Home Eye diseases
|
Reasons
|
Classification
|
Symptoms
|
Diagnostics
|
Treatment of uveitis
|
In the eye, between the sclera and the retina, there is the most important structure - the choroid , or, as it is also called, the uveal tract . It is divided into an anterior part (iris and ciliary body) and a posterior part (choroid, from the Latin Chorioidea - the choroid itself). The main function of the iris is to regulate the amount of light entering the retina. The ciliary body is responsible for the production of intraocular fluid, fixation of the lens, and also provides an accommodation mechanism. The choroid performs the most important function of delivering oxygen and nutrients to the retina.
Uveitis is an inflammatory disease of the choroid of the eye. Its causes and manifestations are so diverse that even a hundred pages may not be enough to describe them. There are even ophthalmologists who specialize only in the diagnosis and treatment of this pathology.
The anterior and posterior parts of the choroid are supplied with blood from different sources, so isolated lesions of their structures most often occur. The innervation is also different (the iris and ciliary body are by the trigeminal nerve, and the choroid has no sensitive innervation at all), which causes a significant difference in symptoms.
The disease can affect patients regardless of gender and age and is one of the leading causes of blindness (about 10% of all cases) in the world. According to various sources, the incidence is 17-52 cases per 100 thousand people per year, and the prevalence is 115-204 per 100 thousand. The average age of patients is 40 years.
Finland has the highest incidence, possibly due to the high incidence of HLA-B27 spondyloarthropathy (one of its causes) in the population.
Causes
Often it is not possible to determine the cause (idiopathic uveitis). Provoking factors can be genetic, immune or infectious diseases, injuries.
It is believed that the cause of this disease after injury is the development of an immune reaction that damages the cells of the uveal tract in response to microbial contamination and the accumulation of decay products of damaged tissues. When the disease is infectious, the immune system begins to destroy not only foreign molecules and antigens, but also its own cells. In cases where uveitis occurs against the background of an autoimmune disease, the cause may be damage to the choroid's own cells by immune complexes, as a result of a hypersensitivity reaction.
Diseases that most often contribute to the occurrence of uveitis include: seronegative arthropathy (ankylosing spondylitis, Reiter's syndrome, psoriatic arthropathy, inflammatory bowel disease (Crohn's disease, ulcerative colitis)), rheumatoid arthritis, systemic lupus erythematosus, Behçet's disease, sarcoidosis, tuberculosis, syphilis, herpes virus, toxoplasmosis, cytomegalovirus, AIDS.
According to Rodrigues A. et al. (1994), idiopathic uveitis predominates among other forms and accounts for about 34%. Seronegative spondyloarthropathy causes the disease in 10.4% of cases, sarcoidosis - in 9.6%, juvenile rheumatoid arthritis - in 5.6%, systemic lupus erythematosus - in 4.8%, Behçet's disease - in 2.5%, AIDS - at 2.4%. According to the same author, anterior uveitis is the most common (51.6%), posterior - in 19.4% of cases.
When identifying symptoms of uveitis in a patient, it is necessary to remember about the “masquerade” syndrome, which imitates the disease. It can be of either a non-tumor nature (with intraocular foreign bodies, retinal detachments, myopic dystrophies, pigment dispersion syndrome, retinal dystrophies, circulatory disorders in the eye, reactions to the administration of medications), or tumor (with such oncological diseases as intraocular lymphomas, leukemia , uveal melanoma, metastases of tumors of other localizations, paraneoplastic syndrome, cancer-associated retinopathy, retinoblastoma).
Consequences and complications
Severe trophic disorders, the action of toxins, epithelial lesions, pupillary fusion, congestion and exudation in the retina can lead to such serious consequences and complications as:
- clouding of the lens or in other words - cataract ;
- secondary glaucoma;
- atrophy of the eyeball;
- neuritis;
- exudative retinal detachment;
- band-shaped corneal degeneration.
