New drug Salmecort in the basic therapy of bronchial asthma
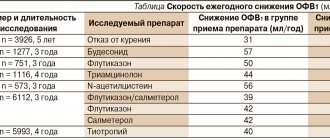
The main anti-inflammatory drugs for the treatment of asthma are inhaled glucocorticosteroids (ICS). Controlled studies conducted taking into account the requirements of evidence-based medicine have shown the effectiveness of ICS in terms of improving respiratory function, reducing airway hyperresponsiveness and severity of symptoms, reducing the frequency and severity of exacerbations (level of evidence, A) [6–8].
In the 1970s Selective β2-receptor agonists entered clinical practice, which had a predominant effect on bronchial smooth muscle and clinically insignificant activity against α- and β1-receptors. Patients who regularly took short-acting β2-agonists before taking ICS demonstrated greater clinical efficacy of therapy than those who took these drugs only as needed. This led to the development of selective long-acting β2-agonists (LABAs). In the treatment of BA, inhaled salmeterol or formoterol are used, which in combination with ICS are the basis of basic therapy for BA. Including them in the treatment regimen of patients whose asthma cannot be completely controlled with various doses of ICS allows one to achieve better control over the disease than simply increasing the dose of ICS by 2 times or more (level of evidence, A) [9–11]. ICS and LABA should be considered as synergists, due to their complementary effects at the molecular and receptor levels [12–15]. The high anti-inflammatory effect of the combined use of ICS and LABA is an argument in favor of using this therapeutic approach for BA, which is accompanied by inflammation of the bronchial mucosa, its swelling, plasma exudation (increased vascular permeability), hypertrophy of smooth muscle cells and desquamation of the epithelium.
In 2005, 2008 and 2010 The US Food and Drug Administration (FDA) has further assessed the safety of LABAs in asthma. From the data presented, it follows that the increased risk is observed primarily in a very specific group of patients - black Americans who did not receive therapy with inhaled hormonal drugs before starting LABA treatment. An increased risk of severe exacerbations was also noted in cases where treatment with this group of drugs was started against the background of a pronounced deterioration or an existing exacerbation of BA [16].
Long-acting β2-agonists can only be prescribed in addition to ICS. Regular use of LABAs for routine therapy requires their mandatory combination with ICS. Doctors should be aware that the use of monotherapy with β2-agonists causes the development of the phenomenon of down-regulation of β2 receptors, which can lead to serious consequences for patients, including the development of asthmatic conditions.
A combination of fluticasone propionate (FP) and salmeterol xinafoate (SAL). The components that make up these drugs have been used for quite a long time: FP - since 1993, SAL - since 1990.
FP is one of the most highly active anti-inflammatory drugs available today. The drug has low systemic bioavailability (~1%), and absolute bioavailability is 10–30% depending on the type of inhaler. FP has a high affinity for glucocorticoid receptors and has a long-lasting relationship with the receptor. To prevent hoarseness and the development of candidiasis, when taking FP, you should follow the same rules as when taking other ICS, i.e., rinse your mouth and throat with water after inhalation. Due to its high anti-inflammatory effect, FP is also indicated for patients with severe asthma and dependence on systemic steroids [17].
SAL is an inhaled LABA. Clinical studies have shown that LABAs have a stabilizing effect on mast cells and inhibit their IgE-mediated release of histamine, which leads to a decrease in its systemic and local concentrations [18]. SAL is prescribed only as a drug for basic therapy and is not used as needed, during exacerbation of the disease, asthmatic condition, or to relieve attacks of difficulty breathing. Only recommended doses should be used, and short-acting β2-agonists should be used to relieve symptoms. Note that SAL also has a number of unexpected properties - in particular, it causes a decrease in the pathogenicity of Pseudomonas aeruginosa and has a protective effect against Haemophilus influenzae in cultures of the respiratory tract epithelium [19–21]. SAL is a highly safe drug, as proven by numerous clinical studies.
The first fixed-combination drug was Seretide®, containing ICS AF and SAL and classified as a long-acting inhaled β2-agonist.
