Pharmacodynamics
Pimecrolimus is a derivative of the macrolactam ascomycin and has an anti-inflammatory effect. Pimecrolimus selectively inhibits the production and release of cytokines and inflammatory mediators from T lymphocytes and mast cells.
Pimecrolimus specifically binds to the cytosolic receptor macrophilin-12 and inhibits the calcium-dependent phosphatase calcineurin. Inhibition of calcineurin leads to suppression of T-lymphocyte proliferation and prevents the transcription and production of early cytokines in T-helper types 1 and 2, such as IL-2, interferon-γ, IL-4, IL-5, IL-10, tumor necrosis factor (TNFα) and granulocyte-macrophage colony-stimulating factor. Pimecrolimus and tacrolimus equally suppress the secondary immune response in isolated skin T helper cell colonies obtained from patients with atopic dermatitis.
In addition, in vitro, after interaction with the antigen/IgE complex, pimecrolimus prevents the antigen/IgE-mediated release of cytokines and inflammatory mediators from mast cells. Pimecrolimus does not affect the growth of keratinocytes, fibroblasts and endothelial cells and, unlike corticosteroids, has a selective effect on cells of the immune system and does not cause dysfunction, viability, differentiation processes, maturation of Langerhans cells in mice and dendritic cells of monocytic origin in humans. The drug does not affect the differentiation of “naive” T-lymphocytes into T-effector cells under the influence of Langerhans cells and dendritic cells, which is one of the main mechanisms of a specific immune response.
In experimental models of skin inflammation, the high anti-inflammatory activity of pimecrolimus was demonstrated after its local and systemic application. When applied topically in experimental models of allergic contact dermatitis (ACD), pimecrolimus is comparable in effectiveness to highly active corticosteroids: clobetasol-17-propionate and fluticasone, inhibits the inflammatory response in response to skin irritants, without causing changes in skin consistency and atrophy.
In addition, when administered topically and orally, pimecrolimus effectively reduces skin inflammation, itching, and the severity of histopathological changes in experimental models of ACD. When applied topically, the penetration of tacrolimus and pimecrolimus into the skin is equally good. However, the ability of pimecrolimus to penetrate the skin is less than that of tacrolimus and GCS. Thus, pimecrolimus has a selective effect on the skin.
The unique mechanism of action of pimecrolimus is the combination of a selective anti-inflammatory effect on the skin with a slight effect on the systemic immune response.
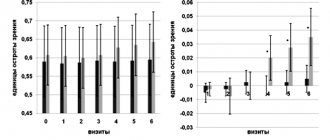
When used for 6 weeks in children aged 3 months to 17 years, pimecrolimus effectively reduces itching and skin inflammation (erythema, infiltration, excoriation and lichenification). With long-term use for 12 months, pimecrolimus effectively reduces the incidence of sudden exacerbations of ACD without causing atrophy, irritation or increased sensitivity of the skin, and without phototoxic or photosensitizing effects.
Pharmacological properties of the drug Elidel
Pimecrolimus is a derivative of the macrolactam ascomycin. Selectively inhibits the production and release of cytokines and mediators from T lymphocytes and mast cells. Has anti-inflammatory properties. Pimecrolimus binds highly specifically to macrophilin-12 and inhibits the calcium-dependent phosphatase calcineurin. As a result, by blocking the transcription of early cytokines, pimecrolimus suppresses the activation of T lymphocytes. In particular, in nanomolar concentrations, pimecrolimus inhibits the synthesis of interleukin-2, interferon gamma (Th1 type), interleukin-4 and interleukin-10 (Th2 type) in human T lymphocytes. In addition, in vitro after interaction with the antigen/IgE-pimecrolimus complex, it prevents the antigen/IgE-mediated release of cytokines and inflammatory mediators from mast cells. Pimecrolimus does not affect the growth of keratinocytes, fibroblasts and endothelial cells. The drug combines high anti-inflammatory activity and a slight effect on systemic immune responses. When pimecrolimus is applied topically, its concentration in the blood is very low, so it is impossible to determine metabolic parameters. In vitro in human skin .
