Sepsis in adults: symptoms and treatment
Blood poisoning (sepsis) is an acute or chronic disease that occurs due to the penetration of bacterial, viral or fungal flora into the body.
Many people believe that blood sepsis develops after the suppuration of severe wounds, however, in reality there are many other “gates” through which the infection can enter the circulatory system, and very often it turns out that the true causes of the disease cannot be found out.
Classification
Depending on the speed of development of the infectious process, the following types of septic conditions are distinguished:
- Fulminant sepsis, which develops within three days after infection with pathogenic pathogens;
- Acute, in which clinical symptoms develop no earlier than a week after identifying the primary source of infection;
- Subacute septic condition develops from a week to four months;
- Chronic sepsis in adults will be considered when the first symptoms appear no earlier than six months later; it usually develops in patients with immunodeficiencies of various etiologies.
In epidemiological terms, when characterizing this pathology, the following types are distinguished:
- Nosocomial infection. It develops as a result of surgical, gynecological, diagnostic or other medical procedures that occur after medical care.
- Community-acquired infection. The cause is any infectious disease, for example, intestinal infection, meningitis, ENT pathology, etc.
According to the characteristics of the manifestation of clinical symptoms of sepsis, the following are distinguished:
- Toxemia, in which a systemic inflammatory process develops due to the spread of infection from the primary focus;
- Septicemia, which is characterized by the absence of formation of secondary purulent foci;
- Septicopyemia, with such foci present.
Types of sepsis
It is not enough to know what sepsis is; you need to understand how the pathology is classified. First of all, they distinguish:
- Primary sepsis. It develops against the background of any dormant infection in the body and is quite rare.
- Secondary sepsis. This is a common pathology that is associated with the presence of a purulent focus in the body.
Sepsis is classified according to its duration:
- Fulminant. It is characterized by the rapid onset of symptoms and their intensification. In a short time, the functioning of most internal organs occurs. If the patient's condition cannot be stabilized, death may occur within a couple of days.
- Spicy. Symptoms increase slowly, the process lasts up to 6 weeks.
- Subacute. The duration of the process is extended to 3-4 months.
- Recurrent. A characteristic feature is the undulating course of the disease, when periods of stabilization alternate with exacerbations.
- Chronic. It is characterized by a long course - up to several years. The source of inflammation does not heal, despite the measures taken, and against the background of this, the body’s protective reactions worsen.
Causes of blood poisoning
The causative agents of sepsis are a variety of microorganisms: staphylococci, meningococci, pneumococci, Escherichia coli, Mycobacterium tuberculosis, Klebsiella, Candida type fungi, and viruses of the herpetimorph group.
It is worth noting that the development of sepsis is associated not so much with the properties of the pathogens themselves, but with the state of the human body and its immunity. A decrease in the effectiveness of protective barriers leads to the fact that our security systems can no longer localize harmful pathogens in a timely manner, much less prevent their penetration into various organs.
If we talk about the most common methods of infection with sepsis, it is worth noting that they depend on the type of specific pathogen. Each of them has its own characteristics and epidemiological prerequisites. The only exceptions are cases where patients develop nosocomial sepsis, the symptoms of which sometimes make themselves felt even after inhaling poorly purified air in the wards (potentially dangerous microorganisms are detected in 60% of samples).
It is also possible to identify other routes of infection that determine the main symptoms of sepsis:
- obstetrics and gynecology;
- otogenic;
- cryptogenic;
- percutaneous sepsis;
- oral;
- blood poisoning resulting from surgical and diagnostic procedures.
Identifying the “gate” through which sepsis entered is of great importance for the successful treatment of patients. Early diagnosis of sepsis allows you to identify the infection in time, separate it from cases of short-term presence of microbes in the blood and activate the body's defense systems.
As we said above, for the development of sepsis certain conditions must be met, in particular:
- the formation of secondary foci, which subsequently also supply pathogens;
- the presence of a primary focus (it must be associated with the circulatory system or lymphatic vessels);
- repeated penetration of pathogens into the blood;
- the body’s inability to organize the necessary immune defense and provoke reactions against harmful microbes.
Only if all these conditions are met and the patient has appropriate clinical signs of infection, doctors diagnose blood sepsis. The development of sepsis is provoked by serious diseases (diabetes, cancer, rickets, HIV, congenital defects of the immune system), therapeutic measures, injuries, long-term use of immunosuppressive drugs, radiotherapy and some other factors.
Stages of sepsis development
The development and course of the septic process is individual and depends both on the properties of the pathogen and on the characteristics of the patient’s body. However, several phases of the course of this disease can be distinguished:
- Voltage phase. In response to the introduction of the pathogen, the body’s defense systems are activated and mobilized, in particular the pituitary-adrenal system is activated.
- Catabolic phase. The patient's condition deteriorates due to metabolic disturbances. The processes of metabolism of proteins, fats and carbohydrates are enhanced, and they are extracted from the “depot”. Disorders of water-electrolyte metabolism and acid-base status also develop.
