiated with a laser, and the resulting light scattering and fluorescence signals are recorded by detectors and analyzed. In order to correctly determine membership in a population, several parameters are examined at once. Thus, light scattering at a small angle provides information about the relative size of cells, and light scattering at a right angle allows you to “look” inside the cell and study its internal structure - the presence of granules and the shape of the nucleus. Another parameter - fluorescence - can tell about the number of antigens and their appearance on the surface of cells - this cannot be accurately determined by eye. Unlike manual differentiation methods, not 100–200 cells are analyzed, but tens of thousands per second! And each leukocyte receives an individual approach: hydrodynamic focusing ensures that the cells line up in a row and are irradiated one by one in the flow cell. The result of the count appears on the screen in the form of scatter diagrams, where cells with similar properties form clusters.
Precipitated: 2.0
Modern instruments can measure ESR in two fundamentally different ways. The first is the modified Westergren method. The principle of operation has not changed since your grandmother's time, but due to automation it has become faster and more accurate. The second is measuring the kinetics of erythrocyte aggregation using an optical method [21]. It happens like this: an anticoagulant is added to the blood, the tubes with blood are placed in a rotor, where automatic mixing occurs. After this, the analyzer takes part of the blood into a microcapillary, where it accelerates and abruptly stops (the so-called “stopped stream” method). The stop causes aggregation of red blood cells, and at this moment the optical density of the blood is determined using a photometer - the denser the red blood cells are located, the less light will pass through the sample. The device uses the data obtained and builds a sedimentation curve - its analysis will allow you to present the result in the usual units of ESR measurement [22], [23].
Photo for memory
To determine hemoglobin concentration, the International Committee for Standardization in Hematology recommends the methemoglobin-cyanide method. However, a different test that does not use toxic cyanide is now widely used. Meet the SLS method. It is named after the main reagent - sodium laurithyl sulfate. SLS destroys red blood cell membranes, after which it binds to heme groups and forms stable complex compounds. They are analyzed photometrically - laser light is passed through the blood sample. Complex compounds absorb part of the light, as a result of which the intensity of the output light flux weakens. Attenuation is measured using a photosensor and the resulting data is converted into hemoglobin concentration units [24].
What does a complete blood count show?
The detailed analysis considers:
- level of erythrocytes - red blood cells;
- color index (MCHC) - a sign of saturation with hemoglobin and red blood cells;
- reticulocytes - germ cells of red blood cells;
- platelets - cells responsible for the ability of blood to clot;
- thrombocrit - the ratio of total blood volume to the number of platelets;
- Plasma cells are agents of the immune system that produce antibodies.
The disease is indicated by strong deviations in indicators. For example, an increase in red blood cell levels may indicate heart or lung disease. A change in color indicator is a sign of anemia and vitamin deficiency. The reticulocyte count may change in anemia, tumor metastasis, and autoimmune diseases.
An increase in platelet levels is possible after surgery, with intense physical activity, and tumors. A decrease indicates anemia, an autoimmune process, and inflammation.
Competition "bio/mol/text"-2019
This work was published in the category “Visually about the beloved” of the “bio/mol/text” competition-2019.
The general sponsor of the competition and partner of the Skoltech nomination is the Skoltech Center for Life Sciences.
Competition sponsor: the largest supplier of equipment, reagents and consumables for biological research and production.
The audience award was sponsored by BioVitrum.
"Book" sponsor of the competition - "Alpina Non-Fiction"
How to read results
In commercial laboratories, the result is given on a form where standards are indicated along with the indicators. This is convenient for perception, since shifts in one direction or another are immediately visible. Moreover, the standards are indicated separately for men, women and children. And this is important to consider, especially in childhood.
pixabay.com/
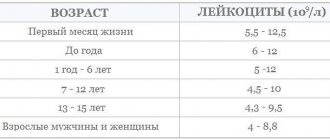
As you grow older, the composition of your blood changes. And the standards that are relevant for a month-old baby are no longer suitable for a one-year-old baby. Therefore, age limits have been introduced for children:
- up to a year;
- from one to six years;
- from seven to 12 years;
- from 13 to 15 years.
And only then the indicators approach those of adults, for men and women. But even the deciphered results do not use such a clear gradation. Therefore, only a doctor should read the analysis and interpret it. After all, when studying on your own, there is a high risk of making a mistake and diagnosing diseases that you or your child do not have.
In addition, a general analysis is a primary diagnosis. And it is usually not enough to make a diagnosis. Your doctor may order other types of tests. And based on the data obtained, establish the cause of the disease and recommend treatment. So studying the “blood picture” by the patient is, as a rule, pointless. These numbers on paper only have meaning in context. And only a doctor can examine it.
Rules for collecting capillary blood
Tool
The finger is pierced with a disposable sterile scarifier - this eliminates the risk of infection. The size of the needle or blade is selected individually, depending on the age and physical (physiological) characteristics of the patient. Modern automatic scarifiers reduce both pain and anxiety for the patient.
| Acti-lance automatic lancets | Scarifiers are designed specifically to prevent severe trauma to the phalanges of the fingers of patients. Uniform needle pressure reduces pain to a minimum. |
| Prolance automatic lancets | Scarifiers with a double spring mechanism provide high puncture speed and eliminate needle vibration. 6 different color-coded sizes allow you to choose the lancet for your desired blood flow. |
| Impromini tubes with plastic cap without capillary | Hermetically screwed plastic cap. They have a protrusion tray for easy blood collection. The design of the lid reduces the aerosol effect. |
| Impromini tubes with plastic cap and capillary | The built-in capillary allows you to quickly and accurately draw blood into the tube. Hermetically screw cap. The second hinged lid ensures the safety of the sample during transportation after removing the capillary. |
Choosing a blood collection site
Choose a non-cooled, non-cyanotic, non-edematous finger. The puncture is best done at the tip of the fourth finger of the left hand (for right-handed people). Fingers II and III can be pierced. If the patient’s hands are cold, then before performing the puncture they need to be wrapped in a fairly hot towel for 10-15 minutes. To increase blood flow, gently massage the finger from base to tip. Using a swab moistened with alcohol, carefully treat the tip of the finger and allow the surface to dry.
In newborns and children under 1 year old, capillary blood is collected from the heel. The method of taking blood from the heel is in many ways similar to the method of taking blood from the finger. A deep heel injection is performed at the distal edge of the heel bone, after preheating the foot in warm water
The procedure for taking capillary blood from a finger
- Prepare the necessary equipment on the manipulation table.
- Identify the patient, introduce yourself, announce the progress and purpose of the procedure. Make sure that the patient has informed consent for the upcoming procedure. If this is not the case, check with your doctor for further steps.
- Label the tubes, indicating the patient’s name and department (in order to eliminate errors in identifying the biomaterial sample).
- Treat hands hygienically and dry.
- Treat your hands with antiseptic. Do not dry, wait until the antiseptic has completely dried
- Wear non-sterile gloves