Doctors Cost
Price list Doctors clinic
Cerebrovascular accident (CVA) is a reduction in blood access to the brain. This is a real vascular catastrophe. The brain weighs approximately 2% of a person's body weight. A relatively small organ consumes 20% of all incoming energy. The brain does not accumulate the substances necessary for its activity. For normal functioning, it needs a continuous flow of glucose, oxygen, and some other elements supplied with the blood.
Cerebral circulation is distinguished by a multi-level system of redundant vessels and several regulatory mechanisms. But sometimes this is not enough. Cutting off blood supply to the brain for 10 seconds is enough to cause irreparable harm.
Causes of circulatory disorders in the brain
- Systolic pressure is less than 60 or more than 180 millimeters of mercury.
- Insufficient metabolic control, accompanied by unreasonable dilation of cerebral vessels.
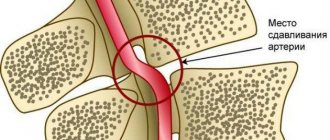
- Atherosclerosis of cerebral vessels.
- Decreased blood oxygen saturation.
The compensatory capabilities of the brain are great. Vascular anastomoses allow blood to be distributed throughout the entire volume of the organ, even if the inflow through the left or right carotid artery is disrupted. However, these mechanisms do not work for long; after some time, oxygen starvation develops, and the first signs of the disease appear. This is why it is important to seek medical help immediately.
Most often, NMC develops against the background of:
- history of traumatic brain injury;
- chronic venous insufficiency;
- hypertension,
- atherosclerosis, ischemic heart disease,
- osteochondrosis,
- diabetes mellitus,
- hormonal imbalance,
- excess weight,
- stress, stress
- chronic fatigue,
- lipid metabolism failure,
- drinking alcohol,
- smoking.
How does blood circulation function between mother and fetus?
The mother-fetus circulatory system is based on such anatomical structures as the placenta, umbilical arteries, and veins.
Blood enters the placenta through the uterine arteries. The structure of their walls is distinguished by the presence of a muscle layer that can contract and block the lumen. Before pregnancy occurs, this mechanism helps reduce blood loss during menstruation.
At 4–5 weeks of consolidation of the fertilized egg (gestation process), the muscle layer disappears. Blood flow to the placenta no longer depends on vascular contraction. And by the sixteenth week, the arteries are transformed for constant blood supply. This turns out to be dangerous when bleeding occurs, since it is impossible to stop it by reducing the lumen of the vessels.
Under normal conditions, the placenta is fixed on the inner surface of the uterus with the help of villi that penetrate deep into the thickness of the mucosa. They grow into the walls of blood vessels and come into direct contact with maternal blood.
What happens here at the cellular level:
- exchange between the maternal body and the fetal bloodstream;
- two differently directed flows meet;
- the transfer of necessary substances takes place (diffusion).
The other part of the general blood circulation is provided by the vessels of the umbilical cord (normally there are 2 arteries and a vein). The main volume of blood flows to the fetus through the arteries, and flows through the veins towards the placenta.
As the uterus grows, the arteries expand and form anastomoses.
Violation of fetal-placental blood flow is most difficult for a developing child. Creates conditions for an unsatisfactory prognosis for the development of internal organs and systems and the birth of a healthy baby.
Acute cerebral circulatory disorders. Symptoms
According to the World Health Organization (WHO), 17 million people are diagnosed with stroke every year. Five million of them die, another 5 million remain disabled.
Table 2. Types of NMC
| NMK | Kinds | Development mechanism |
| Ischemic. | Cerebral infarction (ischemic stroke). | Stopping the blood supply to a part of the brain. |
| Transient NMC. | Lasts up to a day. | |
| Transient cerebrovascular ischemic attack. | Occurs periodically. | |
| Hemorrhagic. | Intracerebral hemorrhage. | Rupture of a vessel with subsequent effusion of blood into the brain tissue. |
| Subarachnoid hemorrhage. | Hemorrhage into the subarachnoid space. | |
| Non-purulent thromboembolism. | Thrombosis. | Blockage of a vessel by a thrombus. |
| Embolism. | Blocking of a vessel with an embolus. |
How does insufficient placental blood supply threaten the fetus?
