Instructions for use
Before using the medication, you must study the rules of administration and the dosage recommended by experts.
Indications for use
You should use this drug if you have the following ailments:
- Hepatitis;
- Food allergies;
- Fatty liver degeneration;
- Liver damage due to medications;
- Poisoning;
- Disturbances in the digestive system;
- Discomfort and pain in the abdomen;
- Weakness, dizziness and feeling of nausea.
Mode of application
The medicine is intended for intramuscular or intravenous jet administration. The drug is introduced into the body very slowly and carefully.
Sirepar actively works against pathogens and improves liver function. Before starting the procedure, the product must be diluted with the patient’s own blood, or with a 0.9% sodium chloride solution.
The solution cannot be diluted with water, otherwise it will lose its healing properties and its effectiveness will decrease several times. This can lead to allergic reactions and unpleasant consequences.
First, to establish possible hypersensitivity, it is necessary to inject 0.1–0.2 ml of solution intramuscularly deeply, then monitor for thirty minutes. If no signs of an allergic reaction are noticed, you can use the drug in the prescribed doses.
For adults, the daily dose is 2-8 ml, the course dose reaches 150-200 ml . Children from one year to fourteen years are recommended to take 1 to 3 ml of medication per day for two to six weeks.
Experts recommend starting to take the product at 0.1-0.2 ml. Gradually the dosage increases to 0.5. You cannot use a lot of the drug from the first days. The body must prepare for it to avoid complications.
It must be remembered that the exact dosage, as well as the duration of taking the drug, is determined by the doctor. These factors depend on the patient’s well-being, disease, and characteristics of the body. During the recovery period, the dosage may be slightly reduced.
The drug must be taken under the supervision of a doctor so as not to cause harm.
Release form, composition
The medication is prepared in the form of an injection solution. The solution is placed in 10 ml bottles. There are five bottles in one package of the drug. Ingredients: Liver extract hydrolyzate containing cyanocobalamin.
The component has a beneficial, but at the same time, gentle effect on the human body without causing complications.
If side effects occur, the patient should stop taking this drug and consult with their doctor.
Interaction with other drugs
Data on the interaction of Sirepar with other drugs are not provided. It is not recommended to take risks and take several medications at once. Side effects may occur. If taking multiple medications is unavoidable, you should consult your doctor.
Triplixam®
All precautions associated with taking individual components of the drug should be taken into account when using their fixed combination as part of the drug Triplixam®.
Amlodipine
Chronic heart failure
Patients with chronic heart failure should be treated with caution.
When using amlodipine in patients with chronic heart failure of functional class III and IV according to the NYHA classification, pulmonary edema may develop. Slow calcium channel blockers, including amlodipine, should be used with caution in patients with chronic heart failure due to a possible increased risk of cardiovascular adverse events and mortality.
In patients with severe chronic heart failure (NYHA functional class IV), treatment should begin with lower doses and under close medical supervision.
Patients with arterial hypertension and coronary heart disease should not stop taking beta-blockers: an ACE inhibitor should be used in conjunction with beta-blockers.
Hypertensive crisis
The effectiveness and safety of amlodipine in hypertensive crisis has not been established.
Indapamide
Hepatic encephalopathy
In the presence of liver dysfunction, taking thiazide and thiazide-like diuretics can lead to the development of hepatic encephalopathy. In this case, you should immediately stop taking the diuretic.
Photosensitivity
Cases of photosensitivity reactions have been reported while taking thiazide and thiazide-like diuretics (see section "Side effects"). If a photosensitivity reaction develops while taking the drug, treatment should be discontinued. If it is necessary to continue diuretic therapy, it is recommended to protect the skin from exposure to sunlight or artificial ultraviolet rays.
Content of calcium ions in blood plasma
Thiazide and thiazide-like diuretics can reduce the excretion of calcium ions by the kidneys and lead to a slight and temporary increase in the content of calcium ions in the blood plasma. Severe hypercalcemia may be a consequence of previously undiagnosed hyperparathyroidism. In such cases, you should stop taking diuretics and conduct a study of the function of the parathyroid glands (see section “Side effects”).
Uric acid
In patients with elevated concentrations of uric acid in the blood plasma, the frequency of gout attacks may increase during therapy.
