Among heart diseases, endocarditis is one of the most insidious. Under the influence of various infections (there are about 130 causative agents of this disease), the inner lining of the heart becomes inflamed. The danger is that the symptoms of infective endocarditis do not appear immediately, so patients do not always seek help in a timely manner. Also, the disease is not easy to diagnose, which is why treatment may be started later than expected. That is why cardiologists recommend regular examinations in medical centers equipped with modern equipment that has extensive research capabilities.
What is endocarditis
Symptoms of the disease occur in people of different ages, including children diagnosed with “congenital heart defects” (tetralogy of Fallot, single ventricle defects, etc.). It can be provoked by:
- mitral valve prolapse;
- hypertrophic cardiomyopathy;
- surgery on heart valves;
- cardiac septal defects;
- coronary heart disease (especially after surgery).
The disease is primarily infectious. Inflammation caused by microorganisms affects not only the endocardium itself - the internal tissues of the heart muscle - but also the heart valves and nearby vessels. Often the infection penetrates the liver, kidneys, and spleen.
Most often, pathology becomes a consequence of other diseases. The prerequisites for the occurrence of infective endocarditis is bacteriological infection of the body under various conditions. The infection also affects the heart when its valves are injured due to the installation of prostheses and pacemakers, on the surface of which microorganisms can develop. There are atherosclerotic forms caused by dystrophic changes in cardiac tissue, and rheumatic forms - due to rheumatism of the heart valves.
INFECTIOUS ENDOCARDITIS: diagnosis, clinical course, treatment
Infective endocarditis (IE) is a serious disease with a high mortality rate. Without treatment, the mortality rate for IE is 100%. In recent years, there has been a significant increase in the number of patients with endocarditis in our country and abroad. According to various authors, today the incidence has increased in the elderly and senile, as well as among people under 30 years of age who use intravenous drugs [1, 2].
It is known that IE is a disease of an infectious nature with the primary localization of the pathogen on the heart valves and parietal endocardium, occurring with manifestations of systemic infection, vascular complications and an immune reaction [3, 4, 5].
Traditionally, the development of IE is associated with the presence of “intracardiac” risk factors, which include congenital and acquired heart defects, the presence of prosthetic valves, valve prolapse and other anomalies [6]. In recent years, patients with focal infection, as well as people who have had invasive research methods, including the installation of a subclavian catheter, have been classified as high-risk individuals [7]. A special risk group consists of drug addicts who practice intravenous drug administration, in whom IE occurs with damage to intact heart valves.
This paper summarizes the experience of diagnosing and managing patients with IE on the basis of the general therapeutic department of the Alexandrovskaya Hospital in St. Petersburg for the period 1998–2003. Diagnosis of the disease was carried out in accordance with Duke criteria [8]. The diagnosis of IE was assessed as reliable if two main criteria were present, namely:
- when a pathogen typical for IE is isolated from a patient’s blood culture;
- when determining echocardiographic signs of endocardial damage - mobile vegetations on the heart valves, abscesses in the area of the valve prosthesis; formation of intracardiac fistulas, etc., in combination with three and/or five auxiliary criteria, which included vascular complications (embolism of large arteries, septic pulmonary infarctions, intracranial hemorrhages, etc.), immunological phenomena (glomerulonephritis, Osler’s nodes, hemorrhagic vasculitis and etc.), as well as febrile fever, hepato-splenomegaly and other manifestations of systemic infection.
We examined 105 patients with IE, of which in 80 people aged 18 to 30 years (first group), the main risk factor for the disease was injection drug addiction.
In the second group of patients (25 people), the main predisposing factors for the development of IE were congenital and acquired heart defects, as well as prosthetic valves.
In people of the older age group, an additional risk factor was degenerative-dystrophic changes in the heart valves.
The relationship between the nature of heart valve damage and risk factors for IE is presented in Table 1.
According to an echocardiographic study, 100% of patients in the first group had mobile vegetations on the leaflets of the tricuspid valve (TV), which was accompanied by the formation of its insufficiency of degrees I-III.
In the second group of patients with IE, there was damage to the left chambers of the heart with the formation of vegetations on the leaflets of the aortic and mitral valves. Isolated damage to the mitral valve was observed in two people with rheumatic heart disease (mitral stenosis), in one patient with a congenital ventricular septal defect, and in a single case of an obstructive form of hypertrophic cardiomyopathy.
