Complexes with this research
Preventive check-up Universal annual preventive screening 11,960 ₽
Composition Coagulogram Study of the functional state of hemostasis 2,020 ₽ Composition
Examination during pregnancy. 1st trimester 16,690 ₽ Composition
IN OTHER COMPLEXES
- Expanded hospital complex RUB 7,700
- For those at risk of COVID-19 RUB 4,510
- Female infertility RUB 16,210
- Joining IVF RUB 23,020
- Men's check-up No. 1 RUB 18,570
Why do you need to know the INR?
INR analysis is a common research method during the diagnosis of cardiovascular diseases. In addition, bleeding and severe thrombus formation are direct indications for studying all parameters affecting coagulation.
Knowing the INR is very important for the cardiologist who prescribed anticoagulants to the patient, since this allows him to control the correctness of the dose calculation, in order not to harm the patient. This also includes taking warfarin, the dosage of which is determined for each patient individually.
In case of cirrhosis of the liver or other disease of the filtering organ, it is also important to know the INR level, because it is the liver that produces many factors that clot the blood.
A separate group of patients are pregnant women. First of all, this is due to the fact that the entire body system begins to work differently during pregnancy. The level of hormones and enzymes changes, and the volume of blood circulating through a woman’s veins increases. Hence the need to control the functioning of the hematopoietic system. Due to the high level of blood clot formation, the likelihood of complications is high. And if the blood is too thin and there is a lack of platelets, there is a high probability of dangerous bleeding during childbirth.
At the very beginning of labor, each woman in labor is given a catheter in a vein, into which, if necessary, an IV will be placed with a composition that increases the level of blood clotting to prevent large blood losses.
Detailed description of the study
Normal blood clotting is possible by maintaining a balance between the processes of blood clot formation and mechanisms that prevent excessive blood clotting.
Prothrombin is a protein that is produced in the liver and plays an important role in blood clotting. Under its action, blood clots form in case of damage to the vascular wall, and bleeding stops.
Prothrombin time (PTT) is the time in seconds it takes for a blood clot, or thrombus, to form.
Prothrombin index (PTI) is a value equal to the ratio of the PTI of the control sample to the PTI of the test sample, expressed as a percentage. The indicator is also used in conjunction with other tests included in the coagulogram to assess the risk of thrombosis or bleeding.
INR (international normalized ratio) is a calculated value characterizing the ratio of prothrombin time and prothrombin index. This indicator is used to monitor treatment with indirect anticoagulants. These drugs reduce the body's ability to form blood clots by blocking the formation of clotting factors. Patients taking anticoagulants should regularly monitor this indicator to prevent complications of anticoagulant therapy. The frequency of INR testing is determined by the attending physician.
Cardiovascular diseases, liver pathology, diabetes mellitus and some other conditions contribute to an imbalance between the blood coagulation and anticoagulation systems. During pregnancy, there is also some change in PTT, PTI and INR. It is caused by changes in hormonal regulation and related factors and usually refers to physiological conditions.
An increase in PTT may be associated with bleeding, and its reduction increases the risk of thrombosis. To prevent complications associated with thrombosis, drugs are prescribed that reduce the likelihood of vascular clot formation - anticoagulants. At the same time, these medications, if the dose is incorrectly selected, increase the risk of bleeding, which requires specialist supervision.
The results of the analysis reflect the value of all three indicators. Assessment of PTT, PTI and INR will help the doctor assess the state of the blood coagulation system and select treatment.
INR norm
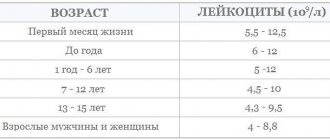
Units are used to express INR. The higher the INR, the less blood contains prothrombin and other factors that affect coagulation. The INR of a healthy person ranges from 0.85 units. up to 1.37 units. At the same time, the patient’s age affects the values of the norms:
- Newborns and children of the first year of life – from 0.9 units. up to 1.25 units
- Children from one to six years old can normally have 0.95-1.1 units.
- In patients aged 12-16 years, the normal INR ranges from one to 1.35 units.