Pharmacokinetics
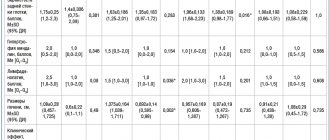
Adults. The concentration of pimecrolimus in the blood was determined in 12 adult patients with atopic dermatitis (eczema) affecting 15–59% of the body surface area, treated with Elidel cream 2 times a day for 3 weeks. In 77.5% of observations, the concentration of pimecrolimus in the blood was below 0.5 ng/ml (minimum detectable concentration), and in 99.8% it was below 1 ng/ml. Cmax of pimecrolimus in the blood, recorded in 1 patient, was 1.4 ng/ml.
In 98% of 40 adult patients with initial lesions of 14–62% of the body surface area, after 1 year of treatment with Elidel cream, pimecrolimus blood concentrations remained low and in most cases were below the minimum detectable concentration.
A Cmax value of 0.8 ng/ml was recorded after 6 weeks of treatment in only 2 patients. None of the patients showed an increase in concentration over 12 months of treatment. During a 3-week period of treatment with Elidel cream twice daily in 13 adult patients with hand dermatitis (using the cream on the palms and dorsum of the hands and bandaging at night), the maximum recorded blood concentration of pimecrolimus was 0.91 ng/ml.
In 8 patients with pimecrolimus blood levels above the minimum detectable concentration, the AUC value was 2.5–11.4 ng/ml.
Children. Pharmacokinetic studies of pimecrolimus were conducted in 58 children aged 3 months to 14 years with atopic dermatitis (eczema) affecting 10–92% of the body surface area, treated with Elidel cream 2 times a day for 3 weeks. Five children received treatment for 1 year as needed.
Pimecrolimus blood concentrations were consistently low, regardless of the area of skin lesions and duration of therapy, and were in the same range as in adult patients receiving Elidel cream therapy at the same doses. In 97% of cases, pimecrolimus blood concentrations were below 2 ng/ml, and in 60% they were below 0.5 ng/ml (minimum detectable concentration). The Cmax of pimecrolimus recorded in 2 patients aged 8 months and 14 years was 2 ng/ml.
Among the youngest children (from 3 to 23 months), the Cmax of pimecrolimus was 2.6 ng/ml and was recorded in 1 patient.
In 5 children treated with Elidel cream for 1 year, pimecrolimus concentrations were at consistently low levels. The maximum value recorded in 1 child was 1.94 ng/ml. Throughout the entire treatment period, an increase in drug concentrations was not observed in any of the patients.
In 8 children aged 2 to 14 years with blood levels of pimecrolimus above the minimum detectable concentration when measured three times, the AUC value ranged from 5.4–18.8 ng/ml. AUC values in patients with skin lesions less than or greater than 40% were comparable.
In in vitro studies, the binding of pimecrolimus to plasma proteins (mainly various lipoproteins) was 99.6%.
Since the concentrations of pimecrolimus in the blood are very low when applied topically, determination of metabolic parameters is not possible.
Pharmacokinetics in special clinical situations
Atopic dermatitis (eczema) is rarely observed in patients aged 65 years and older. The number of patients of this age in clinical studies of Elidel 15% cream was insufficient to detect any difference in treatment effectiveness compared with younger patients.
Dosing recommendations for infants (3–23 months), children (2–11 years), and adolescents (12–17 years) are the same as for adult patients.
Contraindications
hypersensitivity to timecrolimus or any components of the drug;
children under 3 months of age (the safety and effectiveness of Elidel cream in children under 3 months of age has not been studied);
the presence of acute viral, bacterial or fungal skin infections.
Carefully:
patients with Netherton's syndrome (no safety data available) - there may be a risk of increased systemic absorption of the drug;
severe forms of inflammation or skin damage, incl. generalized erythroderma (no data on safety of use) - there may be a risk of increased systemic absorption of the drug;
weakened immunity - because the effectiveness and safety of use have not been studied.
There are no data on the safety of long-term use of Elidel cream.
Since the effect of long-term use of the drug on the immune defense of the skin and the incidence of malignant neoplasms has not been studied, Elidel cream should not be applied to damaged areas of the skin with possible malignancy or dysplastic changes.
In case of bacterial or fungal infection of the skin, the use of Elidel cream on the affected areas is possible only after the infection has been cured.
Elidel Rosacea Cream
In 2021, rosacea disease is gaining momentum in popularity and becoming a pressing problem in the field of dermatology. This is a chronic disease expressed in the form of rosacea on the face. It usually occurs in people in the age group of 30 to 50 years. However, women experience rosacea three times more often than men. The disease progresses especially in people with fair skin.
