Blood coagulation is an extremely complex and in many ways still mysterious biochemical process that is triggered when the circulatory system is damaged and leads to the transformation of blood plasma into a gelatinous clot that plugs the wound and stops bleeding. Disturbances in this system are extremely dangerous and can lead to bleeding, thrombosis or other pathologies, which together are responsible for the lion's share of mortality and disability in the modern world. Here we will look at the structure of this system and talk about the most modern achievements in its study.
Anyone who has received a scratch or wound at least once in their life has thus acquired a wonderful opportunity to observe the transformation of blood from a liquid into a viscous non-flowing mass, leading to the cessation of bleeding. This process is called blood coagulation and is controlled by a complex system of biochemical reactions.
Having some kind of system to stop bleeding is absolutely necessary for any multicellular organism that has a liquid internal environment. Blood clotting is also vital for us: mutations in the genes of the main clotting proteins are usually lethal. Alas, among the many systems of our body, disturbances in the functioning of which pose a danger to health, blood clotting also takes absolute first place as the main direct cause of death: people suffer from various diseases, but almost always die from blood clotting disorders. Cancer, sepsis, trauma, atherosclerosis, heart attack, stroke - for a wide range of diseases, the direct cause of death is the inability of the coagulation system to maintain a balance between the liquid and solid states of blood in the body.
If the reason is known, why can’t it be fought? Of course, it is possible and necessary to fight: scientists are constantly creating new methods for diagnosing and treating coagulation disorders. But the problem is that the coagulation system is very complex. And the science of regulating complex systems teaches that such systems need to be managed in a special way. Their reaction to external influences is nonlinear and unpredictable, and in order to achieve the desired result, you need to know where to put the effort. The simplest analogy: to launch a paper airplane into the air, you just need to throw it in the right direction; at the same time, for an airliner to take off, you will need to press the right buttons in the cockpit at the right time and in the right sequence. But if you try to launch an airliner with a throw, like a paper airplane, it will end badly. It’s the same with the coagulation system: in order to successfully treat, you need to know the “control points”.
Until very recently, blood clotting successfully resisted researchers' attempts to understand its workings, and only in recent years has there been a qualitative leap. In this article we will talk about this remarkable system: how it works, why it is so difficult to study, and - most importantly - we will tell you about the latest discoveries in understanding how it works.
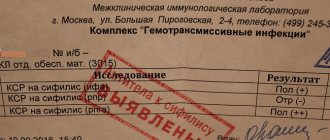
Detailed description of the study
Blood clotting is a complex, multi-step process that involves numerous factors. Blood coagulation factors are protein substances that are found in blood plasma (plasma factors) and platelets (platelet factors). They are involved in the formation of a blood clot (thrombus). In total, thirteen plasma factors and twenty-two platelet factors are distinguished. Laboratory studies make it possible to measure the activity of almost each of them.
Blood clotting factors are produced in the liver and in the blood vessels themselves, and constantly circulate in the circulatory system in an inactive state. They are activated at the moment of damage to the vascular wall.
If the activity of a certain factor is low or insufficient, this can lead to serious clotting disorders, which is dangerous due to uncontrolled bleeding. If the factor activity is too high, it is dangerous due to excessive thrombus formation. Assessing the activity of blood coagulation factors allows a specialist to determine the cause of the defect and choose the appropriate treatment tactics.
When the tissue or wall of a vessel is damaged, the process of hemostasis starts, which stops bleeding, forming the so-called. plug at the site of damage. The platelets are directed to the damaged area, stick together and cover it. The blood coagulation cascade is activated.
As the cascade nears completion, soluble fibrinogen is transformed into insoluble fibrin strands. The threads are stitched together to form a fibrin mesh, which is secured to the damaged area.
This blood clot prevents unnecessary blood loss and remains at the site of injury until healing. Normally, in the human body there is a certain balance between the formation of blood clots and their timely dissolution. If the functional activity of one of the factors of the blood coagulation system is disturbed, the balance is also disturbed.
Blood clotting factors are designated by Roman numerals. Factor XII (Hageman factor) is produced in liver cells and is a plasma coagulation factor. It is activated by vascular damage and interacts with factor XI, triggering a further coagulation cascade.