- Anabolic phase. At this time, recovery processes begin. This primarily concerns structural proteins.
- Rehabilitation phase. During this period, further restoration of metabolic processes occurs. In some cases, complete recovery is not possible.
As for the duration of the disease, everything is again individual. In some, stronger patients, sepsis is relieved within 3-4 weeks, in others it can last for years, periodically subsiding and flaring up.
In addition, when diagnosing sepsis, the following conditions are distinguished.
Toxic-resorptive fever
Toxic-resorptive fever is a condition that develops when bacterial toxins or tissue decay products are absorbed from the primary pathological focus. As a rule, this is typical for bacterial infections of wounds, catheters, etc. There are common typical syndromes that accompany infectious processes - fever, changes in general blood and urine tests (leukocytosis, proteinuria). Once the primary lesion is eliminated, the patient's condition stabilizes.
Septicemia
Septicemia is a form of sepsis in which there is a pronounced intoxication syndrome, hyperergy (increased reactivity of the body) and a rapid course. Septic foci are either minimally expressed or absent. This form of sepsis is more typical for children in the first years of life. The clinical picture is more characterized by general manifestations:
- Hemolytic jaundice, accompanied by yellowing of the skin and sclera.
- Rash. It first appears as small pink dots, which grow and merge with each other, forming pale pink or purple spots.
- In some patients, elements of the rash may become blistered or ulcerated. With deep lesions, subcutaneous fatty tissue may be affected with the development of phlegmonous inflammation.
- Hemorrhagic syndrome - hemorrhages in internal organs.
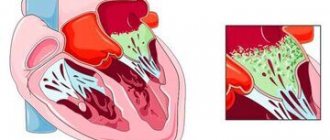
Septicopyemia
Septicopyemia is a form of sepsis in which in the body, in addition to general intoxication, metastatic abscesses begin to appear in organs and tissues, which are the result of bacterial embolism. Most often, the first abscesses are found in the lungs, and then the process spreads to other organs: liver, liver, heart, meningeal membranes, synovial membranes. Abscesses can break through and cause the development of pleural empyema, phlegmon, peritonitis, etc.
The first symptoms of sepsis
The clinical course of sepsis symptoms in adults can be fulminant (rapid development of manifestations within 1-2 days), acute (up to 5-7 days), subacute and chronic. Atypical or “erased” symptoms are often observed (for example, at the height of the disease there may not be a high temperature), which is associated with a significant change in the pathogenic properties of pathogens as a result of the massive use of antibiotics.
Sepsis (see photo) can occur with the formation of local abscesses in various organs and tissues (infection from the primary focus) - the so-called. septicopyemia, in which the course of sepsis depends on the location of the ulcers (for example, an abscess in the brain with corresponding neurological disorders), and without metastatic ulcers - the so-called. septicemia, often with a more rapid course, pronounced general symptoms. With the development of sepsis in newborns (the source is a purulent process in the tissues and vessels of the umbilical cord - umbilical sepsis), vomiting, diarrhea, complete refusal of the child to breastfeed, rapid weight loss, and dehydration are characteristic; the skin loses elasticity, becomes dry, sometimes sallow in color; Local suppuration in the navel area, deep phlegmons and abscesses of various localizations are often detected.
When diagnosing blood poisoning, there are:
- Systemic inflammatory response syndrome. Characterized by changes in body temperature (both upward, more than 38 °C, and downward, below 36 °C), rapid heartbeat (more than 90 beats per minute) and breathing (more than 20 breaths per minute), changes in the number of leukocytes in blood (less than 4x109 or more than 12x109 cells per liter of blood).
- Sepsis. With the same symptoms as in the case of systemic inflammatory syndrome, one of the known pathogens is detected in one of the normally sterile tissues (in the blood, cerebrospinal fluid, urine...), signs of peritonitis, pneumonia, purpura and other local inflammatory processes are revealed.
- Severe sepsis. Characterized in the same way as regular sepsis, but with hypotension, hypoperfusion, or organ dysfunction.
- Septic shock. The most severe condition, after which death occurs in every second patient due to impaired blood supply to organs and tissues. It is defined by the same symptoms as sepsis, when intensive resuscitation measures do not lead to normalization of blood flow and blood pressure levels. Other signs of septic shock include slow urine production and confusion.
In February 2021, the concepts and diagnostic criteria for sepsis were revised. The concepts of systemic inflammatory response syndrome and severe sepsis were recognized as irrelevant, and new definitions were given to the concepts of sepsis and septic shock.
To identify and diagnose sepsis, it is recommended to use the SOFA and qSOFA scales.
Diagnosis of sepsis
Timely diagnosis of sepsis is crucial for the patient’s recovery. The earlier treatment is started, the greater the chances of success. The diagnosis is made on the basis of clinical examination and laboratory and instrumental examination.