Causes of the disease
The leading role in the occurrence of rosacea is assigned to:
- Vascular disorders;
- Pathologies of the gastrointestinal tract;
- Dysfunction of the endocrine system;
- Psychosomatic and immune disorders.
With rosacea, specific redness of the skin, papules, and pustules appear. The severe course of the disease is manifested by the presence of nodes. In patients, the level of large globular plasma proteins of class: A, M and G increases. Deposits of immunoglobulins are detected on the basement membrane using an immunofluorescent assay. When studying cellular immunity, a significant increase in the absolute number of “total” and “active” cells and a decrease in the number of T-suppressors was revealed.
The main factors that provoke the appearance of rosacea include:
- Climatic conditions (exposure to sunlight, heat, cold, humidity, sharp wind);
- Negative feelings (anger, fear, rage, stress);
- Nutrition (excessive consumption of hot and spicy foods, foods made from milk, chocolate, soy sauce, coffee, alcohol);
- Circumstances (bathhouse, working outside in bad weather conditions, heavy physical activity, lifting and carrying heavy objects);
- Certain medications (vasodilators, nicotinic acid) and cosmetics (cleansing gels and lotions containing alcohol, perfumed soaps).
Self-care for your skin
Knowing the factors behind the appearance of rosacea, you need to fight rosacea at home. The first rule of care: avoid overheating. To do this, you should avoid staying in the summer sun from 11 a.m. to 4 p.m. You also need to protect your facial skin from wind and cold. In winter, it is better to apply a special cream before going outside. But in the summer you shouldn’t neglect protection. You should apply a sunscreen that contains zinc oxide or titanium dioxide. And also the protection factor should be at least 30. You should avoid scrubs or facial massage. Use only decorative cosmetics, with minimal application to the skin. Try to avoid getting hairspray on inflamed areas.
Choice of medicine
But even if you follow all the rules, you cannot rule out turning to specialists. When choosing a drug for rosacea, you need to consider:
- nature and stage of development;
- severity of rosacea disease;
- age restrictions;
- area and location of the lesion.
The choice of dosage form of the drug plays an important role in rosacea. It determines the rationality of the prescription to protect the affected areas of the skin and the development of possible complications. The preferred dosage form for bodies with thin skin is cream. The oil-in-water composition is concentrated in the stratum corneum of the epidermis. It allows you to gently eliminate the inflammatory process, is quickly absorbed, and does not leave an oily sheen.
In 2021, doctors recommend prescribing a drug called Elidel for the treatment of rosacea. Its cost in Moscow pharmacies ranges from 946 to 2000 rubles. You can order the drug via the Internet - this way the price will be lower. This medicine is intended to be applied to the surface of the skin. Elidel for rosacea has an unmistakable and rapid effect.
The instructions recommend starting treatment at the first symptoms. This is due to the elimination of the formation of the disease in a deeper form. Elidel is applied in a thin layer, gently rubbing into the skin until completely absorbed. This procedure should be carried out twice a day until the problem disappears completely. But if after six weeks of applying the product the severity of symptoms continues, you should see a doctor. Repeated examination of the patient is required to confirm the presence of dermatitis or rosacea.
Elidel has a wide range
The instructions do not mention rosacea, but it is possible to use the product for this disease. The medicine has an antiphlogistic effect due to the active substance in the composition: pimecrolimus. It uniquely blocks the transcription of early cytokines, suppressing the activation of T lymphocytes. The substance helps with skin inflammation, but the effect on the systemic immune response is negligible. The uniqueness of the drug mechanism lies in the combination of anti-inflammatory activity that is selective for the skin. But only one that has a low ability to induce systemic immune responses.
Elidel drug allows to achieve clinical remission in 83% of patients with rosacea. And with further observation of two years, the result is maintained in 59% of people. Resumption of the disease occurs 1.5 times less than with metronidazole. Treatment with Elidel promotes:
- improvement of the morphological structure of the skin in the form of a more uniform stratum corneum;
- an increase in the thickness of the epidermis with a clear line of the epidermal-dermal junction;
- uniform distribution of hyperechoic zones and reduction of their area
This is confirmed by visualization of ultrastructural changes during ultrasonic dermascanning. As well as indicators of the thickness of the epidermis and the density of the dermis during a morphometric study of the skin. This remedy is effective for facial skin in the treatment of mild to moderate inflammatory rosacea. It reduces the intensity of erythema by 8.6%, the severity of the process - by 24.6%. And this is just after a week of application to the skin. After 7-12 weeks, the number of papulopustular elements will decrease by 80%.