- After 16 years, the value should be within 0.85 units. – 1.3 units.
For those who have already been prescribed anticoagulant therapy, the INR should be between 2.0 units. up to 3.0 units, because drugs that fight the formation of blood clots do not allow the blood to thicken, which also affects the prothrombin index.
If a patient is not taking blood thinning medications, but his INR is higher than normal, this may indicate:
- liver diseases;
- coagulopathies;
- prothrombin deficiency;
- lack of fibrogen;
- vitamin K deficiency;
- taking certain medications that affect blood composition;
A low INR always indicates that a person is at risk. Value below 0.5 units. reports the onset of venous thrombosis.
Who do doctors prescribe “indirect” anticoagulants (warfarin)?
Patients who need treatment and prevention of thrombosis and embolism of blood vessels, including: – heart rhythm disturbances (atrial fibrillation); – heart valve diseases;
– presence of prosthetic heart valves or blood vessels, incl. in combination with aspirin (acetylsalicylic acid); – acute venous thrombosis (phlebothrombosis) and pulmonary embolism (in combination with heparin); – recurrent venous thrombosis; – repeated pulmonary embolism; – thrombosis of peripheral, coronary and cerebral arteries; – postoperative thrombosis; – myocardial infarction, complicated by the development of an aneurysm and intracardiac thrombus; – during surgical or thrombolytic treatment of thrombosis; – when performing electrical cardioversion of atrial fibrillation (as an additional therapy); – congenital diseases accompanied by pathological thrombosis (thrombophilia).
Indications for prescribing INR
A blood test for INR is prescribed for certain indications. The normal range of this test varies depending on the underlying disease of the patient.
Indications:
- Preoperative examination of patients. The norm is closer to 1 (from 0.7 to 1.3, usually 0.85-1.25).
- Taking blood thinners (such as Warfarin). The norm is 2.0-3.0.
- Therapy for pulmonary embolism. The norm is 2.0-3.0.
- Condition after aortic valve replacement with a mechanical implant. The norm is 2.0-3.0.
- Condition after mitral valve replacement with a mechanical implant. The norm is 2.5-3.5.
- Preventive treatment of pulmonary embolism for heart defects. The norm is 2.0-3.0.
- Preventive treatment of deep vein thrombosis after surgery. The norm is 2.0-3.0.
INR analysis for patients taking blood thinners is carried out at certain intervals, which are determined individually by the doctor. At the beginning of the disease, when the patient is in the hospital, such tests are performed daily. Next, the patient is recommended to monitor the INR once a week and, if the test results are stable, then the frequency of tests can be reduced to once every 2-3 weeks.
The following changes in the patient’s life or symptoms of hypocoagulation may be the reason for prescribing an extraordinary test:
- long-term cold or other illness;
- changing the concomitant therapy regimen;
- lifestyle or diet changes;
- sudden climate change;
- unmotivated nosebleeds;
- bleeding gums;
- causeless appearance of hematomas;
- blood in urine:
- prolonged and heavy menstruation in women;
- streaks of blood in sputum or vomit;
- blood in stool (or tarry stool);
- prolonged bleeding from cuts;
- unexplained lumps, pain and swelling in the joints while taking a blood thinner.
Decreased INR level
There is also the opposite condition - hypercoagulation, in which the blood thickens. This condition is dangerous due to blood clots that can block blood vessels leading to vital organs.
- INR blood test - what is it. Norm and interpretation of INR blood test in adults and children
Then such severe conditions as pulmonary embolism (thromboembolism), myocardial, kidney, spleen, intestinal infarction, acute ischemic cerebrovascular accident occur.
Typically, INR levels decrease when:
- dehydration of the body (rapid loss of fluid without its replenishment) - when taking diuretics, burns, impaired permeability of the walls of blood vessels, when fluid leaks out of them into the surrounding tissues, and cellular elements remain in the channel;
- hereditary deficiency of antithrombin III;
- when taking hormonal drugs (especially oral contraceptives);
- infectious diseases accompanied by a significant increase in temperature;
- malignant neoplasms;
Also, indicators may be low due to technical errors during blood sampling or analysis.
