Classification of pathology
Depending on the cause of the disease, there are 2 main types of diabetes mellitus: insulin-dependent (type 1) and non-insulin-dependent (type 2). In insulin-dependent diabetes, the pancreas does not synthesize insulin or produces it in insufficient quantities, and in non-insulin-dependent diabetes, tissue sensitivity to insulin decreases.
Additionally, a distinction is made between secondary diabetes (develops against the background of other diseases) and gestational diabetes (occurs in pregnant women).
Depending on compensation, diabetes mellitus is:
- compensated - carbohydrate metabolism is normalized, and glucose concentration approaches normal;
- subcompensated – blood sugar levels periodically increase or decrease;
- decompensated - neither diet nor medications can lower glucose, which is why diabetics often develop precoma or coma, which can lead to death.
To successfully compensate for diabetes, it is important to regularly measure blood sugar levels and make timely adjustments to treatment.
Diabetes: types and risk factors
International Diabetes Day has been celebrated around the world since 1991. The decision to approve such a day belongs to the International Diabetes Federation and the World Health Organization, and since 2007 the events have been held with the support of the UN. November 14 was not chosen by chance. On this day in 1891, one of the scientists who discovered insulin, Frederick Banting, Nobel Prize laureate, was born.
According to WHO, from 1980 to 2014, the number of people with diabetes increased almost 4 times - from 108 million to 422. It is likely that today this number is even higher - firstly, the upward trend continues, and secondly, statistics only take into account those people who know about their disease and receive medical care about it. In any case, diabetes is one of the three leading causes of disability and death.
Degrees of diabetes
According to the WHO classification, there are 3 degrees of the disease:
- mild (glucose level does not exceed 7 mmol/l) - often occurs hidden, symptoms are absent or barely noticeable, complications do not arise;
- moderate (sugar concentration - 7-14 mmol/l) - complications are observed in the form of damage to the skin, blood vessels, heart, kidneys, eyes, nerves;
- severe (glucose level is in the range of 15-25 mmol/l, and sometimes higher) - severe complications occur (diabetic ulcers, kidney failure, gangrene of the extremities, diabetic coma), and death is possible.
Causes of the disease
The hereditary factor is of primary importance in the development of diabetes mellitus. Predisposition to the disease is transmitted through the maternal line in 5% of cases and through the father in 10% of cases. If both parents have diabetes, the risk of developing pathology reaches 100%.
Also, the main causes of non-insulin-dependent diabetes include:
- inactivity and overeating, leading to obesity - if body weight is 50% higher than normal, then the risk of increased glucose increases to 60%;
- poor nutrition.
The main causes of insulin-dependent diabetes:
- autoimmune diseases (lupus, autoimmune thyroiditis, glomerulonephritis, hepatitis);
- viral infections that destroy pancreatic beta cells responsible for the production of insulin (chickenpox, rubella, hepatitis, mumps).
Factors influencing the development of diabetes mellitus
There are two key points in the mechanisms of development of diabetes mellitus, on the basis of which the disease is divided into types:
- Low insulin production by intrasecretory pancreatic cells.
- Impaired ability of the hormone to act on the body, cell insensitivity to insulin.
If there is insufficient insulin production, type 1 diabetes develops. It is based on the progressive destruction of the islets of Langerhans (intrasecretory cells of the pancreas). This occurs as a result of autoimmune processes in the body - antibodies to insulin, secretory cell structures, and enzymes are produced.
Provoking factors for the development of autoimmune disorders can be:
- viral infections;
- malnutrition during pregnancy and breastfeeding;
- unfavorable environmental conditions;
- the effect of stress.
Type 1 diabetes is more often diagnosed in young people. The first manifestations of pathology occur when the death of intrasecretory cells reaches more than 80%. The disease occurs with a high risk of complications; all types of metabolism are significantly affected.
Type 2 diabetes occurs when tissue receptors are resistant to the action of insulin. In this case, the hormone is reproduced in normal or slightly reduced quantities. The mechanism of such disorders is associated with an initially defective structure of insulin (hereditary predisposition) or acquired changes, as a result of which signal transmission from receptors to the internal structures of the cell is disrupted.
The development of type 2 disease can be provoked by:
- improper diet, overeating;
- sedentary lifestyle;
- hypertonic disease;
- alcohol abuse;
- age-related changes;
- obesity;
- uncontrolled medication use.