Clinical criteria:
- Body temperature is more than 38 degrees or less than 36 degrees.
- Heart rate is more than 90 or exceeds the age norm.
- Respiration rate more than 20 times per minute.
- Presence of edema.
- Confusion.
- An increase in blood glucose levels of more than 7.7 µmol/l in the absence of diabetes.
- Disturbance of hemodynamic processes - a decrease in systolic blood pressure of less than 90 mmHg, or its decrease by more than 40 mmHg. from the usual meaning. [5,6]
Laboratory criteria
A general blood test is performed with a leukocyte count and platelet count. In case of sepsis, leukocytosis is determined by more than 12*109/l or leukopenia when the number of leukocytes is below 4*109/l. There is also the release of immature forms of granulocytes into the bloodstream and a decrease in the number of platelets.
A biochemical blood test shows an increase in C-reactive protein, creatinine, and bilirubin. But these are nonspecific signs that can be observed in other diseases. Therefore, the search for more informative diagnostic methods continues.
Today, the main such markers are procalcitonin, presepsin, and CRP. Based on this laboratory indicator, a diagnosis is made and the dynamics of the disease are monitored.
Bacteriological culture
Detection of microorganisms in the blood is an important, but not mandatory, manifestation of sepsis. Even with the use of the most modern diagnostic systems and careful adherence to material sampling techniques, it is possible to isolate the pathogen from the blood in less than half of the cases. Therefore, a negative culture result in the presence of clinical symptoms should not be regarded as the absence of sepsis, and, conversely, the isolation of microorganisms from the blood in the absence of symptoms should be regarded as transient bacteremia or viremia, but not as sepsis.
However, biological studies should in any case be present as one of the stages in diagnosing sepsis for the following reasons:
- Possibility of determining the etiology of the pathogen.
- Selection or change of antibiotic treatment regimens.
- Monitoring the effectiveness of treatment.
- In some cases, it allows you to determine the source of infection, for example, catheter-related infection, endocarditis, etc.
Book a consultation 24 hours a day
+7+7+78
Neonatal sepsis
In children, as a result of sepsis, many processes in the body are disrupted (blood movement, perfusion). Statistics show that the incidence of the disease in newborns remains high, but this problem is being actively studied.
Sepsis in children can develop as a symptom accompanying other diseases and may not have its own symptoms. This disease is the body’s reaction to the ingress of pathogenic microflora. During the inflammatory process, uncontrolled formation of pus occurs. In newborns, sepsis can occur when exposed to Klebsiella and Pseudomonas aeruginosa, as well as streptococci, enterobacteria or candida. Sometimes the disease occurs when exposed to several microorganisms. Most often, sepsis affects children under one year of age with low body weight.
With the development of a fulminant form of sepsis, septic shock occurs, which in most cases ends in death. The disease leads to a sharp decrease in body temperature, accompanied by severe weakness, lethargy, increased bleeding, pulmonary edema, cardiovascular disorders, and acute renal failure.
Complications of sepsis
- Complications from the respiratory system. Impaired ventilation of the lungs leads to an increase in the air-hematic barrier and, as a result, sweating of fluid into the alveoli. This further disrupts gas exchange and leads to the development of shock lung and respiratory distress syndrome, which is aggravated by fatigue of the respiratory muscles.
- Kidney complications. There is a decrease in the filtration function of the kidneys due to damage to the tubules, which developed as a result of a decrease in pressure. Accompanied by a sharp decrease in urine output, proteinuria, and azotemia.
- Impaired blood clotting due to a drop in platelet levels and the development of disseminated intravascular coagulation syndrome - a dangerous condition in which first there is massive formation of blood clots in the bloodstream, and then massive bleeding due to insufficiency of blood clotting factors.
- Neurological complications. Long-term sepsis can lead to the development of polyneuropathy, which, in particular, leads to weakening of the respiratory muscles and the inability to breathe independently.
- Septic shock is the most severe manifestation of sepsis, accompanied by a persistent decrease in blood pressure that is difficult to restore even with the use of fluid therapy and vasopressors. It develops due to the release of fluid from the blood vessels and due to general dehydration. At the same time, the violations are so severe that they can lead to the death of the patient from multiple organ failure. [13]
Diagnostics
Blood poisoning is diagnosed based on symptoms and data from blood tests for the presence of bacteria, taking into account that at the stage of toxic-resorptive fever and in the chronic course at the stage of remission, bacteremia (presence of microbes in the blood) is not detected.
When diagnosing, changes in blood parameters must be taken into account, which are characterized by:
- high levels of bilirubin and residual nitrogen;
- reduced calcium and chloride content;
- progressive anemia;
- high leukocytosis (abnormally high white blood cell count) or, in the case of weakened patients, leukopenia (decreased number of white blood cells);
- thrombocytopenia - reduced platelet count.