Hageman factor deficiency manifests clinically as prolonged bleeding time. However, patients with this disease do not show a tendency to pathological, uncontrolled bleeding. Therefore, it is quite difficult to suspect a defect. As a rule, insufficient factor activity is discovered by chance.
Also, deficiency of factor XII may manifest itself as a tendency to increased thrombosis, because it is involved in the destruction of formed blood clots, regulating the conversion of inactive plasminogen into active plasmin. The latter dissolves the fibrin threads in the thrombus.
Insufficient activity of factor XII is diagnosed in thrombosis, thromboembolism, heart attack, spontaneous abortion. As a rule, the study is prescribed if a hereditary coagulation pathology is suspected, especially if episodes of prolonged bleeding begin at an early age or blood relatives have a confirmed factor XII deficiency.
Regulation of the coagulation system
Figure 6. Contribution of extrinsic and intrinsic tenase to fibrin clot formation in space. We used a mathematical model to investigate how far the influence of a clotting activator (tissue factor) could extend in space. To do this, we calculated the distribution of factor Xa (which determines the distribution of thrombin, which determines the distribution of fibrin). The animation shows the distributions of factor Xa produced by extrinsic tenase (VIIa–TF complex) or intrinsic tenase (IXa–VIIIa complex), as well as the total amount of factor Xa (shaded area). (The inset shows the same thing on a larger concentration scale.) It can be seen that activator-produced factor Xa cannot travel far from the activator due to the high rate of inhibition in the plasma. On the contrary, the IXa–VIIIa complex works far from the activator (since factor IXa is inhibited more slowly and therefore has a greater effective diffusion distance from the activator), and ensures the distribution of factor Xa in space.
[9]
Let's take the next logical step and try to answer the question - how does the system described above work?
Cascade device of the coagulation system
Let's start with the cascade - a chain of enzymes that activate each other. A single enzyme operating at a constant speed produces a linear dependence of product concentration on time. For a cascade of N enzymes, this dependence will have the form tN, where t is time. For the effective operation of the system, it is important that the response is of precisely this “explosive” nature, since this minimizes the period when the fibrin clot is still fragile.
Triggering of coagulation and the role of positive feedbacks
As mentioned in the first part of the article, many clotting reactions are slow. Thus, factors IXa and Xa themselves are very poor enzymes and require cofactors (factors VIIIa and Va, respectively) to function effectively. These cofactors are activated by thrombin, a device where the enzyme activates its own production is called a positive feedback loop.
As we have shown experimentally and theoretically, the positive feedback of factor V activation by thrombin forms the activation threshold - the property of the system not to respond to small activation, but to quickly respond when a large one appears. This ability to switch seems to be very valuable for folding: it helps prevent “false positives” of the system.
The role of the intrinsic pathway in the spatial dynamics of folding
One of the intriguing mysteries that haunted biochemists for many years after the discovery of the essential coagulation proteins was the role of factor XII in hemostasis. Its deficiency was detected in simple clotting tests, increasing the time required for clot formation, but, unlike factor XI deficiency, was not accompanied by coagulation disorders.
One of the most plausible options for unraveling the role of the internal pathway was proposed by us using spatially inhomogeneous experimental systems. Positive feedbacks have been found to be important specifically for the propagation of coagulation. Effective activation of factor X by external tenase on the activator will not help form a clot away from the activator, since factor Xa is rapidly inhibited in the plasma and cannot move far from the activator. But factor IXa, which is inhibited an order of magnitude slower, is quite capable of this (and is helped by factor VIIIa, which is activated by thrombin). And where it is difficult for him to reach, factor XI, also activated by thrombin, begins to work. Thus, the presence of positive feedback loops helps create the three-dimensional structure of the clot.
Protein C pathway as a possible localization mechanism for thrombus formation
Activation of protein C by thrombin itself is slow, but accelerates sharply when thrombin binds to the transmembrane protein thrombomodulin, synthesized by endothelial cells. Activated protein C is capable of destroying factors Va and VIIIa, slowing down the coagulation system by orders of magnitude. The key to understanding the role of this reaction was spatially inhomogeneous experimental approaches. Our experiments suggested that it stops the spatial growth of the thrombus, limiting its size.