Among elderly and senile people, nine people (36%) had isolated damage to the aortic valve in the absence of signs of aortic stenosis. Along with this, in five patients (20%) aged from 72 to 87 years, IE developed against the background of an aortic defect of atherosclerotic origin, and in all five, combined damage to the aortic and mitral valves was detected. Degenerative-dystrophic changes in other heart valves were detected in 100% of patients in the older age group.
The formation of vegetations on the aortic valve leaflets was observed in two patients with the tertiary form of syphilis against the background of an existing aortic defect associated with a specific process in the aorta.
In two cases, we observed the development of endocarditis of prosthetic valves.
When comparing the results of blood cultures in two groups of patients, significant differences were determined both in the frequency of microbial flora isolation and in the species composition of endocarditis pathogens. According to our data, the causative agent of IE in drug addicted patients in 71.3% of cases (57 people) was Staphylococcus aureus, while in the second group, along with coccal flora, gram-negative microorganisms were more often found (28%). Negative blood culture results were observed significantly less often in the first than in the second group of patients with IE: 18.7% and 56%, respectively. Data regarding the etiological structure of IE in the studied groups of patients are presented in Table 2.
Clinical characteristics and features of the course of IE
The clinical course and nature of complications of infective endocarditis largely depend on the localization of valve vegetations - in the right or left chambers of the heart, as well as the degree of virulence of the causative agent of the disease.
The course of IE in drug addicted patients was particularly severe and polysyndromic. The reason for hospitalization in most patients was acute complications of the underlying disease. A significant proportion of patients were admitted to the intensive care unit of the hospital with clinical symptoms of unilateral or bilateral multifocal pneumonia, the cause of which was septic thromboembolism of the branches of the pulmonary artery (72% of patients). The course of pneumonia was accompanied by severe respiratory failure, often with the development of respiratory distress syndrome (RDS) and foci of destruction in the lungs (12%). Manifestations of secondary nephropathy, which were found in 100% of patients in the first group, were sometimes mistakenly interpreted as an exacerbation of chronic glomerulo- or pyelonephritis, urolithiasis, which served as a reason for hospitalization of these patients in the urological and nephrological departments.
In the second group of patients, the main reason for hospitalization was prolonged febrile fever in combination with anemia and hepatolienal syndrome. Along with this, in five people (20%) the reason for hospitalization was progressive heart failure.
The main clinical syndromes observed in patients with IE of the first and second groups are presented in Table 3.
According to our observations, a characteristic feature of the clinical course of IE in drug addicted patients was a high incidence of septic pulmonary embolism with the formation of multiple foci of infiltration in the lungs. In many patients, pulmonary thromboembolism was recurrent (31.3% of patients) and was often complicated by the development of destructive foci in the lungs.
The formation of vegetations in 100% of patients of the first group was accompanied by tricuspid valve insufficiency of the I-III degree with the formation of regurgitant flows. At the same time, in most patients there were no severe disturbances of central hemodynamics associated with TC dysfunction. In this group of patients, a characteristic clinical feature was the reversible nature of hemodynamic disorders during therapy. Acute heart failure with dilatation of the heart cavities and a decrease in ejection fraction to 40% or lower was observed in 28 patients (35.3%) due to the addition of acute myocarditis or against the background of concomitant damage to the heart valves.
Secondary nephropathy was one of the most common syndromes in the first group of patients with IE. Acute renal failure was observed in 16 patients, and in 10 of them it was reversible and was associated with acute disseminated intravascular coagulation syndrome, as well as acute heart failure with edema. Infectious-toxic nephropathy was recorded in 73.8% of cases and was accompanied by urinary syndrome - hematuria, proteinuria, leukocyturia - with a sufficient level of glomerular filtration.
A characteristic feature of IE in the second group was the subacute course of the disease with a long period of fever at the prehospital stage, and in the elderly and senile age the fever was subfebrile in nature with rare rises in temperature to febrile levels.