Warfarin: use, rules of administration, selection of dosages.
The content of the article:
- General information about taking warfarin.
- Contraindications.
- INR control. Target INR range.
- INR value for patients with prosthetic heart valves.
- About a missed dose or temporary discontinuation of the drug.
- Selection of warfarin dosages and rules for changing the dose of drugs.
- Diet while taking warfarin.
- Precautionary measures.
- Interaction of warfarin with other drugs.
- Portable devices for self-monitoring of INR at home.
General information about taking warfarin.
Warfarin is a drug (anticoagulant) that reduces blood clotting. It is prescribed when there is a high risk of unwanted blood clots. The most common indications for prescribing warfarin: artificial heart valve, atrial fibrillation, deep vein thrombosis, pulmonary embolism, sometimes after a heart attack, stroke, for thrombophilia (a disease in which blood clotting is increased and blood clots constantly appear).
Warfarin blocks part of vitamin K, from which the liver synthesizes prothrombin, a substance necessary for the formation of blood clots. Vitamin K enters the body with food from green vegetables, and is also produced by human intestinal bacteria. Warfarin “neutralizes” part of vitamin K, and the liver does not receive enough “building material” to create prothrombin. However, warfarin does not dissolve already formed blood clots.
The main condition for taking the drug is that warfarin should be taken every day, without skipping. To take the drug, it is important to determine the time when taking the medicine will be most convenient for you. It is advisable to do this always at the same time and on an empty stomach (food affects the absorption of warfarin, so it is better not to combine them). It is best to take warfarin once a day in the evening.
The length of time you take warfarin depends on the reason you are prescribed warfarin. For example, after installation of an artificial mechanical heart valve or for thrombophilia, taking the drug is indicated for life. After certain other heart surgeries or deep vein thrombosis, warfarin is usually prescribed for 6-12 months.
It is very important to control blood clotting when taking warfarin. The main indicator is the international normalized ratio (INR). The higher the INR value, the thinner the blood. Conversely, the lower the INR value, the thicker the blood. When adjusting the dosage of warfarin, it is important to balance the risk of thrombosis with the risk of bleeding.
Contraindications.
Before taking medications, you need to take into account the contraindications that are indicated in the instructions for the drug:
- manifestation of high sensitivity to the components of the product or suspicion of hypersensitivity;
- acute bleeding;
- severe liver and kidney diseases;
- the first trimester of pregnancy and the last 4 weeks of gestation;
- acute DIC syndrome;
- thrombocytopenia;
- lack of proteins C and S;
- varicose veins of the digestive tract;
- arterial aneurysm;
- increased risk of bleeding, including hemorrhagic disorders;
- stomach and duodenal ulcers;
- severe wounds, including post-operative wounds;
- lumbar puncture;
- bacterial endocarditis;
- hypertension is malignant;
- intracranial hemorrhage;
- hemorrhagic stroke.
Monitoring INR when taking warfarin.
At the stage of selecting the dose of warfarin, INR should be monitored every 3 days, after reaching the target range - once every 5-7 days, after receiving three consecutive results of a blood test for coagulation in the target range, you can switch to measurement once every 2 weeks. In general, it is necessary to measure the INR at least once a month throughout the duration of taking the drug. The best results of treatment with warfarin are achieved by monitoring the blood test for INR once a week. It is also necessary to carry out an INR analysis in case of changing the dose of warfarin, changing diet, taking other medications and other situations that could affect blood clotting. Remember that the INR may not change until 3-7 days after such changes occur.
The normal blood INR of a healthy person not taking Warfarin is about 1 (0.8–1.2). With a decrease in coagulability, the INR increases. The goal of prescribing warfarin is to reduce blood clotting to a level where the risk of thrombosis is significantly reduced, but the risk of bleeding is not yet too high.