Perindopril
Potassium-sparing diuretics, potassium supplements, potassium-containing table salt substitutes and food supplements
The simultaneous administration of perindopril and potassium-sparing diuretics, as well as potassium preparations, potassium-containing table salt substitutes and food additives is not recommended (see section “Interaction with other drugs”). Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
There is evidence of an increased risk of arterial hypotension, hyperkalemia and renal dysfunction (including acute renal failure) when ACE inhibitors are used simultaneously with ARB II or aliskiren. Therefore, double blockade of the RAAS as a result of combining an ACE inhibitor with ARA II or aliskiren is not recommended (see sections “Interaction with other drugs” and “Pharmacodynamics”). If a double blockade is necessary, it should be performed under the strict supervision of a specialist with regular monitoring of renal function, plasma electrolyte levels and blood pressure.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Neutropenia/agranulocytosis/thrombocytopenia/anemia
There are reports of the development of neutropenia/agranulocytosis, thrombocytopenia and anemia while taking ACE inhibitors. In patients with normal renal function and in the absence of other aggravating factors, neutropenia rarely develops. Perindopril should be used with extreme caution in patients with systemic connective tissue diseases, while taking immunosuppressants, allopurinol or procainamide, or their combination, especially in patients with impaired renal function.
Some of these patients developed severe infections, in some cases resistant to intensive antibiotic therapy. When prescribing perindopril to such patients, it is recommended to periodically monitor white blood cells in the blood, and patients should report to the doctor any signs of infectious diseases (for example, sore throat, fever) (see section "Side effects").
Renovascular hypertension
In patients with bilateral renal artery stenosis or arterial stenosis of a single functioning kidney during therapy with ACE inhibitors, the risk of developing arterial hypotension and renal failure increases (see section “Contraindications”). The use of diuretics may be an additional risk factor. Deterioration of renal function can be observed with even a slight change in serum creatinine concentration, even in patients with unilateral renal artery stenosis.
Hypersensitivity/angioedema
When taking ACE inhibitors, including perindopril, in rare cases, the development of angioedema of the face, extremities, lips, tongue, glottis and/or larynx may occur. This can happen at any time during therapy. If symptoms appear, the drug should be stopped immediately and the patient should be observed until signs of edema completely disappear. If the swelling affects only the face and lips, it usually resolves on its own, although antihistamines may be used to treat symptoms.
Angioedema, accompanied by swelling of the larynx, can be fatal. Swelling of the tongue, glottis or larynx can lead to airway obstruction, in which case intensive care should be given immediately. If such symptoms appear, you should immediately administer a solution of epinephrine (adrenaline) 1:1000 (0.3-0.5 ml) and/or ensure airway patency. The patient should be under medical supervision until symptoms disappear completely and permanently.
Patients of the Black race had a higher incidence of angioedema while taking ACE inhibitors compared to other races.
Patients with a history of angioedema not associated with taking ACE inhibitors may have an increased risk of developing it when taking the drug (see section "Contraindications"). There are reports of rare cases of the development of angioedema of the intestine during therapy with ACE inhibitors. In this case, patients experienced abdominal pain as an isolated symptom or in combination with nausea and vomiting, in some cases without previous angioedema of the face and with normal levels of C1-esterase. The diagnosis was made using abdominal computed tomography, ultrasound, or at the time of surgery. Symptoms resolved after discontinuation of ACE inhibitors. Therefore, in patients with abdominal pain receiving ACE inhibitors. When carrying out differential diagnosis, it is necessary to take into account the possibility of developing angioedema of the intestine.
Combined use with the combination of valsartan + sacubitril
Due to the increased risk of developing angioedema (see section “Contraindications”), simultaneous use of perindopril with the combination of valsartan + sacubitril is contraindicated. The use of the combination of valsartan + sacubitril is possible no earlier than 36 hours after taking the last dose of perindopril. If therapy with the valsartan + sacubitril combination is discontinued, the use of perindopril should not be started earlier than 36 hours after taking the last dose of the valsartan + sacubitril combination (see sections “Contraindications” and “Interaction with other drugs”). When taking ACE inhibitors concomitantly with other enkephalinase inhibitors (for example, racecadotril), the risk of developing angioedema may be increased (see section "Interaction with other drugs"). In patients receiving perindopril, a careful risk/benefit assessment should be performed before prescribing enkephalinase inhibitors (eg racecadotril).
Concomitant use with mTOR inhibitors (for example, sirolimus, everolimus, temsirolimus)
Concomitant use of an ACE inhibitor and an mTOR inhibitor (eg, sirolimus, everolimus, temsirolimus) may be associated with an increased risk of angioedema (eg, swelling of the airways or tongue, with or without impairment of respiratory function) (see Interactions with Other Drugs section) ).
Anaphylactoid reactions during desensitization
There are isolated reports of the development of prolonged, life-threatening anaphylactoid reactions in patients receiving ACE inhibitors during desensitizing therapy with hymenoptera venom (bees, wasps). ACE inhibitors should be used with caution in patients with a history of allergies or a tendency to allergic reactions undergoing desensitization procedures, and the use of an ACE inhibitor should be avoided in patients receiving immunotherapy with hymenoptera venom. However, an anaphylactoid reaction can be avoided by temporarily discontinuing the ACE inhibitor at least 24 hours before the start of the desensitization procedure.