Most patients with subacute infective endocarditis (PIE) were admitted to the hospital at the stage of a developed clinical picture of the disease with clinical signs of thromboembolism of vessels in the systemic circulation. In this group of patients, the most common complications should be recognized as cerebral embolism with the development of ischemic and hemorrhagic strokes, embolism of the renal vessels with pain and hematuria, as well as the formation of acute focal changes in the myocardium associated with embolism of the coronary vessels or covering the mouths of the coronary arteries with vegetations [9].
Septic thromboembolism of cerebral vessels was often accompanied by the development of purulent meningoencephalitis with a fatal outcome. At the same time, blood cultures of 56% of patients in the second group did not show growth of microbial flora. Noteworthy is the fact that septicemia in patients with positive blood culture results in 28% of cases was caused by gram-negative microflora. In this category of patients, the source of bacteremia was foci of chronic infection in the genitourinary system, and in two patients (according to autopsy) bilateral apostematous nephritis was detected.
A significant number of patients with PIE (62%) showed signs of acute circulatory failure with congestive wheezing in the lungs, pulmonary hypertension, enlarged cardiac cavities and peripheral edema.
In this group of patients, prerenal azotemia and acute renal failure associated with the development of acute circulatory failure were observed more often than in the first group.
Acute diffuse myocarditis, typical manifestations of which were various rhythm disturbances, was diagnosed in 27% of patients in the second group.
Anemia with a decrease in hemoglobin level to 80 g/l or less was detected in 100% of patients in the second group. A significant increase in ESR (more than 45 mm/h) was observed in 85.8% of patients with subacute IE.
Skin changes in the form of hemorrhagic rashes, Henoch-Schönlein purpura, as well as other manifestations of immune inflammation in both groups of patients were uncommon - 6.3 and 4% in the first and second groups, respectively.
Treatment of patients with IE
Conservative therapy of patients with IE was carried out using broad-spectrum antibiotics in combination with detoxification, anticoagulant and metabolic therapy. As part of antibacterial therapy, patients received cephalosporins of III-IV generations in combination with aminoglycosides and metronidazole. From the group of cephalosporins, the following were prescribed: ceftriaxone (Longacef) 2 g per day intravenously (IV), or cefotaxime (Talcef) 2 g per day IV, or cefepime (Maxipim) 2 g per day IV in combination with aminoglycosides ( amikacin in a daily dose of 1.5 g intravenously) and metronidazole 1.5-2 g per day intravenously. If such therapy was ineffective or there were contraindications to the above drugs, antibiotics of the lincosamine group were used: clindamycin 1.2 g per day IV or lincomycin 3 g per day IV in combination with fluoroquinolones (ciprofloxacin 400 mg per day i.v. /V). In the intensive care unit, therapy was carried out for five to seven days with imipinem (thienam) at a dose of 2-4 g per day intravenously or rifampicin at a daily dose of 0.45-0.6 g intravenously. The average duration of antibiotic therapy in the study group of patients was 28 + 3.5 days.
Detoxification therapy included intravenous infusions of rheopolyglucin, hemodez, polarizing mixtures in combination with loop diuretics. The volume of administered fluid averaged 2-2.5 liters per day. During the entire period of infusion therapy, the functional state of the kidneys, electrolyte composition of the blood, and daily diuresis were monitored. In the intensive care unit, CVP monitoring was carried out in all patients. Infusion therapy was carried out throughout the entire acute period of the disease until the manifestations of intoxication syndrome were relieved. The average course duration was 22 + 4.5 days.
The development of pulmonary embolism, especially in combination with signs of acute disseminated intravascular coagulation syndrome in the hypercoagulable stage, served as the basis for prescribing anticoagulant therapy. The initial dose of heparin was 10 thousand units intravenously, in a stream, then - 1000 units per hour intravenously, drip with a transition to subcutaneous administration up to 30 thousand units per day. Heparin was administered under the control of coagulogram parameters and blood clotting time. At the same time, intravenous transfusions of fresh frozen plasma were carried out at a rate of 300 ml per day with the addition of 2500–5000 units of heparin. Severe anemia (Hb less than 80 g/l, Ht ≤25) was corrected by red blood cell transfusions (five to seven doses). In the presence of hypoproteinemia, the administration of solutions of amino acids, albumin or native plasma was used. Identification of clinical and radiological signs of pulmonary edema against the background of recurrent septic pulmonary embolism served as an indication for the prescription of corticosteroids (prednisolone from 120 to 200 mg per day intravenously). Therapy with direct-acting anticoagulants in combination with cryoplasma transfusions was carried out until there was a sustained improvement in hemostasis. The criteria for normocoagulation were the level of fibrinogen in plasma 3-4 g/l, the absence of thrombocytopenia, normalization of CVV, aPTT, thrombin time, as well as negative paracoagulation tests. According to our data, relief of the manifestations of acute DIC at the hypercoagulation stage in 75% of patients was observed on the seventh to tenth day from the start of complex therapy.