For different conditions, this balance point is between certain INR numbers; Thus, when performing a blood test for INR, normal is a relative concept. For example, when installing a mechanical prosthetic heart valve, it is recommended to increase the INR to 2.5-3.5, and for atrial fibrillation to 2.0-3.0. These numbers are called the target INR range, which varies from patient to patient and depends on what specific disease is causing you to be prescribed Warfarin.
INR value for patients with prosthetic heart valves.
Table 1. Recommended INR value for mechanical heart valves*
| Heart valve position | Risk factors for TE complications | |
| none | present | |
| Aortic | 2,0-3,0 | 2,5-3,5 |
| Mitral | 2,5-3,5 | 3,0-4,0 |
Table 2. Recommended INR value for biological heart valves*
| Heart valve position | Risk factors for TE complications | |
| none | present | |
| Aortic | 2,0-2,5 | 2,5-3,0 |
| Mitral | 2,5-3,0 | 3,0-3,5 |
| Tricuspid | 2,5-3,0 | 3,0-3,5 |
Risk factors for TE complications (thromboembolic) include:
- atrial fibrillation;
- history of thrombosis, thromboembolism;
- left ventricular dysfunction (LVD)
- hypercoagulable state. Hypercoagulation - increased blood clotting, predisposing to the formation of blood clots, occurs with malignant neoplasms, blood diseases, and taking oral contraceptives.
About a missed dose or temporary discontinuation of the drug (when switching to a direct anticoagulant).
If you forget to take a warfarin tablet at the usual time, take the missed dose as soon as you remember. However, if it is already time for your next dose, skip the forgotten dose and continue taking the drug according to your regular schedule. Do not take a double dose to make up for a missed dose. Use a warfarin diary. Write down the missed dose in your diary and tell your doctor at your next visit.
If you forget to take warfarin for two or more days, call your doctor immediately!
There are situations when the attending physician recommends that you reduce the daily dose of warfarin or discontinue it for a short time and switch to a direct anticoagulant - heparin. This can include any medical procedure that carries a high risk of bleeding, such as dental, gynecological, urological procedures or minor surgery and cardiac catheterization. In these cases, 1-2 days before invasive interventions, the daily dose of warfarin should be reduced under the control of the INR (reduction of the INR to a level of 2.0). For abdominal surgical interventions, it is necessary to discontinue warfarin and switch to heparin therapy. Heparin therapy is started when the INR decreases to less than 2.0.
The duration of the break in taking warfarin is determined by the specific clinical situation: in the absence of signs of postoperative bleeding (6–12 hours), warfarin should be re-prescribed and heparin should be discontinued when the INR reaches 2.0 or more.
Selection of warfarin dosages and rules for changing the dose of the drug (using the example of 2.5 mg tablets).
Changing the dosage of warfarin (using the example of 2.5 mg tablets).
With a slight increase in INR, for example, with the aortic valve to 4.0 (should be 2.0-3.0) or mitral to 5.0 (should be 2.5-3.5), it is necessary to reduce the daily dose of warfarin by ¼ of that dose which you accept.
If the INR value increases and the aortic valve is about 4.0-4.5 or the mitral valve is about 5.0-5.5, it is necessary to reduce the daily dose of warfarin by ½ of the dose you are taking.
At high INR values (more than 5.0-6.0), skip warfarin for one or more days; after reaching the proper INR value, resume taking warfarin from half the dose at which the previously high INR value was recorded.
The “One Quarter” rule can be used when selecting the dose of warfarin, when changing concomitant therapy, or when overusing foods with a high content of vitamin K.
Warfarin is a drug characterized by individual differences in drug response due to a number of factors.
Factors influencing the effectiveness of warfarin
Diet while taking warfarin
Warfarin acts on blood clotting through vitamin K, which is found in varying amounts in foods (such as green leafy vegetables and herbs).
While taking warfarin you should not:
- allow significant changes in diet (for example, depending on the season);
- change your usual diet without prior approval from your doctor;
- enter into an intensive weight loss program;
- add new vitamins or dietary supplements to your diet without prior approval from your doctor. If you need to take vitamins, it is better to choose multivitamin preparations without vitamin K in the composition.