Combined drug FP and SAL. In a study by S. Kirby et al. It has been shown that when using a combination of SAL and FP in healthy people, no systemic pharmacodynamic or pharmacokinetic interactions are observed [22]. The GOAL (Gaining Optimal Asthma control) study, the results of which formed the basis of the GINA control strategy (2006), demonstrates the benefits of combination therapy with ICS + LABA for moderate to severe asthma [23]. The results of the GOAL study are of important practical importance, since it formulates criteria for the effectiveness of asthma treatment. According to the GOAL study, about 40% of asthma patients treated with a fixed combination of SAL/FP achieved complete control of asthma after 12 months. treatment. It is equally important that in the group that received a fixed combination as basic therapy, there were significantly more patients who achieved complete control over BA than in the case of AF monotherapy. Thanks to the GOAL study, an important conclusion was made that treatment outcomes can be improved by choosing the most effective basic therapy.
A study by NC Barnes et al demonstrated that in patients with persistent asthma, initial treatment with SAL/AF compared with AF was 1.65 times more likely to achieve well-controlled asthma in patients with 2 signs of poor pre-treatment asthma control and 2.6 times more likely to achieve well-controlled asthma in patients with 3 signs of poor asthma control before treatment [24].
Original drugs and generics. The original drug with a fixed combination of AF and SAL, Seretide®, is widely and successfully used for the treatment of asthma and COPD using methiodized (MDI) and powder (Diskus) inhalers. The use of original drugs is possible only upon receipt of reliably proven results of clinical trials to study the safety and effectiveness of the drugs. Thus, at all stages of clinical trials, all adverse reactions are recorded; This also happens for a number of years after the drugs are introduced to the market. These conditions determine the price of original drugs. When the patent of original drugs expires, the most successful medications begin to be produced in the form of generics - copies of the original drug. Moreover, the copy must be complete, since the results of clinical studies of the original drug are automatically extrapolated to it. Generics are always cheaper than original drugs, which expands the possibilities of therapy. The WHO requirements for generics regarding pharmaceutical and therapeutic equivalence are quite stringent - the generic must act exactly the same as the original drug, have the same effectiveness and safety.
Currently, the drug Salmecort has been introduced to the market, in which a fixed combination of 2 active components - FP and SAL - corresponds in dosage to the original drug produced at MDI. In Russia, an open randomized multicenter study was conducted to test the hypothesis of non-inferior efficacy and safety of the drug Salmecort (25/250 mcg, in the form of a dosed inhalation aerosol) compared with the drug Seretide® (25/250 mcg, in the form of a dosed inhalation aerosol ) in the treatment of patients with persistent BA and in need of combination therapy with high doses of ICS and long-acting β2-adrenergic agonists.
Objectives of this study:
1. Comparative assessment of the level of asthma control and its dynamics during the study.
2. Comparative assessment of the safety and tolerability of Salmecort and Seretide®.
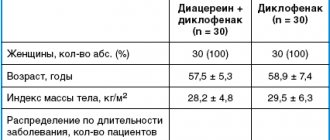
Doctors from 5 leading medical institutions in Russia took part in the study. The diagnosis of asthma was made by a physician in accordance with the practice of the medical institution. After signing informed consent to participate in the study, patients (113 people) were screened; the introductory period lasted an average of 14 days. During this time, the investigator assessed the patient's compliance with inclusion/non-inclusion criteria and disease stability. Then, 107 patients who met the inclusion/exclusion criteria were randomized into 2 treatment groups.
Patients of the 1st group (n=56) were prescribed Salmecort, 2 inhalations 2 times a day, patients of the 2nd group (n=51) were prescribed Seretide®, 2 inhalations 2 times a day. The first drug intake was carried out in the center under the supervision of medical personnel after spirometry was performed. The investigator instructed the patients how to administer the drugs correctly.
Patients took the drugs daily for 12 weeks. They were systematically subjected to spirometry. Patients were required to keep a daily diary - in the morning and evening, record peak flow readings, as well as the presence of asthma symptoms and the need for bronchodilators. During the period of taking the study drugs, patients were scheduled for 3 visits to the center with a frequency of 4 weeks. After the final visit on the 85th day from the start of treatment, the patient’s participation in the study ceased, and further therapy was carried out by the attending physician.