Some patients developed resistance to the ongoing antibacterial therapy, which was characterized by an increase in intoxication, febrile fever, progressive anemia, as well as blood cultures of the causative agent of IE - Staphylococcus aureus - in 65% of cases. During X-ray examination of this category of patients, foci of destruction of lung tissue were detected with a high frequency, and in three patients there was purulent effusion in the pleural cavity.
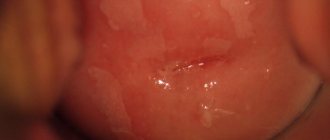
Long-term use of broad-spectrum antibiotics in 70.3% of patients (38 people) was accompanied by the development of side effects of antibacterial therapy. Candidiasis of the oral cavity, pharynx, esophagus, as well as intestinal dysbiosis of stage III-IV was detected in 36 patients (66.7%). The use of antibiotics with hepatotoxic properties (cephalosporins, lincosamines, metronidazole) in two patients (3.7%) with chronic hepatitis C and B led to the progression of liver failure, which was accompanied by high fermentemia (ALT 1500 IU, AST 1000 IU) and jaundice.
The development of congestive heart failure with the appearance of acrocyanosis, moist rales in the basal parts of the lungs, peripheral edema in combination with cardiomegaly and a drop in ejection fraction to 50-45% was observed in five patients (9.3%) against the background of massive infusion therapy.
Long-term anticoagulant therapy in 20.4% (11 people) of observations was accompanied by an increase in plasma tolerance to heparin, which was clinically expressed in the development of peripheral phlebothrombosis, while we did not observe heparin-induced thrombocytopenia in the examined group of patients.
Positive results of conservative therapy were obtained in 70.2% of patients (56 people) with TC lesions and only in 32% of patients (6 people) from the second group. The outcome of IE in both groups of patients was the formation of heart valve insufficiency.
Hospital mortality for IE in drug addicts was 29.4% (24 people), while in patients with damage to the left chambers of the heart (second group) the mortality rate was 68% (19 people).
According to autopsy data, the main causes of death in patients with IE were:
- septicopyemia with the formation of purulent foci in the liver, kidneys, spleen, brain with the development of multiple organ failure (46.2%);
- heart failure due to polyposis-ulcerative endocarditis with destruction of the heart valves, as well as acute myocarditis with dilatation of the heart cavities (39.4%);
- secondary nephropathy with the development of renal failure, pulmonary edema, cerebral edema (14.4%).
Thus, the characteristic features of IE in people with drug addiction are an acute course of the disease with damage to the right chambers of the heart and relapses of septic pulmonary embolism. The causative agent of IE in 71.3% of injection drug users is highly virulent Staphylococcus aureus. The formation of tricuspid valve insufficiency of degrees I-III has become the most common complication of IE in drug addicts. Moreover, most patients do not experience severe disturbances of central hemodynamics leading to the development of acute circulatory failure.
Subacute IE in patients with predisposing heart diseases, as well as in elderly and senile people, occurs with predominant damage to the left chambers of the heart, and monovalvular damage predominates in the older age group. The presence of concomitant pathology in people over 60 years of age masks the course of the underlying disease, which is responsible for late diagnosis and high mortality of patients. The protracted course of IE is characterized by low inoculability of the pathogen compared to acute forms of the disease. The development of thromboembolism of vessels in the systemic circulation is a characteristic clinical feature of subacute IE.
A positive effect from conservative therapy is observed in the majority of patients with IE with TC lesions, while in subacute endocarditis of the left chambers of the heart, conservative therapy is ineffective in most patients.
Hospital mortality in both groups of patients is due to dissemination of the pathogen with the formation of purulent foci and multiple organ failure, as well as the development of acute circulatory failure and secondary nephropathy.