Protein, leukocytes, red blood cells, and increased amounts of urea and uric acid are detected in the urine.
Laboratory methods include:
- Determination of the amount of procalcitonin in the blood: its increased content is considered as a characteristic sign of blood infection
- Isolation of the genetic material of the pathogen that caused sepsis using polymerase chain reaction (PCR) using rapid methods. Within 2 hours, it is possible to identify up to 25 types of microorganisms and pathogenic fungi.
- Bacteriological blood test to identify the active microbe and its reaction to the action of various antibacterial drugs (antibioticogram) to develop an optimal treatment regimen. The sampling is carried out from two different saphenous veins in a volume of 5 - 10 ml, inoculating into a nutrient medium.
The procalcitonin test has a high degree of diagnostic value, allowing you to confirm the diagnosis of bacterial sepsis, septic shock, and differentiate the disease from other pathologies with similar clinical signs.
Signs of septic shock
With septic shock, disruptions in the functioning of the circulatory system begin - oxygen and necessary substances do not reach the body tissues. Septic shock often results in death. In addition to a confirmed infection, septic shock is diagnosed when:
- increased content of lactic acid in the body, which is called serum lactate, in this case oxygen does not fully reach the cells;
- the need to take medications to maintain blood pressure at approximately 65 mmHg.
What consequences?
Complications of sepsis are extremely dangerous and difficult to treat even in intensive care. Let's take a closer look at the most common of them.
- Severe bleeding - can occur as a result of a deficiency of special substances (blood clotting factors and platelets) produced by the liver.
- Acute renal and liver failure - develops under the direct influence of toxins on the kidney, or as a result of blockage of the filtering apparatus of the kidneys with microbial fragments and pus. The removal of metabolic products from the body is disrupted and completely stops, which further aggravates the condition.
- Infectious-toxic shock (ITSH) is a sharp drop in blood pressure under the influence of a large number of microbial toxins. Without emergency medical care, you can die within an hour or even a few minutes. ITS is treated in the intensive care unit.
- Bacterial endocarditis - develops when microbes enter the heart cavity. By causing inflammation, they contribute to the formation of blood clots in its cavity. Subsequently, these blood clots, breaking off and entering the blood vessels of the brain with the bloodstream, can lead to a stroke.
In general, sepsis leads to dysfunction and damage to all internal organs.
Causes of sepsis
Sepsis can be caused by most microorganisms known in epidemiology, including bacteria, viruses (including seasonal influenza viruses), fungi, and parasites. Typically, the infectious agent enters the body from the external environment. Under certain conditions, for example, with immunodeficiencies, the disease can develop from the natural, opportunistic flora of the body, which is normally present in every person. [1]
The presence of infection in itself does not guarantee the development of sepsis. Additional conditions are needed that will lead to generalization of the process and a pathological response of the body. The likelihood of such events increases in the following cases:
- The patient's age is over 75 years.
- Performing surgeries or invasive procedures.
- Presence of injuries and burns.
- Immune system disorders - AIDS, cancer, chemotherapy, the need to use immunosuppressive therapy (for example, after organ transplantation), the need to take high doses of glucocorticosteroids.
- Long-term treatment in a hospital setting.
- Availability of catheters, cannulas, probes and other invasive devices.
- Pregnancy and childbirth.
- Chemical dependence - alcoholism, drug addiction.
- The presence of chronic diseases - chronic renal failure, respiratory failure, diabetes mellitus and much more.
What is needed to treat sepsis?
It is well known that sepsis is extremely difficult to treat. The mortality rate is extremely high and in some situations reaches 50%. However, timely assistance provided reduces this figure significantly.
According to clinical guidelines in 2021, patients with sepsis are treated in intensive care or intensive care units. This is caused by the need to constantly monitor vital signs. During the first 6 hours, doctors’ efforts are aimed at bringing these numbers to a certain value and stabilizing them:
- amount of urine excreted - 0.5 ml/(kg*h) or more;
- oxygen saturation of mixed venous blood - 70% or more;
- central venous pressure - up to 8-12 mm. Hg;
- blood pressure - up to 65 mm Hg. and higher.
This is usually achieved by using various infusion solutions that are poured through a “dropper,” often into several peripheral veins or into one central vein. Sometimes it is necessary to transfuse blood products and add drugs to the solutions that increase blood pressure. These measures alone already reduce the mortality rate of patients by 17% (from 50 to 33).
Treatment consists of eliminating the complications that have arisen, which for the most part are resuscitative.
For example, in case of acute renal failure, hemofiltration, hepatoprotectors and hemodialysis are used, in case of hemodynamic disorders - restoration of vascular permeability and circulating blood volume, in case of cardiac failure - cardiac stimulating and vasotropic drugs, in case of pulmonary failure, mechanical ventilation is used, in case of stress bleeding, H2 histamine blockers/proton blockers are used. pumps/ sucralfate. As for antibiotic therapy, antibiotics should be prescribed based on the results of bacterial studies or against the most likely pathogens.