Restrictions
However, the product has a number of contraindications. The first thing you should pay attention to is age. The use of Elidel in people under three months of age has not been studied. Do not apply the product if you have an acute viral, bacterial or fungal skin infection. It is also impossible to exclude an increased reaction to the substances of the Elidel drug to avoid allergies.
You should be careful with:
- Weakened immunity (neither efficacy nor safety has been studied);
- Severe inflammation or skin lesions (no safety data);
- The presence of Netherton's syndrome in patients (there is a possible risk of increased systemic absorption of the drug Elidel);
Unfortunately, side effects from the drug cannot be ruled out.
For example, a slight reaction in the form of burning, redness or itching may occur in the area of application. These symptoms occur early in treatment and should be short-lived. Otherwise, you should consult a doctor. In rare cases, studies have revealed suppuration and worsening of the disease. And on the part of the immune system - a rapid allergic reaction that poses a danger to life. A rash, hives and swelling may also occur. A change in skin color is possible. When using Elidel, the development of malignant neoplasms was extremely rarely observed. However, a cause-and-effect relationship could not be determined.
Women pay special attention when applying the drug during pregnancy and breastfeeding. This is not surprising; they worry about the health of their newborn children. However, no data were found during the study of Elidel on the development of the embryo or the course of labor. The low degree of absorption of the substance contained in the drug reduces the risk to a minimum. But there have been no studies following topical use during breastfeeding. Therefore, it doesn't hurt to be careful.
However, according to reviews, Elidel rarely leads to adverse reactions. Situations with drug withdrawal are minimal. But for safety it is better to follow the rules:
- If the product gets into your eyes, wash with water.
- When using the drug, it is necessary to reduce artificial insolation of the dermis. Doctors advise excluding UV radiation.
- There is no need to use the treatment under tight bandages.
- After application to the skin, it is necessary to treat with emollients.
- The drug should not be used by persons with hereditary or acquired immunodeficiency. Patients who use immunosuppressive drugs for treatment.
- Do not apply to areas with malignant lesions.
- The medicine contains stearyl, cetyl alcohol, and propylene glycol. The components may cause local skin reactions.
Description of the drug
Elidel can be purchased in dosages from 15 to 30 g. It is sold in sealed aluminum tubes with a cap. There is a convenient ledge for opening. The product is a dense snow-white mass, without foreign inclusions and a characteristic odor. Storage plays an important role. The room temperature should not exceed 25 degrees. Freezing the drug is prohibited. Compliance with storage rules ensures the desired treatment effect. The shelf life is 1 year. Once the aluminum tube is opened, it is applied to the skin for no more than 24 months. Do not use the product after the expiration date. This will not bring the desired effect, but it can also be harmful to health. Storage should be in a room without direct sunlight on the drug. Deterioration of the product is manifested in the stratification of the mass, color modification and change in odor.
As a result, Elidel cannot be a panacea for all diseases. But rosacea is included in the list of diseases in which an anti-inflammatory effect is achieved. But it is necessary to minimize the impact of factors that cause and aggravate the disease. Therefore, it is necessary to include in therapy not only drug treatment, but also preventive measures. And although this drug has been on the market since 2007, it is classified as a fundamentally new non-steroidal drug. It has an immunomodulatory and anti-inflammatory effect. It has broad prospects in external therapy. Reviews on the sites say that side effects rarely occur. The drug is easy to use. And, according to research, the best results in treating the disease were achieved with Elidel. There is rapid relief, removal of redness and healing of problem areas with rosacea. And although after visiting a consultation, doctors more often recommend this drug. The choice is up to the patient.
Use during pregnancy and breastfeeding
There are no data on the use of the drug in pregnant women. In experimental studies with local use of the drug, no direct or indirect damaging effect of Elidel cream on the course of pregnancy, the development of the embryo/fetus, the course of childbirth and the postnatal development of the offspring was not revealed. Caution should be exercised when prescribing to pregnant women. However, given the minimal absorption of pimecrolimus when administered topically, the potential risk in humans is considered negligible.