Literature
- Butkevich O. M., Vinogradova T. L. Infective endocarditis. - M., 1997.
- Simonenko V. B., Kolesnikov S. A. Infective endocarditis: current course, diagnosis, principles of treatment and prevention. - Wedge. Med., 1999. - 3. - P. 44-49.
- Tazina S. Ya., Gurevich M. A. Modern infective endocarditis. - Wedge. med., 1999. - 12. - pp. 19-23.
- Bansal RC Infective endocarditis. Med Clin North America 1995; 79 (5): 1205-1239.
- Bayer AS, Bolger AF, Taubert KA et al. Diagnosis and management of infective endocarditis and its complications. Circulation 1998; 98: 2936-2948.
- McKinsey DS, Ratts TE, Bisno AI Underlying cardiac lesions in adults with infective endocarditis. The changing spectrum. Amer J Med 1987; 82: 681-688.
- Lamas CC Eykyn SJ Suggested modifications to the Duke criteria for the clinical diagnosis of native valve and prosthetic valve endocarditis: analysis of 118 pathologically proven cases. Clin Infect Dis 1997; 25: 713-719.
- Durack DT, Lukes AS, Bright DK et al. New criteria for diagnosis of Infective Endocarditis Utilization of Specific Echocardiographic Finding. Amer J Med 1994; 96: 200-209.
- Tyurin V.P., Dubinina S.V. Infectious endocarditis in elderly and senile people. - Wedge. Med., 2000. - 4. - P. 53-56.
V. I. Ulanova V. I. Mazurov, Doctor of Medical Sciences, Professor Medical Academy of Postgraduate Education, St. Petersburg
Classification and causes of endocarditis
In accordance with the causes and clinical manifestations, the disease is classified as follows.
Infectious (bacterial) endocarditis most often manifests itself in an acute form. Ulcers and polyps form on the heart valves or in the heart tissues, which lead to functional disorders.
The chronic or subacute form is usually caused by streptococci. The disease is manifested by ulceration and changes in the shape of the heart valves, the formation of blood clots in the vessels, followed by blockage. The consequences may be inflammation of the kidneys and heart attacks of other organs.
A non-infectious disease occurs against the background of a general weakening of the body, with various intoxications, and in older people with the development of marasmus. Among the forms are degenerative warty, abacterial, etc. Most often it manifests itself in the form of thrombotic deposits on valve tissue.
Rheumatic endocarditis , as the name suggests, occurs due to rheumatism. In this case, inflammation spreads to the heart valves and causes heart defects. There are 4 forms: diffuse, acute warty, recurrent warty, fibroplastic.
Loeffler's endocarditis is characterized by an increase in blood eosinophils and a decrease in the volume of the heart chambers due to fibrous changes in the endocardium and then the myocardium. There are three stages: acute (cell death within 5-6 weeks), thrombotic (formation of blood clots and atrophy of some tissues), fibrosis (sclerosis and thickening of the endocardium).
Etiology and routes of infection
The causative agents of endocarditis are most often microorganisms such as streptococci, staphylococci, enterococci, but the cause of the disease can also be representatives of the normal microflora of the oropharynx, upper respiratory tract, as well as fungi. Infection can enter the body, for example, during surgical interventions (prosthetic valves, catheterization of large vessels, and even tooth extraction). The likelihood of IE is quite high in patients with weakened immunity and the presence of foci of chronic infection (chronic tonsillitis, boils). Endocarditis often develops against the background of pre-existing cardiac pathology.
From the entrance gate of the infection, the pathogen enters the heart cavity with the bloodstream, settles on the valve flaps and forms vegetations (growths). The surface of the valves becomes ulcerated and deformed. Most often, the aortic and mitral valves are damaged, less often the tricuspid and pulmonary valves. Platelets and fibrin threads, responsible for the formation of blood clots, settle here. Once the valve leaflets become so deformed that they cannot close completely, a valve defect is formed, which in turn can lead to heart failure.
Microbial vegetations also pose a great danger because their elements can break off from the endocardium and spread through the bloodstream throughout the body, infecting other organs and tissues and leading to blockage (embolism) of large vessels. That is why, with endocarditis, the blood supply to the kidneys, spleen, lungs, brain, and also the heart itself is disrupted.