If you significantly increase your intake of foods rich in vitamin K while on a stable dose of warfarin, this can greatly weaken its effect and lead to blood clots!
Daily requirement of vitamin K: 0.03-1.5 mcg/kg/day (up to 105 mcg/day).
The maximum amount of vitamin K (3000-6000 mcg/kg) is found in dark green leafy vegetables and herbs (spinach, parsley, green cabbage), and in green tea up to 7000 mcg/kg. Intermediate amounts (1000-2000 mcg/kg) - in plants with paler leaves (white cabbage and Brussels sprouts, broccoli, lettuce). Vitamin K is found in legumes and mayonnaise (due to vegetable oils). Fats and oils contain varying amounts of vitamin K (300-1000 mcg/kg), more of it in soybean, rapeseed, and olive oils. The vitamin K content in dairy, meat, bakery products, mushrooms, fruits and many vegetables, black tea, and coffee is low (no more than 100 mcg/kg). Taking multivitamins that contain vitamin K may reduce the effect of warfarin. Regular consumption of berries and cranberry juice may increase the effect of warfarin.
Table. Vitamin K content in foods (µg/100 g)
| Products | Vitamin K content |
| Green tea, leaves | 964 |
| Black tea, leaves | 42 |
| Chard, leaves raw | 830 |
| Cabbage leaf | 817 |
| White cabbage | 125 |
| Spinach, leaves raw | 415-640 |
| Spinach, leaves, frozen, cooked | 360 |
| Brussels sprouts, fresh, frozen | 289 |
| Raw chicory | 231 |
| Red leaf salad | 210 |
| Soybean oil | 193 |
| Olive oil | 60 |
| Sunflower oil | 6 |
| Broccoli, fresh/frozen, cooked | 101-205 |
| Green onions | 190 |
| Peas | 81 |
| Iceberg lettuce, leaf lettuce | 123-173 |
| Kiwi | 41 |
| Beef liver | 93 |
| Butter | 30 |
| Cheese | 35 |
| Egg | 11 |
| Milk | 1 |
| Coffee | 38 |
Warfarin and food There is no need to avoid foods high in vitamin K. You should eat a nutritious diet. Continue to eat what you have always eaten - without making any sudden major changes to your usual diet. It is best to try to adhere to the principles of healthy eating (click on the blue link to learn more about healthy eating). Tell your doctor if you have digestive problems for more than 1 day (nausea, vomiting, bowel movements). Any disease accompanied by diarrhea can lead to vitamin K deficiency and increase the blood-thinning effect.
Some medicinal herbs can both enhance the effect of warfarin, for example: ginkgo biloba, garlic, angelica, papaya, sage, and reduce its effect, for example: ginseng, St. John's wort. In this case, the increased effect of warfarin when taken simultaneously with St. John's wort can persist for two weeks after discontinuation. Monitoring of MHO in these cases must be careful, because its value may increase even more when St. John's wort is discontinued.
Quinine contained in tonic drinks can enhance the effect of warfarin. You should be aware that warfarin can enhance the effect of drugs prescribed for diabetes, which can cause dizziness and weakness. In such cases, you should eat a piece of sugar.
Precautions during treatment with warfarin.
Both deficiency and excess of warfarin are dangerous to life and health. Strictly observe the intervals of control blood tests. Follow your doctor's instructions. With an overdose of warfarin , pinpoint hemorrhages and bruises on the body, bleeding gums, black stools, dark (red) urine, and changes in the menstrual cycle in women are possible.
In cases where the INR increases to 5.0, it is necessary to reduce the daily dose of warfarin or skip 1-2 doses of warfarin if the INR value is from 5.0 to 9.0. However, if you are in doubt about what to do if the INR value increases, then it is better to consult a doctor!
Treatment with warfarin limits the body's natural ability to stop bleeding. For this reason, you should be especially careful with activities that may cause cuts, bleeding, or other injuries. Any head injury can lead to very serious consequences.
Remember!