Classification
The International Working Group on Standardization of Uveitis Nomenclature has developed recommendations for the classification of this disease.
Thus, according to localization it is customary to distinguish
| Type | Primary localization of inflammation | Manifestations |
| Anterior uveitis | Front camera | Iritis, iridocyclitis |
| Peripheral (medium, intermediate) uveitis | Vitreous body | Posterior cyclitis, hyalite, parsplanite |
| Posterior uveitis | Choroid | Choroiditis, chorioretinitis, retinitis, neuroretinitis |
| Panuveitis | All of the above | All of the above |
As we see, inflammation can involve both structures belonging to various parts of the choroid and surrounding tissues (sclera, retina, optic nerve).
Based on the causes of occurrence, uveitis is divided into infectious (bacterial, viral, fungal, parasitic, etc.), non-infectious (associated or not associated with known systemic diseases) and “masquerade” syndromes (tumor or non-tumor nature), simulating these diseases.
Based on the morphological picture , focal (granulomatous) and diffuse (non-granulomatous) uveitis are distinguished.
The onset of the disease can be either sudden or hidden, practically asymptomatic. Based on duration, uveitis is divided into limited (up to 3 months) and persistent. According to their course, they can be: acute (sudden onset and limited duration), recurrent (periods of exacerbation alternating with periods of remission without treatment for more than three months) and chronic (persistent uveitis with relapses less than 3 months after cessation of treatment).
To determine the degree of activity of the inflammatory process, cellular opalescence and the presence of cellular elements in the anterior chamber of the eye are assessed.
Uveitis is also differentiated according to many other parameters: morphological, patient age, immune status, etc.
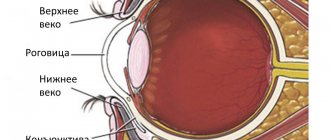
Uveal tract
The choroid is the most important structure of the eye. It is located between the sclera and the retina. It has front and back parts. The anterior part is represented by the iris and ciliary body, the posterior part by the choroid itself (choroid).
- The iris regulates the amount of light entering the retina.
- The ciliary body is responsible for the production of intraocular fluid, fixes the lens, and provides a mechanism of accommodation.
- The choroid performs the function of delivering oxygen and nutrients to the retina of the eye - the inner layer (it is the peripheral part of the visual analyzer).
Rice. 1a. The photo shows a schematic representation of the structure of the eye.
Symptoms
The symptoms of uveitis depend on many factors. The main ones are the localization of the inflammatory process (anterior, middle, posterior) and its duration (acute or chronic). Depending on the cause, specific manifestations characteristic of this form of the disease may be identified.
Anterior uveitis
The most common form - acute anterior uveitis - is usually accompanied by a sudden onset, severe pain on the affected side (typically increased pain at night, with changes in lighting, pressing on the eyeball in the limbus), photophobia, blurred or decreased vision, lacrimation, characteristic redness of the eye (ciliary or mixed injection of the eyeball), narrowing of the pupil and weakening of its reaction to light due to sphincter spasm. The symptoms of chronic anterior uveitis are similar, but are usually less severe, and some are even absent.
Upon examination, the ophthalmologist can detect the presence of cellular elements, purulent and fibrinous exudate (hypopyon) in the aqueous humor of the anterior chamber, its opalescence (Tyndall phenomenon); deposits (precipitates) on the posterior surface of the cornea; characteristic deposits on the pupillary edge of the iris (Keppe's nodes) or in its middle zone on the anterior surface (Boussac's nodes); posterior or anterior fusion of the iris with surrounding structures (synechia), its atrophic changes; difference in color between the right and left eyes (heterochromia); the appearance of pathological vessels in the iris (rubeosis). IOP levels can vary from low to high.
Average uveitis
Inflammation of the choroid in this localization is accompanied by floating opacities in the field of vision, deterioration of vision in the absence of pain (the clinical picture is similar to posterior uveitis), and mild photophobia.