For the latter case, a table has also been created:
| Localization of the primary focus | Most likely pathogens |
| Lungs (nosocomial pneumonia that developed outside the ICU) | Streptococcus pneumonia, Enterobacteriaceae (E.colli), Staphylococcus aureus |
| Lungs (nosocomial pneumonia developed in the ICU) | Pseudomonias aeruginosa, Acinetobacter spp, as well as the above pathogens |
| Abdomen | Bacteroides spp, Enterococcus spp, Streptococcus spp, Pseudomonias aeruginosa, Staphylococcus aureus |
| Leather and soft tissues | Streptococcus spp, Staphylococcus aureus, Enterobacteriaceae |
| Kidneys | Enterobacteriaceae, Enterococcus spp. |
| Oropharynx | Staphylococcus spp, Streptococcus spp, anaerobes |
| After splenectomy | Streptococcus pneumonia, Haemophilis influenzae |
| Intravenous catheter | Staphylococcus epidermididis, Staphylococcus aureus, enterococci and candida |
When secondary purulent foci form, their surgical treatment is necessary - opening abscesses, removing pus and washing the wounds, excision of the affected areas.
Key Recommendations
A. Initial therapy of sepsis
- Sepsis and septic shock are medical emergencies and therefore initial therapy and resuscitation measures must be started immediately! (best practice guideline – BPS).
- Patients with hypoperfusion should receive at least 30 mL/kg intravenous crystalloid solutions during the first 3 hours of resuscitation (strong recommendation, low-quality evidence).
- Subsequent additional fluid resuscitation is adjusted based on frequent reassessment of hemodynamic status (best practice recommendation - BPS).
- Further assessment of the patient's hemodynamics (eg, cardiovascular function) to determine the type of shock is recommended when the clinical picture does not lead to a clear diagnosis (best practice recommendation - BPS).
- In patients with signs of septic shock who require vasopressors, the initial target mean arterial pressure (MAP) should be 65 mmHg. Art. (strong recommendation, moderate quality of evidence).
- Dynamic hemodynamic parameters, as opposed to static ones, can be used as a predictor of response to fluid therapy, where possible (weak recommendations, low quality of evidence).
- Resuscitation efforts should also aim to normalize lactate levels in patients with sepsis/septic shock, as a major marker of tissue hypoperfusion (weak recommendation, low-quality evidence).
B. Screening for sepsis and improving its quality
- It is recommended that hospitals establish a program to improve the quality of care for sepsis, which would include screening for sepsis in patients with severe illness and in high-risk patients (best practice recommendation - BPS).
C. Diagnosis of sepsis
- Microbiological culture samples (including blood) should be obtained before initiating antibacterial treatment in patients with suspected sepsis/septic shock; as long as it does not significantly delay the initiation of antimicrobial therapy (best practice recommendation - BPS).
D. Antibacterial therapy
- Intravenous antimicrobials should be started immediately after identification of the causative agent and/or within 1 hour of the first symptoms of sepsis/septic shock (strong recommendation, moderate quality of evidence, assessment applies to both conditions).
- Empiric antimicrobial therapy in patients with sepsis/septic shock is recommended, including at least two classes of broad-spectrum antibiotics to target a broader range of microorganisms or suspected pathogens, including bacteria, potential fungi, and viruses (strong recommendation, moderate quality evidence).
- Adjustment, in the form of tapering of empirical antibiotic therapy, should be made if the pathogen and its susceptibility are identified and/or if there is clinical improvement (best practice recommendation - BPS).
- Prophylactic use of antibacterial drugs in patients with severe inflammatory diseases of non-infectious origin (severe pancreatitis, thermal skin burns, etc.) is not recommended (best practice recommendation - BPS).
- Antimicrobial dosing strategy should be based on generally accepted pharmacokinetic/pharmacodynamic principles, as well as taking into account organ function and certain characteristics of antimicrobials in patients with sepsis or septic shock (best practice recommendation - BPS).
- In the case of septic shock, initial empiric combination antibiotic therapy (using at least two classes of antibiotics) should be directed at the most likely pathogen (weak recommendation, low-quality evidence).
- Combination antibiotic therapy for neutropenic fever/bacteremia is not recommended in routine clinical practice (strong recommendation, moderate quality of evidence).
- The use of combination antibiotic therapy is not recommended for the chronic treatment of most other serious infections, including bacteremia and sepsis without signs of shock (weak recommendation, low-quality evidence).
- The use of combination antibiotic therapy is not recommended for the routine treatment of neutropenic fever/bacteremia (strong recommendation, moderate quality of evidence).
- When combination antimicrobial therapy is initially used to treat septic shock, it is recommended that it be de-escalated or discontinued within the first few days in response to clinical improvement and/or evidence of resolution of the infection. This applies to both etiotropic (positive culture of the pathogen) and empirical (in case of negative bacteriological study) antibiotic therapy (best practice recommendation - BPS).
