The most common diagnostic procedure that is performed when visiting a doctor of any specialization is a blood test. It is the blood that reacts very quickly to any changes occurring in the body. By changes in its composition, inflammatory processes can be detected, serious diseases can be suspected and identified at an early stage.
Using a general blood test, the number of formed elements (leukocytes, red blood cells, platelets) is determined and, based on a comparison of the results obtained with existing standards, conclusions are drawn about the state of health.
The PLT blood test is a test for platelet levels. This indicator is one of the main ones and is of great importance in laboratory diagnostics.
What are platelets?
These elements are formed in the bone marrow and are small, round, irregularly shaped plates that lack nuclei. The function of these particles is very important: they are involved in the process of blood clotting and regeneration of damaged tissue, that is, they help prevent large blood losses in the event of vascular damage. The cells live for no more than 10 days, after which they are destroyed in the spleen and liver, and they are replaced by new ones.
The platelet count changes throughout the day. They are increased during physical activity. During pregnancy and menstruation, their number, on the contrary, decreases. Such changes are considered natural, and platelet levels return to normal at rest, at the end of menstruation, or after childbirth.
In other cases, deviations from the norm in any direction indicate some kind of pathology. A condition in which platelets are elevated is called thrombocytosis, and if they are low, it is called thrombocytopenia.
Restoring platelet levels in the blood
You can normalize the level of platelets in the blood with a balanced diet. It is important to saturate your diet with foods high in materials and microelements. You need to give up spicy food, alcohol, fast food and sweet carbonated drinks, lead a healthy lifestyle and maintain a drinking regime.
If it is not possible to normalize the indicators using natural methods, then you need to undergo a full examination by a hematologist. If platelet levels are elevated, special medications may be prescribed - anticoagulants or antiplatelet agents. They thin the blood and minimize the risk of blood clots. But at the same time, they should be taken only as prescribed by a doctor. It should be understood that stabilization of the condition is possible only after eliminating the underlying causes that provoke deviations from the norm.
Interpretation of the blood test on PLT
Decoding the analysis is within the competence of the attending physician. Thrombocytosis or thrombocytopenia may be the first signs of various pathologies.
The platelet level is determined during a general blood test
If the level of platelets in the blood exceeds normal values, the development of the following diseases can be assumed:
- Blood poisoning.
- Lymphogranulomatosis.
- Stomach cancer.
- Malignant blood diseases.
- Consequences of severe blood loss.
- Consequences of surgery to remove the spleen (thrombocytosis persists for two months).
- Chronic diseases: colitis, tuberculosis, rheumatoid arthritis and others.
Thrombocytopenia may indicate the following pathological conditions:
- Leukemia (chronic and acute).
- Werlhof's disease, or thrombocytopenic purpura.
- Systemic connective tissue diseases: scleroderma, lupus erythematosus, dermatomyositis.
- Folate deficiency anemia.
- Increased activity of the spleen in hepatitis (chronic, viral), liver cirrhosis.
- Taking certain medications.
- Viral infections: influenza, rubella, chickenpox, measles.
- Endocrine diseases: hypothyroidism, thyrotoxicosis.
- Metastases in the bone marrow in cancer.
- Aplastic and hypoplastic conditions of unknown origin, in which there is a decrease in platelet formation in the bone marrow.
Consequences of low platelet count
In a state of low platelet count, disorders subsequently develop, which include frequent bleeding (menstrual and nosebleeds), while the bleeding time increases significantly and becomes difficult to stop. Sudden gum bleeding may develop (not everyone does). Blood clots may be found in urine or stool. Petechiae (red dots resulting from damage to the capillary wall) appear on the skin of the lower extremities, most often the legs. Even minimal damage leads to the formation of ecchymoses (bruises), when normally a bruise would not appear.
The severity of symptoms directly depends on the platelet count. The fewer platelets, the more severe the clinic. If the platelet count is very low, internal bleeding into the digestive tract or even bleeding into the brain may occur.
Even in the presence of a mild clinic, it is recommended to consult a general practitioner in order to prevent this condition.
Testing for PLT in children
Monitoring blood composition, including PLT levels, is especially important in childhood. If this indicator drops below normal, the following diseases can be assumed:
- allergic reactions to medications;
- intoxication;
- thyrotoxicosis;
- blood diseases;
- parasitic and viral infections.
The causes of elevated PLT levels in children are varied. There are primary and secondary thrombocytosis. The first is due to the fact that brain stem cells produce an excess amount of platelets with an altered structure, which, for example, is observed in leukemia.
Secondary, or reactive, develops as a result of some pathological process, which disrupts the production of these cells, as well as their structure and shape. Factors in the development of reactive thrombocytosis include:
- heavy operations;
- splenectomy;
- sudden bleeding;
- osteomyelitis;
- anemia;
- fractures of tubular bones;
- pulmonary infections;
- malignant diseases;
- some drugs.