All disorders of both uteroplacental and fetoplacental nature lead to oxygen deficiency of the fetus (hypoxia). Complications are caused precisely by this mechanism:
- the formation of the internal organs of the fetus is disrupted, there is a lack of weight, this is called “intrauterine growth retardation”;
- the heart reacts with rapid contractions (tachycardia) or arrhythmias, bradycardia;
- the composition of electrolytes and acid-base balance are disrupted;
- the functioning of the endocrine system is disrupted, the fetus experiences a hormonal imbalance;
- fat depots are not formed.
The most severe complications are fetal death and threatened miscarriage.
Myomatous nodes take away part of the vascular network from the fetus for its growth
Signs and symptoms of acute cerebrovascular accidents depending on the area of brain damage
- The basin of the internal carotid artery – paresthesia, paresis, paralysis on the opposite side of the face and body. Pathology of speech and vision in one eye.
- Vertebrobasilar basin - systemic dizziness, pain in the back of the head, unsteady gait, loss of visual fields, double vision, inability to swallow and speak.
- Brain stem - eye paralysis, hearing loss, swallowing and speech disorders, paresthesia of the facial skin.
- Medulla oblongata – bilateral paralysis.
- Temporal lobe – loss of spatial and temporal orientation, memory impairment.
Symptoms of uteroplacental blood flow disorder 1a degree
If this pathology is in the stage of compensation, the expectant mother will not feel any pronounced deviations. In this case, you can find out about the disease only after examination. Obvious signs of the disease accompany the acute form and chronic decompensation. This pathology is accompanied by the following symptoms:
- a sharp increase or cessation of motor activity of the embryo;
- too slow growth of the abdomen (the diameter of its circumference does not correspond to the normative indicators corresponding to the specific gestational age);
- gestosis;
- arterial hypertension;
- strong weight gain of the expectant mother;
- swelling of the legs below the knees;
- proteinuria.
In some cases, bleeding may occur. This symptom most likely indicates placental abruption. If bleeding occurs, you should immediately see a gynecologist.
- Violation of uteroplacental blood flow 1a degree: what is it, what are the consequences for the child?
Diagnostics of NMC
- Duplex ultrasound examination of blood vessels.
- Contrast venography, angiography.
- CT, MRI.
- Transcranial Doppler.
- Laboratory tests - clinical, biochemical blood tests with determination of lipid profile, hematocrit.
- Fundus examination.
- Detection of hearing loss, smell, taste, and pathology of the vestibular apparatus.
Symptoms of ischemia of the lower extremities
Since ischemia of the lower extremities has such dangerous consequences, if signs of ischemia appear, you must consult a doctor. In medicine, a condition of critical ischemia is distinguished, in which urgent measures are needed to normalize blood circulation. Critical ischemia is a condition characterized by one of the following symptoms:
Leg muscle pain
Ischemia is manifested by pain in the leg muscles at rest (mainly at night).
Ischemic pain cannot be relieved with painkillers. It becomes easier if you keep your leg down (patients often lower their leg off the bed while sleeping). However, in this case, relief is achieved due to the deterioration of the outflow of venous blood, which, accumulating in the tissues, further compresses the arteries; the influx of arterial blood becomes even less, as a result of which the development of trophic phenomena (ulcers and gangrene) rapidly progresses.
Trophic ulcers
Ulcers occur as a result of lack of nutrition. First of all, the most distant parts of the leg - the toes - are affected, then the entire foot.
Intermittent claudication
Intermittent claudication manifests itself as a forced stop when walking due to pain in the calf muscles. Similar stops may be required every 30 meters of the route.
Intermittent claudication is the main symptom of impaired blood supply to the lower extremities. If the arterial blood flow is insufficient, during physical activity (for example, walking), after some time, numbness and coldness of the leg are observed, as well as pain in the calf muscles, which prevents walking further. It is enough to just stand in one place for a while, and the pain will go away. In the early stages, pain occurs no earlier than after a kilometer of travel. But this is already a reason to consult a doctor, since the disease tends to progress, and in the future the distance that can be walked without pain will decrease.