- The adequate duration of antibiotic therapy for most infections associated with sepsis/septic shock is 7–10 days (weak recommendation, low-quality evidence).
- Longer use of antibacterial drugs may be justified in patients with a slow clinical response to therapy; bacteremia caused by Staphylococcus aureus; some fungal and viral infections, as well as in patients with neutropenia (weak recommendation, low quality of evidence).
- In certain categories of patients, shorter courses of antibiotic therapy are possible, for example, in patients with a rapid clinical response, as well as after adequate sanitation of the source of infection in the case of abdominal / urinary sepsis or in uncomplicated pyelonephritis (weak recommendation, low quality of evidence).
- Daily assessment of the ability to de-escalate antimicrobial therapy in patients with sepsis/septic shock is recommended (best practice guidelines - BPS).
- Procalcitonin levels can be used to assess the duration of antimicrobial therapy in patients with sepsis (weak recommendation, low-quality evidence).
- Procalcitonin levels can be used to predict discontinuation of empirical antibiotic therapy in patients who initially presented with symptoms of sepsis, but no evidence was found for localized infection (weak recommendation, low-quality evidence).
E. Sanitation of the source of infection
- It is recommended that in patients with sepsis/septic shock, the specific anatomical source of infection be identified and treated and that any necessary management of that source be undertaken as soon as the diagnosis is established (Best Practice Guidelines - BPS).
- It is recommended that any intravascular devices that may be a possible cause of sepsis/septic shock be immediately removed, but only after another device has been placed (Best Practice Guidelines - BPS).
F. Infusion therapy
- It is recommended that fluid therapy be used as long as necessary in terms of basic hemodynamic parameters and their improvement over time (best practice guidelines - BPS).
- The choice of fluid therapy should be crystalloid solutions, both initially in the treatment of sepsis/septic shock and subsequently for intravascular fluid resuscitation (strong recommendation, moderate quality of evidence).
- It is possible to use other balanced crystalloid solutions or saline as fluid therapy in patients with sepsis/septic shock (weak recommendation, low-quality evidence).
- Albumin may be used as a primary addition to crystalloid fluids during fluid resuscitation in patients with sepsis/septic shock for intravascular fluid resuscitation, particularly when patients require significant amounts of crystalloid (weak recommendation, low-quality evidence).
- The use of hydroxyethyl starch (HES) for intravascular fluid volume replacement in patients with sepsis/septic shock is not recommended (strong recommendation, high-quality evidence).
- Crystalloid solutions should be used preferentially over gelatin in fluid therapy for sepsis/septic shock (weak recommendation, low-quality evidence).
G. Vasoactive drugs
- Norepinephrine is the first-line vasopressor drug of choice (strong recommendation, moderate quality of evidence).
- It is possible to add either vasopressin (up to 0.03 units/min) (weak recommendation, moderate-quality evidence) or epinephrine (weak recommendation, low-quality evidence) to norepinephrine to increase mean arterial pressure to target, as well as adding vasopressin (up to 0.03 units/min) (weak recommendation, moderate quality of evidence) to reduce the dose of norepinephrine.
- As an alternative to norepinephrine, dopamine may be recommended as a vasopressor only in certain patients (eg, patients at low risk of tachyarrhythmia and absolute/relative bradycardia) (weak recommendation, low quality of evidence).
- The use of low-dose dopamine to preserve renal function is not recommended (strong recommendation, high-quality evidence).
- The use of dobutamine is recommended when persistent tissue hypoperfusion persists despite adequate fluid resuscitation and the use of vasopressors (weak recommendation, low-quality evidence).
- All patients who require vasopressors should have arterial access (catheter) when possible and resources available (weak recommendation, very low-quality evidence).
N. Corticosteroids
- In patients with septic shock, the use of intravenous hydrocortisone is not recommended unless adequate fluid loading and vasopressor therapy are sufficient to stabilize hemodynamics. When, despite measures taken, stabilization does not occur, hydrocortisone 200 mg/day may be prescribed (weak recommendation, low-quality evidence).
I. Blood components
- In adult patients, red blood cell (RBC) transfusion is recommended only when hemoglobin levels are <70 g/L and in the absence of other aggravating conditions such as myocardial ischemia, severe hypoxemia, or acute blood loss (strong recommendation, high-quality evidence).
- The use of erythropoietin for the treatment of anemia associated with sepsis is not recommended (strong recommendation, moderate quality of evidence).
- The use of fresh frozen plasma (FFP) for the correction of coagulation abnormalities in the absence of bleeding or planned invasive procedures is not recommended (weak recommendation, very low-quality evidence).