Video about the functions of platelets and the reasons for changes in their number in the blood:
General information
Platelets are granulocytic blood cells without a biconvex nucleus, formed from plasma cells of the bone marrow. They are presented in different forms - young, adult and mature. The diameter is directly proportional to age: 2-4 microns. Platelets contain granules that create blood clotting proteins, lytic enzymes, phosphatase and cathepsin, create serotonin, calcium ions and ATP, and contain lysosomal enzymes.
One of the most important functions of blood platelets is participation in blood clotting (primary hemostasis).
Platelets bind clotting factors, making blood clots thicker. As a rule, in an inactive state, when the vessel wall is damaged, platelets are directed to the damaged area. Thanks to the pseudopods located on the surface of the body, they are attached to each other and the vascular wall, forming a blood clot, which is an excellent barrier to bleeding. In the active state, platelets are able to change the shape of the body, due to which they increase their area, and this allows them to completely close the damage.
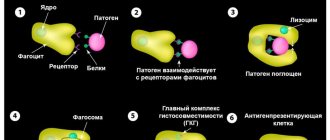
In addition, platelets are able to protect the body from foreign bodies by catching them with the help of pseudopods, and then digesting them with the help of the enzyme lysocine, which is formed from platelet factors (thrombin, thromboxane), from platelet granules. Thus, platelets are important for the immune response, being “killer” cells for foreign agents entering the body.
Blood plates serve as a storage site for serotonin, providing antitumor and radioprotective effects.
Thus, a violation of the number of platelets leads to inhibition of their functions, this certainly leads to disruption of the body’s activity and entails negative symptoms.
Prevention
Preventive measures are extremely simple. It is enough to follow simple recommendations:
- Regularly undergo inspections. Every six months or a little less often.
- Eat well. To prevent the development of anemia and deficiency diseases.
- Treat pathologies of any profile in a timely manner. Even an old source of infection can present an unpleasant surprise.
- Eliminate alcohol from your life.
- Do not self-medicate.
PLT stands for platelet, which means platelets in English. The indicator is informative, but it needs to be clarified by other methods. This way you can quickly detect health problems.
Reasons for the decline
{banner_banstat10}
A similar condition occurs no less often. Among the development factors.
Hepatitis
Inflammatory liver damage. Accompanied by acute dysfunction of the organ. In the chronic phase it is not so dangerous.
Among the symptoms:
- Pain in the right side of the abdomen.
- Nausea.
- Vomit.
- Change in color of stool.
- Diarrhea, constipation.
- Digestive disorders.
- Bitter taste in the mouth.
- Increased body temperature (not always).
The disease is progressing. Not at the same speed, but steadily. If nothing is done, necrotic changes will begin.
The condition is corrected under the supervision of a hepatologist. When such a narrow specialist is not available, a gastroenterologist is involved. The goal is to slow down, and ideally stop, change altogether. Protective drugs are prescribed.
Be sure to prescribe a gentle diet low in animal fat. If hepatitis is of infectious origin, you cannot do without special antiviral medications.
The prognosis for systematic treatment is positive, PLT concentration will recover quickly.
Cirrhosis of the liver
Necrotic process. Characterized by the death of organ tissue. In the acute phase, days and even hours count. It is necessary to transport the patient to the hospital. Then carry out urgent correction.
The clinical picture corresponds to that of hepatitis, only more severe. Problems begin with the nervous system and hematopoietic structures.
Among the manifestations:
- Pain in the right side.
- Impaired consciousness.
- Nausea.
- Vomit.
- Decline in cognitive level and intellectual abilities.
- Discoloration of stool.
- Diarrhea or constipation.
- Bleeding.
- The formation of spider veins on the body.
Chronic forms allow more time for treatment. Therapy consists of using protectors. We must do everything we can to stop the progression of the disease.
At the initial and middle stages of the pathological process, there is a chance of a liver transplant. The operation can only be successful during these periods.
In the decompensated stage, transplantation will make little sense. Bleeding begins and surgery is no longer possible. The disease is serious and must be dealt with quickly.
PLT decreases because cells die and new ones are not produced in sufficient quantities.
Thyroid disorders
Pathologies in which too much hormones T3 and T4 are synthesized. The lifespan of platelets in this case is significantly reduced. Hematopoiesis slows down. This is the reason for the deficiency of red PLT plates.
Pathology is treated under the supervision of an endocrinologist. The task is not quick, it takes several months. Iodine preparations are prescribed, as well as a diet low in this element.
Radiation sickness
As such, it inhibits the normal functioning of the bone marrow. This just ends with insufficiently rapid platelet maturation.
Attention:
The same is possible with a systematic, but weak influence of radiation. For example, when performing X-rays, CT scans too often.
Indications for the study
Adults should be attentive to small children. They cannot always explain their unusual symptoms on their own.
That is why adults should immediately seek advice from a pediatrician if their child suddenly develops the following undesirable symptoms:
- constant bleeding gums;
- frequent nosebleeds;
- bruises on the body that appear for unknown reasons;
- frequent numbness of the limbs;
- general weakness;
- frequent complaints of headache and dizziness.