Infectious (bacterial) endocarditis
In the acute form, the symptoms of bacterial endocarditis develop quite quickly. Typically, the infection affects the lining of the heart valves, 2-10 mm ulcers appear on the tissues of the valves, and the valves themselves swell - platelets and fibrin accumulate, and aneurysms form. As a result, one of the large vessels may become blocked by a blood clot, and valve particles may come off. In some cases, septic infarction cannot be excluded.
If you do not seek qualified help in time and do not start treatment:
- heart failure develops;
- the structure of valves and leaflets is deformed;
- arrhythmic phenomena appear;
- hemodynamics are impaired.
Patients with subacute septic endocarditis are characterized by the same manifestations of pathology, but in this case, most often the tissues are affected by thrombotic formations, which sooner or later clog one of the most important vessels.
Causes
There are many causes of endocarditis:
- infections;
- injuries;
- allergic diseases;
- intoxication;
- connective tissue damage.
Often endocarditis develops not as an independent disease, but as a consequence of other pathologies in the body. Both men and women are equally susceptible to the disease. It can occur at any age. Currently, about 130 types of microorganisms are known that can provoke endocarditis.
Endocarditis in children
In children, the most common bacterial type of this disease occurs. The pathology is expressed by damage to the mitral and aortic valves, and then spreads to the internal cardiac tissues:
- the child experiences acute toxicosis;
- endocardial tissue becomes inflamed;
- myocardial damage occurs;
- blood vessels may become clogged;
- blood flow is disrupted.
Infectious endocarditis in children usually develops at a faster rate; inflammation can spread to other internal organs and lead to liver and kidney failure. Therefore, in this case, it is necessary to seek professional cardiac help as soon as possible.
Symptoms of endocarditis
The disease is characterized by an asymptomatic course at an early stage, as well as a sudden exacerbation against the background of a relatively healthy state. Symptoms of endocarditis in adult patients usually appear 10-14 days after infection:
- fever with chills, profuse sweating;
- the temperature may rise for several days;
- signs of intoxication appear: headache, weakness, exhaustion;
- the skin may acquire a pale, yellowish tint;
- rashes may be observed on the mucous membranes, feet, and palms.
These signs indicate the presence of an infection in the body, so you should immediately consult a doctor and begin treatment.
They are complemented by more characteristic symptoms of infective endocarditis in adults, which indicate the development of this particular disease:
- arthritic changes in joints;
- damage to the heart valves;
- thrombosis and blockage of large arteries;
- enlarged lymph nodes;
- kidney infarction and other lesions;
- rapidly developing heart failure;
- pericarditis.
These symptoms of endocarditis are identified during diagnostic procedures.
Symptoms of the lesion
In 90% of patients, the temperature rises, sometimes there is a fever, it can be unstable.
85% of patients have a heart murmur. Half of the patients have the so-called classic signs of endocarditis:
- petechiae (small subcutaneous hemorrhages) are a common but nonspecific sign;
- subungual hemorrhages in the form of dark red lines;
- Osler's nodes: subcutaneous formations, often located in the area of the fingertips;
- Genway spots: painless lesions on the palmar surfaces and soles.
a) Janeway spots;
b) subungual hemorrhages; c) Osler's nodes; d) Lukin-Libman symptom (conjunctival hemorrhage). Neurological disorders are observed in 40% of patients:
- ischemic stroke;
- intracerebral hemorrhage;
- multiple microabscesses of the brain.
Other possible symptoms of endocarditis:
- heaviness in the area under the left rib due to an enlarged spleen;
- stiff neck, inability to tilt your head forward;
- mental disorders, delirium;
- paralysis, speech disorders;
- hemorrhages in the conjunctiva of the eye;
- pale skin;
- pulmonary wheezing, cough;
- abnormal heart rhythm;
- friction noise of the pleura or pericardium, determined by listening.
In subacute endocarditis, the symptoms are nonspecific:
- slight increase in temperature;
- lack of appetite;
- weight loss;
- flu-like symptoms;
- muscle pain;
- chest pain when breathing (due to pleural effusion);
- headache;
- heaviness in the right hypochondrium, vomiting, abdominal pain.