Treatment
In case of acute cerebrovascular accident, treatment should be started immediately. The minutes count down.
For chronic pathology, the course of therapy is drawn up individually after diagnosis. The doctor takes into account age, concomitant diseases, and stage of the process.
Basic treatment includes, among other things, 3 mandatory recommendations.
- Nutrition correction. It should help normalize lipid metabolism and reduce blood cholesterol. Usually the consumption of meat, deli meats, and animal fats is limited. It is recommended to eat more vegetables, herbs, and dairy products.
- Increased physical activity. Helps normalize blood flow and increase vascular tone.
- Weight loss. Correcting your diet and increasing physical activity usually helps you lose extra pounds and be in good physical shape. If this is not enough, seek the help of an endocrinologist.
In case of cerebrovascular accident, with various symptoms, treatment is prescribed:
- physiotherapy;
- physical therapy;
- medicines;
- surgical treatment.
Excursion into physiology
The uninterrupted supply of substances necessary for the nerve cells of the brain and the cleansing of waste are carried out by the cerebral circulatory system, where arterial blood carries oxygen and nutrition to the brain, and venous blood removes toxins and metabolic products.
The vessels of the brain have a unique, perfect structure that ideally regulates blood flow, ensuring its stability. They are designed in such a way that with an increased flow of blood into large vessels, the strong pulse impulse of the blood coming from the heart is weakened due to numerous bends (siphons) of the vessels along the vascular bed, which contribute to the pressure drop and smoothing of the pulsating blood flow. Due to complex regulatory mechanisms, when total blood pressure increases, the pressure in the brain remains stable for a long time. Regulatory systems allow blood flow to be redistributed from parts of the brain with less load to areas with increased brain activity.
The brain has an autonomous regulatory system, which allows it to be in a healthy functional state and control the processes of continuous adaptation of the body to constantly changing conditions of the external and internal environment. In a state of functional rest, the brain receives 750 ml of blood per minute, which is 15% of cardiac output. In children, blood flow activity is 50–55% higher, and in elderly people it is 20% lower than in adults.
It should be noted that the gray matter of the brain (cell bodies of neurons) is supplied with blood more intensively than the white matter (conducting pathways), which is due to greater cell activity. Thus, during intense mental work, local blood flow in the cerebral cortex can increase 2–3 times compared to the resting state.
The brain has the richest capillary network. Nerve cells are not only intertwined, but also penetrated by capillaries. The vessels of the brain are connected to each other by collaterals (“bridges”). Arterial collateral circulation of the brain, important for maintaining normal blood flow, plays a particularly significant role in compensating for circulatory disorders when one of the cerebral arteries is blocked.
With a high intensity of blood flow in the vessels of the brain, the blood pressure in them is maintained relatively constant. A complex chain of regulatory mechanisms protects the brain from a drop in blood pressure and hypoxia (decreased oxygen). Along the path of blood flow to the brain, there are many sensitive cells (pressoreceptors, chemoreceptors) that can respond to blood pressure and regulate heart rhythm and vascular tone.
The activity of the vasomotor centers of the brain is associated not only with nervous and humoral regulation mechanisms, but also with the autonomic regulation system, which allows, despite significant fluctuations in total blood pressure, to maintain cerebral blood flow at a constant level.
Thus, cerebral circulation is provided with complex regulatory mechanisms that make it possible to maintain a constant supply of the substances it needs.
With excessive blood supply to the brain, excessive hydration (fluid accumulation) may occur, followed by the development of edema and damage to vital centers that are incompatible with life. The cause of excess blood supply can be, for example, an increase in systemic blood pressure to 160–170 mm Hg. Art. and higher.
In the problem of impaired blood supply to the brain, much attention is paid to arteries. But venous circulation is no less important. The veins carry out the removal of waste substances (toxins) with the blood - that is, cleansing the brain. Thanks to these vessels, constant intracranial pressure is maintained.
