Types of hyperlipidemia
The classification of hyperlipidemia is based on LDL, HDL, and triglycerides.
The concentration of lipoproteins is measured: Low density - LDL, VLDL, TG;
- High density HDL.
It is cholesterol that has a low density that is considered “bad”. It forms plaques and creates a risk of developing vascular pathology. It is important for the doctor to achieve a reduction in LDL cholesterol. However, total cholesterol levels may remain slightly elevated.
In total, there are 6 types of hyperlipedemia. Three of them are considered dangerous: 2a, 2b and 3. They are dangerous because they threaten the formation of dense plaques.
Type 2 is considered common. It is divided into 2a and 2b. With 2a, an increase in LPN and total cholesterol is observed. 2b – all factions are increased.
*Note: 4 and 5 can also be atherogenic with low HDL and other metabolic disorders.
By what indicators can one judge about impaired fat metabolism?
The mechanisms of dyslipidemia often remain unknown. In the laboratory, the main indicators that are directly involved in assimilation and production are identified.
Lipoproteins are complexes of proteins combined with fats, the only way fat molecules can dissolve in liquid.
The condition of the liver cells directly affects the production and circulation of fat components
Based on density they are distinguished:
- high - lipoprotein compounds are carried freely, without settling in the walls of the arteries, they are processed into cholesterol in the liver, enter the gall bladder and ducts, then into the intestines and participate in motility, ensuring the release of the body from toxins;
- low - needed for the delivery of cholesterol into cells for the purpose of “construction” and participation in the synthesis of vitamins and hormones, along the way they lose cholesterol in the form of atherosclerotic deposits in the inner wall of the vessel, in places where there is damage caused by viruses;
- a fraction of “very low” density and its predecessor “intermediate density” were isolated - they play an even more negative role in vascular damage.
Triglycerides give the body energy. They themselves are not deposited as part of the atherosclerotic plaque, but they affect the decrease in the activity of the high-density fraction of lipoproteins, so the increase in triglycerides contributes to the atherosclerotic process.
To more fully take into account the balance of the influence of fat metabolism indicators on the risk of arterial damage, the calculation of the atherogenicity coefficient has been adopted by determining the ratio of “negative” fractions to high-density lipoproteins.
Dyslipidemia in diagnosis is indicated by elevated blood test values:
- total cholesterol - over 6.2 mmol/l;
- low-density lipoproteins - 4.1 mmol/l and above;
- triglycerides - exceeding 2.3 mmol/l.
In this case, the atherogenic coefficient is more than 3.0.
What are the symptoms of lipidemia?
This abnormal accumulation of fat can begin during puberty, after pregnancy, or even during menopause.
Patients notice:
- Blood cholesterol levels - table by age. Cholesterol in the blood - norms for women, men and children
- Soft tissue pain when resting, walking, or touching.
- Sudden accumulation of lipid-lowering fat from the waist to the knees or ankles other than the feet.
- Fat accumulates in nodules or small pockets that put pressure on the joints until it becomes impossible to walk normally.
- The skin loses its elasticity.
- Bruising and swelling occur.
A few months after this first stage, patients notice the following symptoms:
- Constant feeling of cold.
- Fatigue.
- The skin takes on a rubbery texture.
- Chronic pain and gradual deterioration in mobility.
Combined with an unattractive appearance, these symptoms cause feelings of sensation, anger, and sadness until depression develops.
Signs of lipid metabolism disorders
In most cases, there are no signs of dyslipidemia, and it is detected by examining the blood when a patient visits for high blood pressure , heart pain , dizziness , etc. That is, the patient is examined already when the first manifestations of vascular atherosclerosis . With atherosclerosis of the vessels of the legs, pain in the legs appears when walking, and with atherosclerosis of the vessels of the brain - memory impairment, headaches and dizziness.
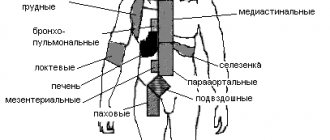
pancreatitis appear - bloating, mushy stools, heaviness and pain in the left hypochondrium or girdle pain. This is due to the fact that toxic products arising from the hydrolysis of large amounts of triglycerides affect the pancreas. An excess of chylomicrons causes microthrombosis in any organ. Triglycerides are deposited in the cells of the reticulohistiocytic system, so the spleen and liver enlarge. Ultrasound reveals fatty hepatosis (fatty liver), which is also a consequence of lipid metabolism disorders and often occurs without symptoms.