References
- Zabolotskikh, I.B., Sinkov, S.V., Lebedinsky, K.M. Clinical guidelines “Perioperative management of patients with disorders of the homeostasis system”, 2021. - 42 p.
- Agibova, N.E., Boeva, O.I., Baykulova, M.Kh. and others. Hageman factor in predicting the risk of thromboembolic complications in atrial fibrillation. — Cardiovascular therapy and prevention, 201. — No. 8. — P.26-27.
- Chaudhry, L., El-Sadek, W., Chaudhry, G. et al. Factor XII (Hageman factor) deficiency: a rare harbinger of life threatening complications. — The Pan African medical journal, 2021. — Vol. 33(39).
Summarizing
In recent years, the complexity of the coagulation system has gradually become less mysterious. The discovery of all essential components of the system, the development of mathematical models and the use of new experimental approaches made it possible to lift the veil of secrecy. The structure of the coagulation cascade is being deciphered, and now, as we saw above, for almost every significant part of the system, the role it plays in the regulation of the entire process has been identified or proposed.
Figure 7 shows the most recent attempt to reconsider the structure of the coagulation system. This is the same diagram as in Fig. 1, where parts of the system responsible for different tasks are highlighted with multi-colored shading, as discussed above. Not everything in this scheme is securely established. For example, our theoretical prediction that activation of factor VII by factor Xa allows clotting to respond in a threshold manner to flow rate remains as yet untested experimentally.
Figure 7. Modular structure of the coagulation system: the role of individual coagulation reactions in the functioning of the system.
[1]
It is quite possible that this picture is not yet completely complete. However, progress in this field in recent years gives hope that in the foreseeable future, the remaining unsolved regions of the coagulation circuitry will gain meaningful physiological function. And then it will be possible to talk about the birth of a new concept of blood coagulation, which replaced the old cascade model, which faithfully served medicine for many decades.
The article was written with the participation of A.N. Balandina and F.I. Ataullakhanova and was originally published in Priroda [10].
Vitamin K
Vitamin K was discovered by the Danish researcher Henrik Dam in the course of research from 1929 to 1935, who received the Nobel Prize in 1943 together with the American researcher Edward Doisy for the discovery and study of the properties of vitamin K. Dam studied the metabolism of cholesterol and to determine the effect of nutrition on the synthesis of cholesterol in organism conducted experiments on chickens that were given a special low-fat diet. Chickens became ill with an unknown disease if this diet continued for more than 2-3 weeks. They experienced multiple hemorrhages under the skin, in the muscles and internal organs, and the blood clotted very slowly. The disease arose as a result of a lack of an unknown chemical substance that did not coincide with any of the vitamins known at that time. As Dahm himself recounted in his Nobel lecture, it was named vitamin K after the German-Scandinavian word Koagulation (coagulation) and was the first vitamin named from a non-English word.
Vitamin K includes a group of fat-soluble vitamins that are necessary for the post-translational modification of several proteins, most of which are proteins of the blood coagulation and anticoagulation system. Chemically, they belong to the derivatives of 2-methyl-1, 4 naphthoquinolone.
All members of the vitamin K family have a methylated naphthoquinolone ring and a side chain containing varying numbers of isoprene residues. Phylloquinolone (vitamin K1) has 4 isoprene residues in its side chain, one of which is unsaturated. Menaquinolones (vitamin K2) contain varying amounts of unsaturated isoprene residues. They are usually designated as MK-n, where n is the number of spoilen residues. The presence of isoprene residues brings vitamins K closer to other fat-soluble vitamins (A, E and ubiquinolones (coenzymes Q)). Vitamins K1 and K2 are the only naturally occurring vitamin Ks. The remaining vitamins K (K3, K4, etc.) are synthetic.
Vitamin K1 is found in green vegetables (spinach, lettuce, cauliflower, cereals, avocados, kiwi, bananas, meat, dairy products, eggs, soybeans, vegetable oils, in particular olive oil. Vitamin K2 is synthesized by intestinal bacteria, therefore vitamin deficiency vitamin K in adults is a rare occurrence, mainly in dysbiosis after treatment with antibiotics. However, in young children, whose intestines are not yet populated with bacteria in sufficient quantities, hypovitaminosis K is often observed, which can lead to bleeding. Vitamin K does not penetrate placenta.