Possible complications of septic endocarditis:
- myocardial infarction, inflammation of the heart sac (pericarditis), cardiac arrhythmias;
- circulatory failure;
- aneurysm of the sinus of Valsalva;
- abscess of the heart muscle or aortic root;
- vascular emboli, mycotic aneurysms;
- arthritis, myositis;
- glomerulonephritis, renal failure;
- stroke;
- abscess or infarction of the spleen or mesentery.
For information about the causes and symptoms of septic endocarditis, watch this video:
Diagnosis of endocarditis
Qualified diagnosis of infective endocarditis is a whole complex of examinations. The patient is prescribed a cardiac screening program, which includes:
- various types of electrocardiogram (24-hour monitoring, stress echocardiography);
- Ultrasound of the heart and blood vessels;
- computer sphygmomanometry.
Modern diagnostic methods are also applicable: cardiac rhythmography, Dopplerography. Blood tests and cultures for sterility are required - one of the most important examinations for infective endocarditis.
Treatment of endocarditis
At an early stage, treatment of infective endocarditis consists of antibiotic therapy and cardiac support with medications. If septic endocarditis has already manifested itself as significant changes in the tissues of the heart (damage to the valves, aorta, myocardium), surgical intervention is possible.
- Antibacterial treatment for symptoms of endocarditis involves the use of modern antibiotics (benzylpenicillin, penicillins, amphotericin, etc.) administered intravenously.
- Passive immunization is carried out to neutralize bacteria in the body. For this purpose, special antitoxic serums (immunoglobulin, hyperimmune plasma) are most often used intravenously.
- Surgical intervention is performed in cases where it is necessary to remove foci of infection in the tissues of the heart and restore cardiac structures altered by the disease. The services of a cardiac surgeon are necessary if the patient has progressive heart failure, vascular thromboembolism, etc.
What is backendocarditis
Any organism cannot be completely protected from the ingress of dangerous microorganisms. If bacteria penetrate the blood, a dangerous and serious disease occurs - endocarditis, associated with inflammation of the inner lining of the heart. The membrane of the heart (lining) is called the endocardium. In this case, both the valvular and parietal endocardium may be affected.
Backendocarditis or otherwise bacterial endocarditis is associated with septic (infectious) damage to the lining of the heart, when bacteria (most often streptococci, staphylococci, enterococci, and others) found in the body enter the membrane and begin active reproduction. Also, microorganisms that influence the formation of endocarditis include fungi. You can often find other names for a disease that occurs under the influence of bacteria: infective endocarditis or septic endocarditis.
For reference. The risk group for backendocarditis includes drug addicts, since under the influence of drugs, the lining of the heart suffers and is destroyed.
The disease can occur at any age, but according to statistics, males are affected 2 times more often than females.
- Infective endocarditis
Classification of backendocarditis
Statistics say that the nature of the disease may vary depending on the duration and severity of its development. It is customary to divide backendocarditis into three types:
- Spicy;
- Subacute;
- Chronic;
The duration of acute infective endocarditis reaches up to two weeks. The disease develops valve defects as a consequence.
The degree of complication of subacute infective endocarditis is slightly higher, so its duration can reach three months. The disease is characterized by the formation of various types of ulcers on the myocardial valves and thrombotic growths.
As for the last stage, such an infectious disease is practically untreatable, and the symptoms haunt the patient for years. Chronic bacterial endocarditis occurs when the mother has a chronic infectious disease.
There is a classification of this disease according to one more criterion - the presence or absence of a background disease.
- Primary infective endocarditis occurs on undamaged (intact) valves. This can happen if the body suffers complications after a disease such as acute respiratory viral infection or due to stress and overwork. Statistics say that about 6% of cases of disease are associated with primary endocarditis.
Endocarditis can also be parietal fibroplastic eosinophilic (Leffler's endocarditis). This disease causes the chambers of the heart to thicken or narrow.
As a result, heart failure may occur. There are three stages:
- spicy _ It lasts for 6 weeks. Inflammatory processes affect the ventricles and heart muscle. Dead cells appear.
- thrombotic . Thrombi appear on the endocardium of the left and right ventricles. The development of focal sclerosis and the growth of young connective tissue occurs.
- stage of fibrosis . At this stage, you can notice a narrowing of the heart chambers and the appearance of signs of heart disease.