Violation of the venous outflow leads to stagnation of blood and accumulation of fluid in the brain, causes hydrocephalus with compression of the brain centers, and contributes to the occurrence of phlebitis and thrombophlebitis.
There is one more feature of the cerebral veins that must be taken into account. The wall of a venous vessel in the brain does not have a valve apparatus, unlike, for example, the veins of the extremities (valves help withstand loads by moving blood upward and preventing it from moving in the opposite direction). Therefore, venous blood in the vessels of the brain passes freely in both directions, depending on the pressure that arises. This creates a danger of rapid spread of infection from the sinuses and eye sockets, which is facilitated by the atomic structure of the nose and its paranasal sinuses, located in close proximity to the brain. When coughing, venous pressure increases, reverse venous flow, congestion, and brain hypoxia become possible. There are known cases of loss of consciousness during a coughing attack in the presence of a chronic respiratory tract disease and in young children when they “go into a fit” of coughing during illness and crying and screaming until they cough.
It becomes clear why long-term respiratory problems, accompanied by constant swelling and coughing, can cause cerebrovascular accidents. Because they not only cause brain hypoxia, but also disrupt venous outflow and, being a constant source of infection, contribute to its penetration into the brain.
An ophthalmologist, for example, can observe manifestations of congestion in the brain (dilated, blood-filled vessels of the fundus). But this is also visible to the naked eye: red, puffy eyes after sleep (due to drinking alcohol the night before, overeating at night, lack of sleep) are a symptom of congestion in the brain.
After a brief excursion into physiology, it becomes clear that the reasons for the deterioration of cerebral circulation may be associated with disturbances in the flow of blood to the brain and the outflow of blood from the brain.
Prevention
To avoid the sudden appearance of cerebrovascular accidents, you need to lead an active lifestyle. Do as much physical activity as possible, morning exercises. Walk more, swim, take a contrast shower. Be sure to monitor blood pressure.
You should stop smoking and drinking alcoholic beverages.
It is recommended to consume more foods rich in vitamins C, D, E, and fiber. Minimize the intake of fried, fatty, spicy, salty foods. If you have chronic diseases, they must be treated. If you have hypertension, monitor your blood pressure.
Why blood circulation may be impaired
Causes of fetoplacental insufficiency (impaired blood circulation between mother and child):
- Low placentation (attachment of the placenta to the wall of the lower parts of the uterus or “presentation”). The thin muscular layer of the lower uterus is not able to provide sufficient blood flow to the fetus. If there is no migration of the placenta (advancement in the upper part of the uterus), the situation threatens to worsen the pathology.
- Late toxicosis of pregnant women. It affects the small vessels of the uterus, which disrupts blood circulation.
- Drop in hemoglobin level or anemia. This condition causes an accelerated heartbeat in the mother, altering the normal blood circulation in the uteroplacental circle.
- Incompatibility of the Rh factors of the blood of mother and baby, causing anemia in the fetus and immune conflict.
- High blood pressure in the mother due to heart problems, swelling, stress.
- Pathology of the umbilical arteries , for example, the presence of only one umbilical artery.
- Multiple pregnancy , requiring more nutrients.
Some maternal diseases contribute to the spread of pathology, in particular:
- Acute infections, the pathogens of which are capable of penetrating the placenta;
- Uterine defect (“bicornuate” uterus, having a septum in the middle dividing it into two halves). Fetal development occurs in only one of them. The threat is posed by the compression factor of the growing fetus and the disruption of blood flow to it. In such situations, a disturbance of uteroplacental blood flow on the left, grade 1a or on the right, often occurs.
- Diabetes. It affects the walls of the uterine vessels.
- Deviations of the uterine epithelium (endometriosis).
- Uterine tumors. The size of a benign tumor (fibroid) determines how much the fetus will suffer from insufficient blood supply. The larger the fibroids, the higher the risk of failure. Hormonal changes caused by pregnancy stimulate the growth of tumors. The presence of this disease requires constant monitoring of the uterine blood supply.