- Prophylactic platelet transfusion is indicated when the platelet level is >10,000 mm3 (10x109/L) in the absence of obvious signs of bleeding or when the level is >20,000 mm3 (20x109/L) in patients at high risk of bleeding. A higher blood platelet level >50,000 mm3 (50 x 109/L) is acceptable during active bleeding, surgery or invasive procedures (weak recommendation, very low quality of evidence).
J. Immunoglobulins
- The use of intravenous immunoglobulin in patients with sepsis/septic shock is not recommended (weak recommendation, low-quality evidence).
K. Hemosorption
- There are no recommendations regarding hemosorption.
L. Anticoagulants
- The use of antithrombin in the treatment of sepsis/septic shock is not recommended (strong recommendation, moderate quality of evidence).
- There are no recommendations for the use of thrombomodulin or heparin in the treatment of sepsis/septic shock.
M. Artificial pulmonary ventilation (ALV)
- For sepsis-induced acute respiratory distress syndrome (ARDS) in adults, a target tidal volume of 6 ml/kg body weight (BW) is recommended versus 12 ml/kg BW (strong recommendation, high-quality evidence).
- In adults with severe ARDS due to sepsis, it is recommended to use an upper limit of plateau pressure (30 cmH2O) versus a higher plateau pressure (strong recommendation, moderate quality of evidence).
- It is recommended to use high positive end expiratory pressure (PEEP) over low positive end expiratory pressure (PEEP) in adults with moderate/severe ARDS due to sepsis (weak recommendation, moderate quality of evidence).
- In adult patients, the use of the alveolar opening maneuver is recommended for severe ARDS caused by sepsis (weak recommendation, moderate quality of evidence).
- For patients with severe ARDS caused by sepsis, the optimal position is a prone position compared to the supine position and a PaO2 / FIO2 ratio <150 mmHg. (strong recommendation, moderate quality of evidence).
- The use of high-frequency ventilation is not recommended in adults with ARDS due to sepsis (strong recommendation, moderate quality of evidence).
- There are no recommendations for the use of noninvasive mechanical ventilation in adult patients with ARDS caused by sepsis.
- It is recommended to use muscle relaxants (NMBAs) for ≤ 48 hours in adults with ARDS caused by sepsis and PaO2/FIO2 ratio <150 mmHg. (weak recommendation, moderate quality of evidence).
- Conservative fluid resuscitation is recommended in patients with established sepsis-related ARDS who do not have evidence of tissue hypoperfusion (strong recommendation, moderate quality of evidence).
- The use of ß2-agonists in the treatment of ARDS caused by sepsis in the absence of symptoms of bronchospasm is not recommended (strong recommendation, moderate quality of evidence).
- In routine practice, pulmonary artery catheter placement is not recommended in patients with ARDS due to sepsis (strong recommendation, high-quality evidence).
- It is recommended to use low versus high tidal volume in patients with respiratory failure due to sepsis but without symptoms of ARDS (weak recommendation, low-quality evidence).
- To prevent aspiration, as well as to prevent the development of ventilator-associated pneumonia in patients receiving mechanical ventilation, a supine position with the head elevated at 30 to 45 degrees is recommended (strong recommendation, low-quality evidence).
- Spontaneous breathing training is recommended for patients with sepsis who are mechanically ventilated but ready to wean (strong recommendation, high-quality evidence).
- It is recommended to use a mechanically ventilated weaning protocol in patients with respiratory failure due to sepsis who are ready to wean (strong recommendation, moderate quality of evidence).
N. Sedation and analgesia
- In mechanically ventilated patients with sepsis, it is recommended to minimize prolonged or intermittent sedation, targeting specific titration points (best practice recommendation - BPS).
A. Glucose control
- In the intensive care unit, in patients with sepsis, it is recommended to use a documented approach to monitoring blood glucose levels - in the case when the glycemia on two tests performed is > 10 mmol/l, it is recommended to start insulin injections. This approach would maintain an upper blood glucose level of ≤ 10 mmol/L rather than an upper blood glucose level of ≤ 6.1 mmol/L (strong recommendation, high-quality evidence).
- Glycemic monitoring is recommended every 1 to 2 hours until glucose levels and insulin infusion rates are stable, then every 4 hours in patients receiving insulin infusions (best practice recommendation - BPS).
- Interpretation of glucose levels from capillary blood testing should be done with caution, as such measurements may not accurately reflect the true level of glycemia in both arterial blood and plasma (best practice guideline - BPS).
- When the patient has arterial access (catheter) for glucose testing, it is recommended to use arterial blood rather than capillary blood (weak recommendation, low-quality evidence).
P. Renal replacement therapy
- In patients with sepsis and/or acute kidney injury, both long-acting and intermittent renal replacement therapy (RRT) are options (weak recommendation, moderate-quality evidence).
- In patients with sepsis and haemodynamic instability, the use of long-acting renal replacement therapy is recommended to control fluid balance (weak recommendation, very low-quality evidence).