The excretion of the drug into breast milk after topical administration has not been studied in experimental models. There are no data on the content of pimecrolimus in the breast milk of lactating women.
Since many drugs are excreted in breast milk, caution should be exercised when prescribing Elidel 1% cream to nursing women. However, given the minimal systemic absorption of pimecrolimus when administered topically, the potential risk to humans is considered negligible.
Breastfeeding women should not apply Elidel 1% cream to the breast area.
The effect of Elidel cream on fertility in men and women has not been established.
Side effects
The use of Elidel cream may cause minor transient reactions at the application site, such as a feeling of warmth and/or burning. If these reactions are severe, patients should consult a doctor.
The most common reactions at the site of application of the drug were observed in 19% of patients treated with Elidel cream and in 16% of patients in the control group. These reactions mainly occurred early in treatment and were minor/moderate and short-lived.
Determination of the frequency of adverse reactions: very often (≥1/10); often (≥1/100, <1/10); sometimes (≥1/1000, <1/100); rare (≥1/10000, <1/1000); very rare (<1/10000), including isolated reports.
Very often - burning at the site of application of the cream.
Often - local reactions (irritation, itching and redness of the skin), skin infections (folliculitis).
Sometimes - suppuration, worsening of the disease, herpes simplex, dermatitis caused by the herpes simplex virus (herpetic eczema), molluscum contagiosum; local reactions such as rash, pain, paresthesia, peeling, dryness, swelling, skin papillomas, boils.
The following adverse reactions were observed during post-marketing use of the drug (frequency estimate based on the number of cases of adverse events in an unspecified population).
From the immune system: very rarely - anaphylactic reactions.
Metabolic disorders (metabolic disorders): rarely - alcohol intolerance.
From the skin and its appendages: rarely - allergic reactions (rash, urticaria, angioedema); changes in skin color (hypopigmentation, hyperpigmentation).
In most cases, facial redness, rash, burning, itching or swelling developed immediately after drinking alcohol.
When using Elidel cream, in rare cases, the development of malignant neoplasms, including skin and other types of lymphomas, and skin cancer was observed. A cause-and-effect relationship between these adverse events and the use of the drug has not been established.
Side effects of the drug Elidel
Common: burning sensation at the site of application of the cream, reactions at the site of application (irritation, rash, erythema), skin infections (folliculitis). Rarely: impetigo, deterioration of the condition, herpes simplex and herpes zoster, herpes dermatitis, Kaposi's varioliform pustulosis, molluscum contagiosum, disturbance at the application site - pain, paresthesia, peeling, dryness, swelling, skin papilloma, boil, alcohol intolerance (in most such cases after When drinking alcohol, there were sensations of blood flow, rash, itching or swelling), allergic reactions (skin rash, urticaria, angioedema) and changes in skin color (hypo- or hyperpigmentation). Very rare : anaphylactic reactions. In isolated cases, malignancies, including cutaneous and other types of lymphomas, as well as skin cancer, have been reported in patients using pimecrolimus cream, although a causal relationship has not been established.
Interaction
The potential interaction of Elidel cream with other drugs has not been studied. Given that the systemic absorption of pimecrolimus is very low, any interaction of Elidel cream with drugs for systemic use is unlikely.
When using Elidel cream in children aged 2 years and older, the drug did not affect the effectiveness of vaccination.
It is not recommended to apply cream to the area where the vaccine was administered until local manifestations of the post-vaccination reaction have completely disappeared.
Incompatibility. Since compatibility studies have not been conducted, it is not recommended to use the drug in combination with other topical agents.
Directions for use and doses
Externally.
Treatment should begin at the first manifestations of the disease to prevent its sudden exacerbation.
The cream is applied in a thin layer to the affected surface 2 times a day and gently rubbed until completely absorbed.
The cream can be applied to the skin of any part of the body, including the head, face, neck, as well as to diaper rash areas. Elidel cream should be used 2 times a day until the symptoms of the disease completely disappear. If the severity of symptoms persists, after 6 weeks of using the drug, it is necessary to re-examine the patient to confirm the diagnosis of atopic dermatitis. After cessation of treatment, in order to avoid subsequent exacerbations, at the first signs of relapse of atopic dermatitis, therapy should be resumed. Emollients can be applied immediately after applying Elidel 1% cream. However, after water procedures, emollients should be used before applying Elidel cream.