Characteristic skin changes are observed in hereditary hyperlipidemias.
- Flat xanthomas . These are yellowish stripes in the folds of the fingers and palms.
- A significant increase in triglyceride levels leads to the appearance of eruptive xanthomas . These are multiple nodular or spherical formations of yellow color, sometimes with a pink corolla. These elements are found throughout the body, but are more often detected on the back, buttocks, chest, elbows and knees.
- Most often, this skin pathology occurs in individuals with decompensated diabetes mellitus and severe triglyceridemia .
- Tendon xanthomas are yellowish nodules that form in the area of the tendons on the hands, in the area of the elbow joint and the Achilles tendon. Tendon xanthomas are a sign of familial hypercholesterolemia.
- Xanthelasma is a deposit of cholesterol under the skin of the eyelids in the form of flat yellow plaques. Xanthelasmas occur in biliary cirrhosis with normal lipid levels.
- The lipoid arch of the cornea appears as a white rim along the edges of the cornea. Its appearance at a young age indicates hereditary dyslipidemia.
Eruptive xanthomas
Xanthelasmas
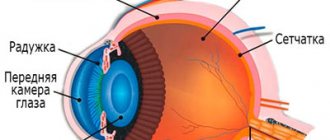
With severe hypertriglyceridemia, the arteries and veins of the retina are creamy white.
Lipoid arch
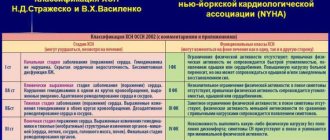
Classification
The classification of lipid disorders, based on changes in the profile of plasma lipoproteins when they are separated by electrophoresis or ultracentrifugation, was developed by Donald Fredrickson in 1965.[1]
The Fredrickson classification has been adopted by the World Health Organization as the international standard nomenclature for hyperlipidemias. However, it does not take into account the level of HDL, which is an important factor reducing the risk of atherosclerosis, as well as the role of genes that cause lipid disorders. For these reasons, it is sometimes considered outdated. However, the system remains the most common classification. Fredrickson classification of hyperlipidemias
| Hyperlipoproteinemia | Synonyms | Etiology | Detectable violation | Treatment |
| Type I | Primary hyperlipoproteinemia , Hereditary hyperchylomicronemia | Reduced lipoprotein lipase (LPL) or disorder of the LPL activator - apoC2 | Elevated chylomicrons | Diet |
| Type IIa | Polygenic hypercholesterolemia , Hereditary hypercholesterolemia | LDL receptor deficiency | Elevated LDL | Statins, Nicotinic acid |
| Type IIb | Combined hyperlipidemia | Decreased LDL receptor and increased apoB | Elevated LDL, VLDL and triglycerides | Statins, Nicotinic acid, Gemfibrozil |
| Type III | Hereditary dys-beta lipoproteinemia | ApoE defect (apoE 2/2 homozygotes) | Increased DILI | Mainly: Gemfibrozil |
| Type IV | Endogenous hyperlipemia | Increased formation of VLDL and their delayed breakdown | Elevated VLDL | Mainly: Nicotinic acid |
| Type V | Hereditary hypertriglyceridemia | Increased formation of VLDL and decreased lipoprotein lipase | Elevated VLDL and chylomicrons | Nicotinic acid, Gemfibrozil |
Hyperlipoproteinemia type I
A rare type of hyperlipidemia that develops due to LPL deficiency or a defect in the LPL activator protein, apoC2. Manifests itself in increased levels of chylomicrons, a class of lipoproteins that transport lipids from the intestines to the liver. The frequency of occurrence in the general population is 0.1%.
Hyperlipoproteinemia type II
The most common hyperlipidemia. Characterized by an increase in LDL cholesterol. Divided into types IIa and IIb depending on the absence or presence of high triglycerides.
Type IIa
This hyperlipidemia may be sporadic (as a result of poor diet), polygenic, or hereditary. Hereditary hyperlipoproteinemia type IIa develops as a result of a mutation in the LDL receptor gene (0.2% of the population) or the apoB gene (0.2% of the population). The familial or hereditary form is manifested by xanthomas and early development of cardiovascular diseases.