Posterior uveitis
With this form of the disease, patients note blurring, decreased visual acuity, the appearance of floaters, image distortion, photopsia in the absence of pain, redness and photophobia. The appearance of pain with uveitis of posterior localization may indicate involvement in the inflammatory process of the anterior chamber of the eye, bacterial endophthalmitis, or posterior scleritis.
An ophthalmological examination can reveal the presence of cellular exudate in the vitreous body, exudative and hemorrhagic preretinal and intraretinal lesions of various shapes and types, which in the inactive stage can turn into atrophic areas with scarring, affecting surrounding tissues.
Patients with panuveitis may experience all of these symptoms.
Panuveitis
Generalized uveitis or panuveitis is a serious disease that affects all membranes of the eye. Accompanied by severe impairment of both central and peripheral vision. The disease is dangerous for its complications, the most severe of which are loss of vision and the eye as an organ. Panuveitis is bilateral in nature with varying degrees of severity in the right and left eyes.
The causes of the disease in most cases remain unclear. Pathogenesis is closely related to immune processes. The disease is often detected in sarcoidosis and tuberculosis.
The complaints of patients and the ophthalmoscopic picture are related to which parts of the vascular tract are predominantly affected. Signs of the disease are observed in different combinations and have varying degrees of severity.
Rice. 16. Panuveitis is a serious disease that affects all membranes of the eye.
Rice. 17. Cytomegalovirus infection. Multiple isolated lesions on the retina in the form of “cotton-wool spots”, which arise as a result of occlusion of capillaries and arterioles (retinal infarction).
Rice. 18 and 18.1. Consequences of toxoplasma uveitis. Retinal damage. Retinal scar (photo on the left).
Rice. 19. Behcet's disease (connective tissue disease). Anterior uveitis, hypopyon, retinitis, inflammation of the optic nerve and retinal vasculitis are severe manifestations of the disease.
Diagnostics
The most important thing in diagnosis is a correct and complete history taking. This saves the patient from undergoing unnecessary types of examination. Many experts have even proposed various questionnaires containing key questions for implementation. They help to standardize the survey and avoid incomplete clarification of the medical history.
There are no mandatory specific ophthalmological diagnostic methods. A general complete examination will reveal certain characteristic signs of the disease. It is important to pay attention to the level of intraocular pressure, which, according to Herbert, tends to increase in approximately 42% of patients. Inspection of the anterior segment is indispensable, which will help identify precipitates on the posterior surface of the cornea, hypopyon or pseudohypopyon, changes in the iris and other characteristic changes. To differentiate changes in the posterior segment of the eye, in addition to the standard examination of the fundus, FA and OCT can be used.
Laboratory diagnostics (PCR, HLA typing and others), X-ray, MRI and cytological methods of examination are carried out according to indications depending on the suspected cause.
In 2005, a working group to standardize the nomenclature of uveitis developed recommendations on the scope of diagnostic measures for various forms of uveitis (see Appendix). They contain a list of the main examinations necessary in each specific clinical case and help to avoid prescribing unfounded ones.
A special place is occupied by the diagnosis of “masquerade” syndrome, which imitates the symptoms of uveitis. It should be suspected in cases of minimal response to aggressive drug therapy. The scope of diagnostic procedures depends on the suspected cause.
It is important to understand that the purpose of the examination may be not only to establish the cause of the disease, but also to exclude pathology, the treatment of which is excluded by certain drugs (for example, infectious, in particular those that cannot be identified by specific tests, “masquerade” syndrome); systemic diseases that can worsen the patient’s general condition, prognosis of recovery, and require correction of the treatment regimen.
Congenital aniridia
| A disease in which the iris is absent (see structure of the eye). At the same time, behind the cornea there is a picture of a maximally dilated pupil, that is, blackness. Sometimes a rim is visible - a remnant (rudiment) of the iris root and ciliary processes (see.
|
You can find out more about surgical treatment here
Treatment
Drug treatment
.