When analyzing the effectiveness, it was revealed:
- The number of patients with a positive response to treatment according to pulmonary function tests was 35 (64.81%) in the Salmecort group and 25 (49.02%) in the Seretide® group. The odds ratio for Salmecort/Seretide was 1.92 (0.88–4.2) and the relative risk was 1.32 (0.94–1.86). The one-sided 95% confidence interval within which the noninferiority hypothesis was tested was 0.99 for the relative risk and odds ratio.
- When comparing BA control indicators (AST questionnaire) at visits 4 and 5, a statistically significant increase was noted in both groups, while the number of patients with an increase in score of at least 1 point was 45 in the Salmecort group and 40 in the Seretide® group (Fig. . 1).
- There was an increase in peak expiratory flow rates according to patient diaries in the period preceding visit 5 compared to the period preceding visit 2.
- During the study periods preceding Visits 4 and 5, a decrease in the total number of asthma attacks was noted. When comparing the drug groups Salmecort and Seretide®, a statistically significant decrease in the total number of asthma attacks was noted in the Salmecort group.
- When assessing changes in the patient’s condition by the doctor at the 5th visit, no statistically significant differences were revealed between the study groups (Fig. 2).
An analysis of the incidence of adverse events, carried out using the “bootstrap” technique, did not reveal a statistically significant difference between treatment groups in this parameter.
In no case was the development of candidal lesions of the mucous membranes of the oropharynx observed during the use of the studied drugs.
The results of the study allowed us to draw the following conclusions:
- The effectiveness of the drug Salmecort (25/250 mcg, in the form of a dosed inhalation aerosol) in 12-week treatment of patients with persistent asthma is not less than the effectiveness of the Seretide® drug (25/250 mcg, in the form of a dosed inhalation aerosol).
- Based on the safety data obtained, it can be concluded that Salmecort has a favorable safety profile and tolerability.
It should be remembered that both Seretide® and Salmecort are not prescribed for the relief of asthma symptoms. For this purpose, it is preferable to prescribe short-acting β2-agonists. If it is necessary to increase the dose of ICS, the permissible dose of SAL should not be exceeded. In this case, the patient should be prescribed a drug with a higher content of FP.
Salmecort, 1 piece, 25 mcg+125 mcg/dose, dosed aerosol for inhalation
Salmecort is not intended for the relief of acute symptoms, since in such cases a fast- and short-acting inhaled bronchodilator (for example, salbutamol) should be used. Patients should be advised to always have medication available to relieve acute symptoms.
The combination of salmeterol and fluticasone propionate can be used for initial maintenance therapy in patients with persistent bronchial asthma (daily occurrence of symptoms or daily use of drugs to relieve attacks) if there are indications for the use of corticosteroids and their approximate dosage has been determined.
More frequent use of short-acting bronchodilators to relieve symptoms indicates worsening disease control, and in such situations the patient should consult a doctor.
A sudden and increasing deterioration in asthma control is potentially life-threatening, and in such situations the patient should also consult a doctor. The physician should consider a higher dose of GCS. If the dose of Salmecort used does not provide adequate control of the disease, the patient should also consult a doctor.
Patients with asthma should not sharply reduce treatment with Salmecort due to the risk of exacerbation; the dose of the drug should be reduced gradually, under the supervision of a physician.
In patients with COPD, drug withdrawal may be accompanied by symptoms of decompensation and requires medical supervision. In patients with COPD receiving Salmecort, the incidence of pneumonia may increase (see "Side effects"). Clinicians should be aware of the possibility of pneumonia in patients with COPD, since the clinical presentation of exacerbation of COPD and pneumonia are often similar.
Any inhaled GCS can cause systemic reactions, especially with long-term use in high doses; however, the likelihood of such symptoms occurring is much lower than with treatment with oral corticosteroids (see “Overdose”). Possible systemic reactions include Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma. Therefore, when treating asthma, it is important to reduce the dose to the lowest dose that provides effective control of the disease.
In emergency and planned situations that can cause stress, you must always remember the possibility of suppressing adrenal function and be prepared to use GCS (see “Overdose”).
When carrying out resuscitation measures or surgical interventions, it is necessary to determine the degree of adrenal insufficiency.
It is recommended to regularly measure the height of children who receive long-term therapy with inhaled corticosteroids.