Type IIb
This subtype of hyperlipidemia is accompanied by an increased concentration of triglycerides in the blood as part of VLDL. High levels of VLDL occur due to increased formation of the main component of VLDL - triglycerides, as well as acetyl-coenzyme A and apoB-100. A more rare cause of this disorder may be slow clearance (removal) of LDL. The frequency of occurrence of this type in the population is 10%. This subtype also includes hereditary combined hyperlipoproteinemia and secondary combined hyperlipoproteinemia (usually in metabolic syndrome).
Treatment of this hyperlipidemia includes dietary changes as a major component of therapy. Many patients require statins to reduce the risk of cardiovascular disease. In cases of severe elevation of triglycerides, fibrates are often prescribed. The combination of statins and fibrates is highly effective, but has side effects such as the risk of myopathy, and should be under constant medical supervision. Other medications (nicotinic acid, etc.) and vegetable fats (ω3-fatty acids) are also used. [2]
Hyperlipoproteinemia type III
This form of hyperlipidemia is manifested by an increase in chylomicrons and DILI, therefore it is also called dys-beta-lipoproteinenia. The most common cause is homozygosity for one of the apoE isoforms, E2/E2, which is characterized by impaired binding to the LDL receptor. Occurrence in the general population is 0.02%.
- Hypertension of the 1st degree: causes, risk factors, diagnosis and treatment features
Hyperlipoproteinemia type IV
This subtype of hyperlipidemia is characterized by elevated triglyceride concentrations and is therefore also called hypertriglyceridemia. The frequency of occurrence in the general population is 1%.
Hyperlipoproteinemia type V
This type of hyperlipidemia is in many ways similar to type I, but is manifested not only by high chylomicrons, but also by VLDL.
Features of treatment
The first step in treating dyslipidemia is to prescribe a diet and give other recommendations not related to taking medications. They consist of the following rules:
- Minimize the amount of animal fat consumed. Perhaps abandon them completely;
- saturate your diet with plant fiber;
- lose weight if you are overweight;
- maintain physical activity under conditions of moderate exercise;
- make your diet balanced. Reduce portion sizes, increase the frequency of meals;
- give up alcohol and smoking.
Of course, you cannot do without medications, especially in severe forms of the disease, for example, in the asterogenic form of dyslipidemia, when a triad of metabolic disorders is observed in the body: an increase in LDL levels, a decrease in HDL, and an increase in the number of triglycerides. In any case, drug treatment will be carried out in several directions; the patient may be prescribed:
- statins - drugs that help lower cholesterol levels;
- cholesterol adsorption inhibitors - agents that create an obstacle to the absorption of cholesterol by the intestine;
- ion exchange resins. Such medications bind bile acids. They bring them out, along with the cholesterol they contain;
- fibrates – help reduce the number of triglycerides;
- Omega-3 polyunsaturated acids – protect the heart from MI and are needed to prevent cardiac arrhythmias.
Important! If we are talking about severe forms of the disease, such as atherogenic dyslipidemia, the patient may be prescribed extracorporeal treatment. It consists of changing the composition of blood outside the human body. This procedure helps prevent complications of the disease.
We looked at what dyslipidemia is and how to treat the disease. But, the prevention of pathology is an equally important topic. It consists of the following activities:
- proper and balanced nutrition with a minimum amount of animal fats;
- moderate physical activity, healthy sleep;
- eliminating bad habits;
- body weight control.
Compliance with these points is enough to significantly reduce the risk of metabolic disorders and the process of removing fat from the body.
Forecast
The prognosis for type I lipid metabolism disorders is relatively favorable, but there is a predisposition to pancreatitis . In type II, the prognosis depends on the severity of vascular damage. If early atherosclerosis develops and lipid metabolism disorders are not treated, complications are possible (coronary artery disease, stroke). Rational and timely treatment of hyperlipidemia can significantly reduce the risk of complications and improve the prognosis. For primary hyperlipidemia, lifelong therapy is carried out.
Risk group
People at risk for developing hyperlipidemia include:
- suffering from abnormalities of the endocrine system (diabetes or obesity);
- who have a history of close relatives with the development of atherosclerosis;
- abusing alcohol and tobacco products;
- those who do not follow proper nutrition (the predominance of fatty and fried foods in the diet);
- over the age of 50;
- leading a sedentary lifestyle.