Signs of the disease
The main symptoms and signs of diabetes are similar for both types of the disease:
- polydipsia - severe thirst;
- polyuria – frequent heavy urination, including at night (nocturia);
- Polyphagia – excessive appetite and constant hunger.
But there are also differences. For example, with type 1 diabetes, patients lose weight (despite a good appetite), and with type 2, they gain weight.
Diabetes mellitus in men is often accompanied by sexual problems: erectile dysfunction, early ejaculation, infertility.
Possible complications
In the absence of treatment or non-compliance with medical instructions, dangerous complications develop:
- diabetic ketoacidosis – accumulation of ketone bodies in the blood;
- hypoglycemia – a decrease in sugar concentration below normal (3.3 mmol/l);
- hyperosmolar coma – accompanied by severe dehydration;
- lactic acidotic coma - lactic acid accumulates in the blood and tissues;
- diabetic retinopathy – damage to the retina of the eye, leading to hemorrhages, possibly retinal detachment;
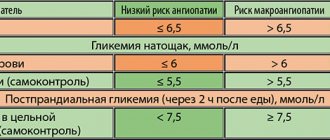
- diabetic macro- and microangiopathy – impaired permeability of blood vessels, increased fragility, tendency to thrombosis and atherosclerosis;
- diabetic polyneuropathy – damage to both parts of the nervous system (somatic and autonomic), which leads to pain in various parts of the body, deterioration of sensitivity and numbness of the lower extremities;
- diabetic nephropathy – kidney damage, eventually leading to kidney failure;
- diabetic arthropathy – pain and “crunching” in the joints, limited mobility of the limbs;
- diabetic ophthalmopathy - eye damage that contributes to the development of cataracts;
- diabetic encephalopathy – instability and sudden mood swings;
- diabetic foot – purulent-necrotic lesions of the foot, often leading to amputation.
It should be noted that the higher the blood glucose level and the longer the disease develops, the greater the risk of complications. Diabetics are 4-6 times more likely to develop malignant tumors. More than half of all amputations are caused by complications of diabetes mellitus.
Diabetes mellitus type 2 - symptoms and treatment
Treatment of type II diabetes involves solving the main problems:
- compensate for the lack of insulin;
- correct hormonal and metabolic disorders;
- implementation of therapy and prevention of complications.
To solve them, the following treatment methods are used:
- diet therapy;
- physical exercise;
- use of glucose-lowering drugs;
- insulin therapy;
- surgical intervention.
Diet therapy
The diet for type II diabetes, like a regular diet, requires an optimal ratio of the main substances contained in foods: proteins should make up 16% of the daily diet, fats - 24%, and carbohydrates - 60%. The difference between the diet for type II diabetes lies in the nature of the carbohydrates consumed: refined sugars are replaced by slowly digestible carbohydrates. Since this disease occurs in obese people, weight loss is the most important condition for normalizing blood glucose levels. In this regard, a caloric diet is recommended, in which the patient will lose 500 g of body weight weekly until reaching the ideal weight. However, weekly weight loss should not exceed 2 kg, otherwise this will lead to excessive loss of muscle rather than fat tissue. The number of calories required for the daily diet of patients with type II diabetes is calculated as follows: women need to multiply their ideal weight by 20 kcal, and men by 25 kcal.
When following a diet, it is necessary to take vitamins, since during diet therapy they are excessively excreted in the urine. The lack of vitamins in the body can be compensated by rational consumption of healthy foods, such as fresh herbs, vegetables, fruits and berries. During the winter and spring periods, it is possible to take vitamins in yeast form.
Exercise stress
A correctly selected system of physical exercises, taking into account the course of the disease, age and present complications, contributes to a significant improvement in the condition of the patient with diabetes. This treatment method is good because the need to use insulitis practically disappears, since during physical activity glucose and lipids are burned without its participation.
Treatment with glucose-lowering drugs
Today, derivatives of glucose-lowering drugs are used:
- sulfonylureas (tolbutamide, glibenclamide);
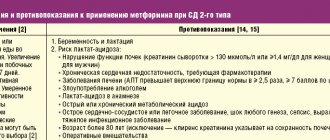
- biguanides, which reduce gluconeogenesis in the liver and increase the sensitivity of muscles and liver to insulin (metformin);
- thiazolidinediones (glitazones), similar in properties to biguanides (pioglitazone, rosiglitazone);
- alpha-glucosidase inhibitors, which reduce the rate of glucose absorption in the gastrointestinal tract (acarbose);
- agonists of glucagon-like peptide-1 receptors, stimulating the synthesis and secretion of insulin, reducing liver glucose production, appetite and body weight, slowing down the evacuation of the food bolus from the stomach (exenatide, liraglutide);
- depeptidyl peptidase-4 inhibitors, which also stimulate the synthesis and secretion of insulin, reduce the production of glucose by the liver, do not affect the rate of evacuation of food from the stomach and have a neutral effect on body weight (sitagliptin, vildagliptin);
- inhibitors of sodium-glucose cotransporter type 2 (gliflozin), which reduce the reabsorption (absorption) of glucose in the kidneys, as well as body weight (dapagliflozin, empagliflozin).