Patients transferred from oral corticosteroids to inhaled fluticasone propionate therapy, due to the possibility of adrenal suppression, should be treated with extreme caution and their adrenal function should be regularly monitored. When transferring patients from taking systemic corticosteroids to inhalation therapy, allergic reactions (for example, allergic rhinitis, eczema), which were previously suppressed by systemic corticosteroids, may occur. In such situations, it is recommended to carry out symptomatic treatment with antihistamines and/or topical drugs, incl. GCS for local use.
After starting treatment with inhaled fluticasone propionate, systemic corticosteroids should be withdrawn gradually, and such patients should have a special patient card containing an indication of the possible need for additional administration of corticosteroids in stressful situations.
In patients with exacerbation of bronchial asthma, hypoxia, it is necessary to control the concentration of potassium ions (K+) in plasma.
There are very rare reports of increased blood glucose levels, and this should be remembered when prescribing a combination of salmeterol with fluticasone propionate to patients with diabetes mellitus (see “Side effects”).
Due to the potential for systemic effects of GCS, including Cushing's syndrome and adrenal suppression, the combined use of fluticasone propionate and ritonavir should be avoided unless the potential benefit to the patient outweighs the risk associated with the systemic effects of GCS (see Interactions). .
When taking salmeterol, the risk of serious respiratory adverse reactions or death in African-American patients is believed to be higher than in other patients. The significance of pharmacogenetic factors or other causes is unknown. The effect of concomitant use of inhaled corticosteroids on the risk of death in patients with asthma has not been studied.
Like other inhaled drugs, Salmecort can cause paradoxical bronchospasm, manifested by an increase in shortness of breath immediately after use. In this case, you should immediately use a fast- and short-acting inhaled bronchodilator, discontinue Salmecort and, if necessary, begin alternative therapy (see “Side effects”).
Adverse reactions associated with the pharmacological action of beta2-agonists, such as tremor, subjective palpitations and headache, may occur. However, these reactions are short-term in nature, and their severity decreases with regular therapy (see “Side effects”).
Impact on the ability to drive vehicles and operate machinery.
Clinical studies have not provided data on the effect of the drug on the ability to drive vehicles and other mechanisms, but the side effects that the drug may cause should be taken into account.
Salmecort aeros d/ing doses 25mcg+250mcg 120DOSES
special instructions
This combination is not intended for the relief of acute symptoms, since in such cases a fast-acting, short-acting inhaled bronchodilator (eg, salbutamol) should be used.
More frequent use of short-acting bronchodilators to relieve symptoms indicates worsening disease control, and in such situations the patient should consult a doctor.
Sudden and increasing deterioration in control of bronchospastic syndrome poses a potential threat to life, and in such situations the patient should also consult a doctor.
Patients with asthma should not abruptly stop treatment with this combination; the dose of the drug should be reduced gradually under the supervision of a physician. In patients with COPD, drug withdrawal may be accompanied by symptoms of decompensation and requires medical supervision.
Any inhaled GCS can cause systemic effects, especially with long-term use in high doses; however, the likelihood of such symptoms occurring is much lower than with treatment with oral corticosteroids. Possible systemic reactions include Cushing's syndrome, Cushingoid features, adrenal suppression, growth retardation in children and adolescents, decreased bone mineral density, cataracts, and glaucoma. Therefore, when treating asthma, it is important to reduce the dose to the lowest dose that provides effective control of the disease.
In emergency and planned situations with the likelihood of stress, the possibility of suppressing the function of the adrenal cortex and the need to use GCS should always be taken into account.
When carrying out resuscitation measures or surgical interventions, it is necessary to determine the degree of adrenal insufficiency.
It is recommended to regularly measure the height of children who receive long-term therapy with inhaled corticosteroids.
Due to the possibility of adrenal suppression, patients switched from oral corticosteroids to inhaled fluticasone propionate therapy should be treated with extreme caution and their adrenal function regularly monitored.
After starting treatment with inhaled fluticasone, systemic corticosteroids should be withdrawn gradually, and such patients should have a special patient card containing an indication of the possible need for additional administration of corticosteroids in stressful situations.
In patients with exacerbation of bronchial asthma, hypoxia, it is necessary to monitor the concentration of potassium in plasma.
There are very rare reports of increased blood glucose levels; this should be taken into account when using this combination in patients with diabetes mellitus.