Treatment of uveitis directly depends on the cause of the disease.
Due to the fact that it is often not possible to establish it, regimens contain drugs that are symptomatic or prescribed empirically until the etiology of inflammation is established. Specific treatment should be applied after identifying the cause of the disease. The gold standard of treatment is corticosteroids . The main goals of the prescription are: reducing exudation, stabilizing cell membranes, inhibiting the production of inflammatory hormones and the lymphocytic reaction. The choice of a specific drug of this group, as well as the method of administration, is carried out taking into account the activity of the inflammatory process, the tendency to increase IOP, etc. Currently, local and systemic use is possible, as well as installation of an implant into the cavity of the eyeball or under the membranes of the eye that releases the medicinal substance in small doses over a long period of time.
The next most often prescribed for uveitis are drugs with cycloplegic and mydriatic action. Their use is due to the prevention of the formation of synechiae (fusions) of the iris with surrounding structures, reducing pain by reducing spasm of the pupillary and ciliary muscles, stabilizing the blood-ophthalmic barrier and preventing further leakage of protein into the aqueous humor.
Second-line drugs are NSAIDs. They have less anti-inflammatory activity compared to steroids, but can be useful for relieving pain, inflammatory reactions, preventing and treating relapses of the disease, as well as macular edema accompanying it in some cases. When prescribed together with corticosteroids, NSAIDs help reduce the dose of the former required to relieve inflammation during long-term treatment of some forms of chronic uveitis. The drug can be prescribed both in the form of eye drops and in tablet form.
Separate attention should be paid to a relatively new group of drugs - immunomodulators, which are now successfully used in some forms of the disease (for example, caused by Behçet's disease, involving the posterior segment of the eye; Wegener's granulomatosis; necrotizing scleritis). This group includes antimetabolites (methotrexate, azathioprine, mycophenolate mofetil), T-lymphocyte inhibitors (cyclosporine and tacrolimus), alkylating agents (cyclophosphamide, chlorambucil). The goal of this therapy is targeted inhibition of certain mechanisms of the immune inflammatory response that led to damage to the organ of vision (immunosuppression). The drugs can be used both together with corticosteroids and without them, allowing to reduce the negative impact of the latter on the body.
Recently, it has also become possible to use in special forms of the disease (serpinginous choroiditis, shotgun chorioretinitis, sympathetic ophthalmia; caused by Behçet, Vogt-Koyanagi-Harada diseases, juvenile idiopathic arthritis, seronegative spondyloarthropathies) drugs inhibitors of growth factor-α tumors, or so called biological therapy. The most commonly used are adalimumab and infliximab. All biological agents are “second-line” drugs in the treatment of these diseases and are used in cases where previous therapy was unsuccessful.
Surgery
The goals of this type of treatment are visual rehabilitation, diagnostic biopsy to clarify the diagnosis, removal of clouded or altered structures that make it difficult to examine the posterior segment of the eye or contribute to the development of complications (cataracts, vitreous destruction, secondary glaucoma, retinal detachment, epiretinal membrane), administration of drugs directly to the site of inflammation. Also, removal of the affected eye structures can help relieve the inflammatory process. The most commonly used surgical methods include vitrectomy, phacoemulsification, glaucoma filtering surgery, and intravitreal injections.
The success of these interventions directly depends on the timeliness of their implementation, the stage of the disease, and the prevalence of irreversible changes in the eyeball.
Prognosis for the treatment of uveitis
Patients suffering from uveitis should be informed of the importance of following the prescribed treatment and examination regimen. This is the main factor determining a favorable prognosis for the outcome of the disease. Some forms of the disease are capable of recurrence, even despite adequate treatment.
Of course, uveitis itself is not fatal, but if not treated adequately it can cause blindness.
Application
Recommendations on the scope of diagnostic measures for various forms of uveitis. .