Insulin therapy
Depending on the severity of the disease and the complications that arise, the doctor prescribes insulin. This treatment method is indicated in approximately 15-20% of cases. Indications for the use of insulin therapy are:
- rapid weight loss for no apparent reason;
- the occurrence of complications;
- insufficient effectiveness of other glucose-lowering drugs.
Surgery
Despite the many hypoglycemic drugs, the question of their correct dosage, as well as patient adherence to the chosen method of therapy, remains unresolved. This, in turn, creates difficulties in achieving long-term remission of type II diabetes. Therefore, surgical therapy for this disease—bariatric or metabolic surgery—is becoming increasingly popular around the world. The IFD considers this method of treating patients with type II diabetes to be effective. Currently, more than 500,000 bariatric surgeries are performed worldwide each year. There are several types of metabolic surgery, the most common being gastric bypass and mini gastric bypass.[4]
Roux-en-Y gastric bypass
During bypass surgery, the stomach is divided below the esophagus so that its volume is reduced to 30 ml. The remaining large part of the stomach is not removed, but is sealed, preventing food from entering it.[5] As a result of the intersection, a small stomach is formed, to which the small intestine is then sewn, 1 m away from its end. This way, food will go directly into the large intestine, while its processing by digestive juices will be reduced. This, in turn, provokes irritation of L-cells in the ileum, which contributes to a decrease in appetite and an increase in the growth of cells that synthesize insulin.
Mini gastric bypass
The main difference between mini-gastrobypass and classic gastric bypass is the reduction in the number of anastomoses (connections of intestinal segments).[2] When performing a traditional operation, two anastomoses are performed: the connection of the stomach and small intestine and the connection of different parts of the small intestine. With mini-gastrobypass, there is only one anastomosis - between the stomach and the small intestine. Due to the small volume of the newly formed stomach and the rapid entry of food into the small intestine, the patient has a feeling of fullness even after eating small portions of food.
Other types of bariatric surgery include:
- gastropplication - suturing the stomach to prevent it from stretching;[8]
- sleeve gastroplasty (otherwise called laparoscopic longitudinal gastrectomy) - cutting off most of the stomach and forming a 30 ml gastric tube, which promotes rapid saturation and also allows you to avoid following a strict diet;
- Gastric banding is a reduction in the volume of the stomach using a special ring (band) placed on the upper part of the stomach (this intervention is reversible).
Contraindications to surgical treatment are the presence of esophagitis (inflammation of the mucous membrane of the esophagus), varicose veins of the esophagus, portal hypertension, liver cirrhosis, gastric or duodenal ulcer, chronic pancreatitis, pregnancy, alcoholism, severe diseases of the cardiovascular system or mental illness. disorders, as well as long-term use of hormonal drugs.
Treatment methods
Currently, there is no way to eliminate the cause of the disease and completely cure diabetes mellitus. Therefore, diabetics are prescribed symptomatic treatment aimed at getting rid of unpleasant symptoms, maintaining stable glucose levels, normalizing body weight and preventing complications.
For type 1 diabetes mellitus, insulin therapy is prescribed, and for type 2 diabetes, sugar-lowering drugs are prescribed. Moderate physical activity and proper diet are important for successful treatment.
MODY-diabetes
MODY diabetes is caused by a genetic defect that interferes with the secretion of insulin by the beta cells of the islets of Langerhans in the pancreas. MODY diabetes is not very common - about 5% of diabetic patients have this form of the disease. The onset of the disease usually occurs at a fairly early age. This type of diabetes mellitus is treated with the use of insulin, but to achieve optimal blood glucose levels, the patient requires low doses of insulin. Compensation for this type of diabetes is achieved quite easily. Figuratively speaking, MODY diabetes occupies a “middle” position between type 1 and type 2 diabetes.