Given the very low systemic absorption of pimecrolimus, there are no restrictions on the total daily dose of the drug applied, the area of skin surface treated, or the duration of treatment. If Elidel cream gets into your eyes or mucous membranes (oral or nasal cavity), you should immediately remove the cream and rinse your eyes and mucous membranes with running water.
special instructions
When treated with topical calcineurin inhibitors, including Elidel, the development of malignant neoplasms (for example, skin tumors and lymphomas) has been observed in rare cases. A cause-and-effect relationship between these adverse events and the use of the drug has not been established.
In clinical studies when using Elidel cream, 0.9% of patients (14 out of 1544) experienced the development of lymphadenopathy. Typically, lymphadenopathy was caused by infectious diseases and disappeared after a course of appropriate antibiotic therapy. In all patients, it was either possible to identify the cause of the development of lymphadenopathy, or the disappearance of this undesirable phenomenon was noted. In patients receiving treatment with Elidel, if lymphadenopathy develops, it is necessary to establish the etiology of the process and monitor patients until this adverse event completely disappears. If the etiology of lymphadenopathy is unknown or if the patient has acute mononuclear inflammation, the drug should be discontinued.
When treated with Elidel cream, patients are advised to reduce artificial or natural insolation of the skin to a minimum or completely eliminate UV irradiation. The possible effect of using the drug on skin lesions caused by UV radiation is unknown.
Influence on the ability to drive vehicles and operate machinery. The effect of using Elidel cream on the ability to drive vehicles or operate machinery has not been established.
Special instructions for the use of Elidel
Should not be applied to skin affected by acute viral infection. In case of bacterial or fungal skin infection, the cream can be used after the infection has been cured. If the infection process does not decrease, the use of the cream should be discontinued until the symptoms of the infection are relieved. Since the effect of Elidel 1% cream upon long-term use on local immunity and on the manifestations of malignant skin neoplasms is not known, it should not be used in cases of potentially malignant skin neoplasms or the possibility of such diseases. Although a causal relationship has not been established, there have been rare cases of skin malignancies and lymphoma in patients treated with topical calcineurin inhibitors, including Elidel 1% cream. This medicinal product is not recommended for patients with Netherton's syndrome or generalized erythroderma, where there is a risk of increased absorption, since the safety of Elidel 1% cream in patients with these diseases has not been established. The safety and effectiveness of Elidel 1% cream in patients with immunodeficiency have also not been studied, therefore the use of the drug in this group of patients is not recommended. In clinical studies of Elidel 1% cream, 0.9% of cases of lymphadenopathy were noted. Typically, they were associated with infections and disappeared with appropriate antibiotic therapy (most of them had a known etiology or disappeared on their own). Therefore, when lymphadenopathy appears in patients who used Elidel 1% cream, it is necessary to clarify the etiology of this process. If the etiology of lymphadenopathy is unclear or if acute infectious mononucleosis occurs, treatment with the drug should be discontinued. It is necessary to monitor the dynamics of patients with symptoms of emerging lymphadenopathy to monitor its cure. During treatment with Elidel 1% cream, it is advisable for patients to limit exposure to natural or artificial sunlight as much as possible or avoid it altogether, even when the cream is not applied to the affected areas of the skin. The potential effect of Elidel 1% cream on affected skin that is exposed to ultraviolet radiation is not known. Cases of atopic dermatitis (eczema) are rare in patients aged 65 years and older. Clinical studies studying Elidel 1% cream did not include a sufficient number of patients in this age category to determine whether their response to the drug differs from that of younger patients. The use of the cream may cause minor transient reactions at the site of application, such as a sensation of warmth and/or burning. If these reactions are severe, patients should consult a doctor. The cream should not be applied to mucous membranes. If the drug accidentally gets on the mucous membrane or in the eyes, rinse them immediately with water. During pregnancy and breastfeeding. There is no data on the use of Elidel cream during pregnancy. Caution should be exercised when prescribing Elidel 1% cream during this period. It is unknown whether pimecrolimus passes into breast milk, so caution should be exercised when prescribing Elidel 1% cream during breastfeeding. During breastfeeding, mothers should not apply 1% Elidel cream to the breast area. Effect on the ability to drive vehicles and operate machinery: not established.