Independent withdrawal of warfarin is unacceptable, since there is a high probability of thrombotic (thrombosis of a prosthetic heart valve) and thromboembolic (stroke, heart attack, pulmonary embolism) complications!
Discuss any problems that arise with your doctor.
Interaction of warfarin with other drugs
Some antibiotics and cardiac drugs enhance the effect of warfarin, in particular amiodarone (cordarone), acetylsalicylic acid (aspirin) and others. Its effect is reduced by phenobarbital (part of Corvalol), carbamazepine, cytostatics, antacids, diuretics, vitamin C. More details in the table. Drugs that affect the effectiveness of warfarin
| Increase efficiency | Reduce efficiency |
| Antibiotics: | Sedatives and anticonvulsants: |
| penicillin | barbiturates (phenobarbital) |
| 2nd-3rd generation cephalosporins: | carbamazepine |
| monolactams | Cytostatics: |
| erythromycin | azathioprine |
| tetracycline | cyclosporine |
| metronidazole | Gastroenterological drugs: |
| Cardiac drugs: | sucralfate |
| amiodarone | antacids |
| propafenone | Cardiac glycosides: |
| quinidine | digoxin |
| disopyramide | |
| Non-steroidal anti-inflammatory drugs: | |
| acetisalicylic acid | Diuretics: |
| paracetamol | veroshpiron |
| Anabolic steroid | furosemide, torasemide |
| H2 blockers and proton pump inhibitors | |
| Ranitidine | |
| Omeprazole | |
| Vitamins A, E | Vitamin C |
| Simvastatin | |
| Allopurinol | |
| Isoniazid | |
| Amitriptyline | |
| Thyroid hormones |
- All drugs that you will take together with warfarin must be agreed with your doctor!
- Always disclose that you are taking warfarin when new medications are prescribed to you!
Portable devices for self-monitoring of INR at home.
Currently, there are portable devices for self-determination of INR (similar to systems for monitoring blood sugar levels in patients with diabetes), which can help you keep anticoagulation therapy under control. Among them, CoaguChek® XS has proven itself for patient self-testing and immediate receipt of PTT/INR results. CoaguChek XS provides accurate and reliable results in less than a minute using only 8 µL (one drop of blood). Your doctor will decide what dose of warfarin, test regimen, and monitoring method is best for you.
A portable INR self-monitoring device takes measurements automatically. Built-in internal quality control does not require instrument calibration or use of control solutions. To carry out the analysis, just one drop of blood from a finger applied to the test strip is required, and within a minute the result automatically appears on the device screen.
Benefits of INR self-monitoring
- Improving the effectiveness of INR control through regular monitoring.
- Improved treatment safety through more frequent testing.
- Increasing time within the target range and thereby ensuring higher long-term survival.
- Simplifying the choice of the most effective option for the prevention of thromboembolic complications.
- Increased reliability with immediate, accurate results.
- More independence with the ability to monitor your INR values anywhere, anytime.
- Improved quality of life by reducing the need for medical consultations and travel costs.
Compared with conventional methods, self-testing and self-monitoring can significantly reduce the risk of complications and death. Patients who self-test have a 39% reduction in risk of death and a 90% reduction in risk of complications compared with patients using conventional laboratory monitoring methods. Self-monitoring can reduce the risk of death even further - by 63% compared to conventional methods.
Staying within the therapeutic range longer is the key to treatment success.
Diet while taking warfarin. Vitamin K content
Warfarin is absorbed in the stomach and jejunum, so changes in the intestinal microflora that produce vitamin K may affect the effect of the drug. The activity of warfarin can also be affected by the food the patient eats. The diet when taking warfarin should take into account those foods that contain large amounts of vitamin K, which can weaken the effect of warfarin, and the lack of vitamin K in the diet can enhance the effect of the drug. Therefore, if you are prescribed warfarin, try to eat a balanced diet and try not to change your diet dramatically so as not to change the amount of vitamin K you get from food.
| Vitamin K content in foods (µg/100 g) | |
| Beef liver | 93 |
| Cheese | 35 |
| Butter | 30 |
| Egg | 11 |
| Soybean oil | 193 |
| Broccoli | 175 |
| Cabbage | 125 |
| Salad | 129 |
| Watercress | 200 |
| Head lettuce | 120 |
| Spinach | 415 |
| Cauliflower | 80 |
| Green tomatoes | 80 |
| Beans | 45 |
| Cucumbers, zucchini | 30 |
| Potato | 16 |
| Green tea | 712 |
| Note: daily requirement of vitamin K is 0.03-1.5 mcg/kg/day (up to 105 mcg/day) | |
Warfarin and alcohol
Alcohol is not recommended during warfarin treatment.