As stated above, vitamin K is required for the carboxylation of glutamic acid residues in some proteins, which are converted to gamma-carboxyglutamic acid (Gla) residues. Proteins that undergo such post-translational modification are called Gla proteins.
There are 14 known Gla proteins in humans:
- Blood clotting proteins: prothrombin (factor II), factors VII, IX, X, proteins C, S and Z
- Bone metabolic proteins: osteocalcin (synonym: bone Gla protein, BGP) matrix Gla protein (MGP)
- Participation in vascular repair (angiogenesis)
Practical recommendations based on the results of testing for polymorphism of factor VII Arg353Gln (R353Q)
- Testing for polymorphism R353Q is an important part of testing for polymorphism of genes of the hemostasis system. A risk factor that increases the likelihood of pregnancy complications is the more common R variant. The Q polymorphic variant reduces the risk of developing thrombotic complications of pregnancy.
- In the presence of variant R, additional risk factors for elevated factor VII concentrations include high triglyceride levels, excess body weight, and use of hormonal contraceptives and hormone replacement therapy. Therefore, an important addition to the study is to determine the patient’s lipid profile, including triglycerides in the set of indicators. The lipid panel in such cases should consist of total cholesterol, low-density lipoproteins, high-density lipoproteins and triglycerides. It is also important to determine glucose levels and conduct a sugar curve. It is mandatory to calculate the patient's body mass index.
- The recommendations must necessarily include recommendations on a diet aimed at reducing the consumption of animal fats and carbohydrates by including oleic and palmitic acids (omega-3 acids) in the diet. Moderate physical activity under the supervision of a specialist in physical therapy is desirable as part of a set of measures to combat excess body weight.
- It should be remembered that the protective variant Q can be combined with such risk factors for thrombophilia as the Leiden mutation, homozygous form 4G/4G of the PAI-1 mutation, etc., which may require the prescription of hypocoagulant therapy consisting of low-dose acetylsalicylic acid and heparin preparations. The relative deficiency of factor VII in such patients may lead to an increased risk of bleeding during anticoagulation.
- Since the intrauterine fetus inherits one copy of the gene from the father and the other from the mother, and some pregnancy complications are associated not only with the genotype of the mother, but also with the genotype of the intrauterine fetus (the development of thrombosis in the fetus), in some cases it is necessary to examine the husband for polymorphisms of the system genes hemostasis in order to calculate the risks of recurrence of the situation during the next pregnancy and develop adequate tactics for preparing for pregnancy.
What is Rh factor
By the middle of the 20th century, scientists received confirmation that the compatibility of people according to the immunological characteristics of blood is not limited to the classical division into four blood groups. A protein was discovered that is present in the blood of approximately 85% of people. Accordingly, approximately 15% of people do not have it. When blood is transfused from the first to the second, the recipient’s body begins to produce antibodies to this protein, that is, this substance is an antigen. In medicine, this protein is designated by the Latin letter D. If protein D is in your blood, it means that you have a positive Rh factor (Rh+)
, and you belong to the majority (85%).
If this antigen is not in your blood, your Rh factor is negative (Rh-)
. The Rh factor does not change throughout life.
Why is the Rh factor important in blood transfusions?
When blood is transfused from a person with Rh+ to a person with Rh-, a conflict occurs regarding the Rh factor
. But if, in the case of a conflict regarding the blood group, the destruction of red blood cells (hemolysis) begins immediately, then in the case of a conflict regarding the Rh factor, there is no hemolysis during the first transfusion. The first contact with antigen D only leads to sensitization of the recipient, that is, his body produces specific antibodies, and sensitivity to the antigen increases. But if the antigen enters the blood of a person with a negative Rh factor again, the body begins to react to the penetration of a foreign agent: red blood cells begin to stick together inside the vessels and destroy. A person feels tightness in the chest, difficulty breathing, pain in the lumbar region. Blood pressure decreases and acute renal failure develops. This complex of symptoms is called hemolytic shock.
Currently, hemolytic shock from blood transfusion is practically excluded. In today's medical practice, blood that matches the recipient's blood group and Rh factor is used for transfusion. In order to eliminate errors, before any operation, the analysis to determine the blood group and Rh factor is done again.