Bibliography
1) Saadia Zohra Farooqui, MBBS Senior Resident, Singapore National Eye Centre, Singapore General Hospital, Singapore, Uveitis Classification, 2021. [Medscape] 2) Monalisa N Muchatuta, MD, Iritis and Uveitis Clinical Presentation, 2021. [Medscape] 3) Herbert HM, Viswanathan A, Jackson H, Lightman SL. Risk factors for elevated intraocular pressure in uveitis. J Glaucoma. 2004;13(2):96–9 4) C. Stephen Foster, Albert T. Vitale. Diagnosis and treatment of uveitis. Jaypee-Highligths, 2013. 5) Niaz Islam, Carlos Pavesio, Uveitis (acute anterior), 2009. [Academia] 6) Robert H Janigian, Jr, MD, Uveitis Evaluation and Treatment, 2021. [Medscape] 7) Monalisa N Muchatuta , MD, Iritis and Uveitis Follow-up, 2021. [Medscape] George N. Papaliodis. Uveitis. A practical Guide to the Diagnosis and Treatment of Intraocular Inflammation. Springer, 2021 9) Kanski's Cinical Ophthalmology. A systematic approach. 8th edition. Eisevier, 2021 10) E.A. Egorov. Emergency ophthalmology: Textbook. Pos. M.: GEOTAR-Media, 2005
Risk factors for elevated intraocular pressure in uveitis. J Glaucoma. 2004;13(2):96–9 4) C. Stephen Foster, Albert T. Vitale. Diagnosis and treatment of uveitis. Jaypee-Highligths, 2013. 5) Niaz Islam, Carlos Pavesio, Uveitis (acute anterior), 2009. [Academia] 6) Robert H Janigian, Jr, MD, Uveitis Evaluation and Treatment, 2021. [Medscape] 7) Monalisa N Muchatuta , MD, Iritis and Uveitis Follow-up, 2021. [Medscape] George N. Papaliodis. Uveitis. A practical Guide to the Diagnosis and Treatment of Intraocular Inflammation. Springer, 2021 9) Kanski's Cinical Ophthalmology. A systematic approach. 8th edition. Eisevier, 2021 10) E.A. Egorov. Emergency ophthalmology: Textbook. Pos. M.: GEOTAR-Media, 2005
Author
: Ophthalmologist E. N. Udodov, Minsk, Belarus.
Date
of publication (update): 06/24/2021
Diet for uveitis
Diet to boost immunity
- Efficacy: therapeutic effect after 3 weeks
- Terms: 1-3 months or more
- Cost of products: 1600-1800 rubles. in Week
If uveitis is non-traumatic in nature, then the severity of the course and the speed of development of pathogenesis directly depends on the state immunity . Therefore, to prevent uveitis, in addition to eye hygiene and regular examinations by an ophthalmologist, it is important to have a nutritious diet rich in vitamins (especially A and E) and foods that increase the body’s resistance. It is advisable to include in the diet:
- seafood, including cod and oysters;
- chicken eggs;
- nuts and seeds;
- carrots, apricots, citrus fruits and other orange fruits and vegetables;
- sprouted wheat, spinach and microgreens;
- Blueberries, which are also very good for vision, are rich in vitamin A and antioxidants .
Coloboma of the iris
| Typically, iris coloboma is located inferiorly at 06.00. clock, resembling a pear or a keyhole (see.
|
You can learn about plastic restoration of the pupil in our video
Install Flash Player to watch the movie.
Prevention
Carefully following the doctor's recommendations and attending all scheduled appointments with the rheumatologist and ophthalmologist, your child's vision problems should be under control - the main preventive measures.
It is recommended to visit doctors regularly (every 3–6 months) to ensure that there are no changes in the condition of the optical system.
Prevention is as follows:
- proper hygiene;
- minimizing injury;
- strengthening the immune system with drugs and hardening;
- minimizing exposure to toxic substances.