Treatment
Regarding symptomatic correction:
With elevated platelets
It is necessary to eliminate the primary cause of the pathological process. These are the diseases that were described earlier. There is no need to fight the platelets themselves. The task is to remove the primary factor. It is better to address this question to a specialized specialist.
Symptomatic correction is to prevent the formation of blood clots. Anticoagulants or antiplatelet agents are prescribed.
At low
The same. Etiotropic treatment is necessary. Fighting the primary cause.
Additional examinations
Ancillary measures are aimed at establishing the origin of the pathology.
Among the techniques:
- Oral interview with the patient.
- Anamnesis collection.
- Ultrasound of the digestive tract.
- MRI as needed.
- Blood and urine tests: general, biochemical. For hormones.
- Coagulogram.
This is a basic diagnostic checklist. Based on its results, specialized examinations are prescribed at the discretion of the doctor.
Tables of norms by age
The abbreviation PLT (short for platelets) in a general blood test refers to platelets.
The rate of red plates, regardless of gender, is highest in the first days after birth and steadily decreases with age.
Among women
| Age | Indicator in thousands U/μl |
| Up to 17 | 160-382 |
| 17-25 | 170-380 |
| 26-36 | 175-400 |
| 37-60 | 170-350 |
| 60 years and older | 175-310 |
The PLT norm in women is in the range of 160-400 thousand units/μl of blood and may vary slightly during one age interval, deviating from the presented calculations.
In men
| Age (years) | Norm in thousands of units per µl |
| Up to 17 | 175-380 |
| 17-25 | 175-390 |
| 26-36 | 185-400 |
| 37-60 | 190-395 |
| 60+ | 175-370 |
In children
| Age | PLT level thousand units/µl |
| Newborns | 180-490 |
| First month | 185-400 |
| Up to a year | 180-400 |
| 1-2 years | 155-390 |
| 2-3 years | 160-385 |
| 3-10 years | 160-380 |
During pregnancy
| Trimester | Normal value (thousand units/μl) |
| I | 170-340 |
| II | 155-321 |
| III | 145-310 |
The PLT norm in a blood test is a dynamic level, we are talking about ranges from 145 to 490 thousand units/μl of blood. Natural factors can also affect the results: physical activity, stress, habits. Also past illnesses. This needs to be taken into account.
table 2
| Index | x 109/l | % |
| Band neutrophils | 0,04-0,3 | 1-6 |
| Segmented neutrophils | 2-5,5 | 45-72 |
| Basophils | up to 0.065 | up to 1 |
| Eosinophils | 0,02-0,3 | 0,5-5 |
| Lymphocytes | 1,2-3 | 19-37 |
| Monocytes | 0,09-0,6 | 3-11 |
The results of a general blood test (Table 1) show many indicators. Let's consider the main ones:
- RBC – total number of red blood cells (erythrocytes). The pathological increase in these cells is associated with impaired hematopoiesis. A decrease in red blood cells is usually a consequence of anemia, hemolysis and blood loss.
- HGB stands for hemoglobin, which is a protein containing iron. It transports oxygen to tissues, and carbon dioxide from them, and also maintains acid-base balance. A decrease in hemoglobin most often occurs due to anemia.
- HCT – hematocrit. It is defined as the ratio between the red blood cells that have settled to the bottom after taking the test and the total blood volume. An increase in this indicator indicates polyuria, erythrocytosis or erythremia. A decrease in hematocrit level occurs with anemia and an increase in circulating blood volume.
- PLT – platelets. These cells are responsible for blood clotting. If their number decreases, then the cause may be viral diseases, bone marrow lesions, bacterial infections and other pathologies. An increase in the number of platelets is caused by a wide variety of ailments: from joint diseases to cancer.
- CPU – color indicator. It determines the saturation of red blood cells with hemoglobin. If it is insufficient, this may indicate iron deficiency anemia, anemia or lead poisoning. When CP rises above normal, the cause is oncology, gastric polyposis and deficiency of vitamins B9 and B12.
- Erythrocyte indices: MCV - average volume of erythrocytes, used to determine water-salt balance and type of anemia;
- RDW is the degree of red blood cell diversity, which determines how different cells differ from each other in volume;
- MCH – average hemoglobin content in erythrocyte; this criterion is considered analogous to the color indicator;
- MCHC – average concentration and content of hemoglobin in red blood cells; this indicator is calculated taking into account the level of hematocrit and hemoglobin.
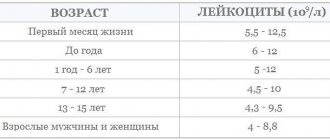
Now let's move on to the leukocyte formula (Table 2). It determines the percentage of different types of white blood cells in the blood, that is, the relative content of each type of white cell. What is this formula for? It is very important because with any changes in the body, the percentage of certain types of white cells in the blood decreases or increases. This is associated with a decrease or increase in other types. Based on the information obtained from the leukocyte formula, one can judge the course of a particular pathology, the occurrence of complications, and also more accurately predict the outcome of the disease.