- In patients with sepsis and/or acute kidney injury, when there are no other indications for dialysis other than high creatinine and oliguria, the use of renal replacement therapy is not recommended (weak recommendation, low quality of evidence).
Q. Bicarbonate infusion
- The use of sodium bicarbonate is not recommended to improve hemodynamics or reduce the need for vasopressors in patients with lactic acidosis, pH ≥ 7.15 caused by hypoperfusion (weak recommendation, moderate quality of evidence).
R. Prevention of venous thromboembolism (VTE)
- For the prevention of venous thromboembolic complications (VTEC), the use of both unfractionated heparins (UFH) and low molecular weight herparins (LMWH) is recommended, provided there are no contraindications to their use (strong recommendation, moderate quality of evidence).
- For the prevention of VTEC, the greatest preference is given to LMWH compared to UFH, provided there are no contraindications to the use of the former (strong recommendation, moderate quality of evidence).
- In situations where possible, a combination of drug prophylaxis of VTE with mechanical (physical) prophylaxis is recommended (weak recommendation, low quality of evidence).
- The use of mechanical prophylaxis of VTE is recommended when medicinal (pharmacological) is contraindicated (weak recommendation, low quality of evidence).
S. Prevention of steroid ulcers
- Steroid ulcer prophylaxis is recommended for patients with sepsis/septic shock at high risk of gastrointestinal bleeding (strong recommendation, low-quality evidence).
- The use of both proton pump antagonists (PPIs) and histamine H2 receptor antagonists (H2RAs) is recommended for the prevention of steroid ulcers (weak recommendation, low-quality evidence).
- Steroid ulcer prophylaxis is not recommended in the absence of risk factors for gastrointestinal bleeding (BPS).
T. Nutrition
- It is not recommended to use parenteral nutrition alone or in combination with enteral nutrition in patients with sepsis/septic shock who can be fed enterally (strong recommendation, moderate quality of evidence).
- It is not recommended to use parenteral nutrition alone or in combination with enteral nutrition (but rather start an intravenous glucose infusion as soon as possible and try to establish enteral nutrition) for the first 7 days in severely ill patients with sepsis/septic shock for whom enteral nutrition has previously been impossible (strong). recommendation, moderate quality of evidence).
- It is recommended to initiate earlier enteral nutrition rather than intravenous glucose infusion alone in severely ill patients with sepsis/septic shock who can be fed enterally (weak recommendation, low-quality evidence).
- It is recommended to use either early low-calorie or early total enteral nutrition in severely ill patients with sepsis/septic shock; If a low-calorie diet is started, the diet should be modified according to the patient's tolerance (weak recommendation, moderate quality of evidence).
- The use of omega-3 fatty acids as an immune supplement in severely ill patients with sepsis/septic shock is not recommended (strong recommendation, low-quality evidence).
- Routine measurement of gastric residual volume in severely ill patients with sepsis/septic shock is not recommended (weak recommendation, low-quality evidence). However, measurement of gastric residual volume in patients with malabsorption or at high risk of aspiration is acceptable (weak recommendation, very low quality of evidence). Note: This recommendation applies to non-surgical severe patients with sepsis/septic shock.
- It is recommended to use prokinetic agents in severely ill patients with sepsis/septic shock and malabsorption (weak recommendation, low-quality evidence).
- It is recommended to place an intrastinal (post-pyloric) feeding tube in severely ill patients with sepsis/septic shock with malabsorption or a high risk of aspiration (weak recommendation, low-quality evidence).
- The use of intravenous selenium in the treatment of sepsis and septic shock is not recommended (strong recommendation, moderate quality of evidence).
- The use of arginine in the treatment of sepsis and septic shock is not recommended (weak recommendation, low quality of evidence).
- The use of glutamine in the treatment of sepsis and septic shock is not recommended (strong recommendation, moderate quality of evidence).
- There are no recommendations for the use of carnitine in the treatment of sepsis and septic shock.
Prevention
The following measures will help prevent blood poisoning:
- proper use of antibiotics;
- compliance with basic hygiene rules;
- timely treatment of purulent processes;
- compliance with aseptic conditions during medical procedures;
- immunization of people at risk.
Purulent-septic diseases are much easier to prevent than to cure, so patients need not only to take individual preventive measures, but also to monitor how the procedure is going in the medical office. Following these simple measures will help prevent the development of the disease.
How to diagnose sepsis?
To accurately diagnose sepsis, signs and symptoms must be confirmed by testing. First, you should take a blood test from two places; sepsis is indicated by blood clotting disorders, improper functioning of the kidneys and liver, and electrolyte imbalance. In addition to a blood test, when the signs do not allow you to say for sure that it is sepsis , it is necessary to check the urine for bacteria, especially with a urinary tract infection.
sepsis diagnosis
An infection can get into an open wound, then you need to take fluid from it for examination in order to prescribe the right antibiotic.
If you have a severe cough, sputum samples should be taken to find out the name of the microbe causing the infection.