You can indulge in a glass of wine once or twice a week. Exceeding this norm may lead to increased effects of the drug and, as a result, possible bleeding. Illnesses that affect appetite and digestion (vomiting, diarrhea) can also reduce or increase the effect of warfarin, so tell your doctor about any changes in how you feel.
Be sure to tell us about all the medications you are taking or have taken shortly before starting warfarin treatment, as well as new prescriptions if you are already taking warfarin therapy. Many drugs can increase or decrease the effect of warfarin on blood clotting. Keep all prescriptions and write down the names of medications you take. The table shows the most commonly prescribed drugs that can affect the effectiveness of warfarin.
How to take medications correctly
In what situations is this examination prescribed?
This examination is prescribed during treatment with indirect anticoagulants - vitamin K antagonists (neodicoumarin, warfarin, syncumar), which reduce the level of prothrombin in the blood, thus thinning it.
Regular monitoring of the indicator allows you to control the dosages of the above drugs to avoid bleeding or blood clots.
When is it necessary to take indirect anticoagulants?
In what situations is it necessary to regularly take a blood test for INR and prothrombin?
- Treatment and prevention of thrombosis of the superficial and deep veins of the lower extremities;
- Varicose veins;
- Acute coronary syndrome;
- Cerebrovascular accident in the acute stage (ACVA);
- PE (pulmonary embolism);
- Permanent form of atrial fibrillation;
- Heart disease;
- Thrombophlebitis;
- The presence of artificial valves in the heart;
- The presence of a vena cava filter (a filter in a large vein of the body that prevents thrombotic masses from entering the veins of the lower extremities and pelvic organs to the heart and lungs.
It must be remembered that when using warfarin and other anticoagulants, the INR level is increased and should be kept within the range of 2.0 - 3.0 (the optimal value is 2.5), and with prosthetic heart valves from 2.5 to 3.5. Patients with an INR value above 6.0 require urgent treatment.
If a person is not treated with anticoagulants, then a deviation of the INR from the norm can cause serious pathological changes in the body. Let's consider in what situations the level of this indicator may change.
Do I need to prepare for an INR test?
First of all, you need to remember that blood to determine the INR value is taken from a vein. A prerequisite is on an empty stomach. This means that you cannot eat or drink sugary water 6-8 hours before. At the same time, you should not fast for more than 10 hours before donating blood, as this will distort the data.
The day before the test, you do not need to do heavy physical work. If the patient jogs in the morning every day, before going to the laboratory, you will have to abandon the activity and reschedule it for the evening. Since jogging will affect the speed of blood flow, blood oxygen saturation and its composition.
Any daily medication intake should also be taken into account - the evening dose on the eve of sampling should be taken no later than 17:00. And triple the appointment must be rescheduled, and you need to take the medicine/get an injection after donating blood.
It is recommended to approach the building of the medical institution 15 minutes before the appointed time in order to have time to put your outerwear in the cloakroom, take your time, find an office and calm down before the procedure. Even slight anxiety associated with the fear of being late can affect the composition of the blood.
We must not forget that taking oral contraceptives significantly distorts the actual state of the coagulation systems due to the elements included in the composition that prevent the formation of blood clots. Therefore, an INR test should be scheduled on the fourth day after completing a three-week course of birth control pills. In other words, the test can be taken closer to the end of the week during which withdrawal bleeding occurs. If this is difficult, you must tell the laboratory assistant the name of the drug you are taking so that he takes its effect into account when calculating the result.