Anaphylactoid reactions during LDL apheresis
In rare cases, life-threatening anaphylactoid reactions may occur in patients receiving ACE inhibitors during LDL apheresis using dextran sulfate. To prevent an anaphylactoid reaction, ACE inhibitor therapy should be temporarily discontinued before each apheresis procedure.
Hemodialysis
Anaphylactoid reactions have been reported in patients receiving ACE inhibitors during hemodialysis using high-flux membranes (eg, AN69®). Therefore, it is advisable to use a different type of membrane or use an antihypertensive agent of a different pharmacotherapeutic group.
Primary hyperaldosteronism
Patients with primary hyperaldosteronism are usually not susceptible to antihypertensive drugs whose action is based on inhibition of the renin-angiotensin system. Therefore, the use of this drug in such patients is not recommended.
Pregnancy
Taking ACE inhibitors during pregnancy is contraindicated. If continued therapy with ACE inhibitors is necessary, patients should switch to other types of antihypertensive therapy with an established safety profile when taken during pregnancy. If pregnancy occurs, ACE inhibitors should be stopped immediately and, if necessary, alternative antihypertensive therapy should be started (see sections “Contraindications” and “Use during pregnancy and lactation”).
Cough
During therapy with an ACE inhibitor, a dry cough may occur. The cough persists for a long time while taking drugs of this group and disappears after their discontinuation. If a patient develops a dry cough, one should be aware of the possible iatrogenic nature of this symptom. If the physician believes that ACE inhibitor therapy is necessary for the patient, continuing the drug may be considered.
Mitral stenosis/aortic stenosis/hypertrophic obstructive cardiomyopathy ACE inhibitors should be prescribed with caution to patients with left ventricular outflow tract obstruction.
Ethnic differences
Perindopril, like other ACE inhibitors. obviously has a less pronounced hypotensive effect in patients of the Negroid race compared to representatives of other races. This difference may be due to the fact that black patients with arterial hypertension are more likely to have low renin activity.
Surgery/General anesthesia
The use of ACE inhibitors in patients undergoing surgery under general anesthesia can lead to a significant decrease in blood pressure, especially when using general anesthetic agents that have an antihypertensive effect.
It is recommended, if possible, to stop taking long-acting ACE inhibitors, including perindopril, one day before surgery.
Patients with renovascular hypertension
The treatment method for renovascular hypertension is revascularization. However, the use of ACE inhibitors has a beneficial effect in patients both awaiting surgery and in cases where surgery is not possible.
When using the drug Triplixam® in patients with existing or suspected renal artery stenosis, treatment should begin in a hospital setting with low doses with constant monitoring of the condition of the kidneys and potassium levels in the blood, since such patients may develop functional renal failure, which disappears with cessation of therapy.
Atherosclerosis
The risk of arterial hypotension exists in all patients, however, special care should be taken when using the drug in patients with coronary heart disease and cerebrovascular insufficiency. In such patients, treatment should begin with low doses of the drug.
Perindopril/Indapamide
Lithium preparations
The simultaneous use of a combination of perindopril and indapamide with lithium preparations is not recommended (see section “Interaction with other drugs”).
Arterial hypotension and water-electrolyte imbalance
The presence of initial hyponatremia is associated with the risk of sudden development of arterial hypotension (especially in patients with renal artery stenosis). Therefore, clinical signs of dehydration and decreased plasma electrolytes, such as after diarrhea or vomiting, should be systematically assessed. Such patients require regular monitoring of blood plasma electrolyte levels.
In case of severe arterial hypotension, intravenous administration of 0.9% sodium chloride solution may be required.
Transient arterial hypotension is not a contraindication for continued therapy. After restoration of blood volume and blood pressure, therapy can be resumed using low doses of the combination, or the components of the drug can be used as monotherapy.
Hyponatremia at the initial stage may not be accompanied by clinical symptoms, so regular laboratory monitoring is necessary. More frequent monitoring of sodium ion levels is indicated for elderly patients and patients with liver cirrhosis (see sections “Side effects” and “Overdose”).
Therapy with any diuretic drugs can cause hyponatremia, sometimes with very serious consequences.
Hyponatremia with hypovolemia can cause dehydration and orthostatic hypotension. The simultaneous loss of chlorine ions can lead to secondary
compensatory metabolic alkalosis: the frequency and extent of this effect are insignificant.
Patients with diabetes mellitus
In patients with type 1 diabetes mellitus (risk of spontaneous increases in potassium ions), treatment should begin with lower doses and under close medical supervision.
When prescribing the drug to patients with diabetes mellitus receiving oral hypoglycemic agents or insulin, regular monitoring of plasma glucose concentrations is necessary during the first month of therapy. It is necessary to monitor blood glucose levels in patients with diabetes mellitus, especially in the presence of hypokalemia.
Amlodipine/Perindopril
Liver failure
In rare cases, cholestatic jaundice occurs while taking ACE inhibitors. As this syndrome progresses, fulminant liver necrosis develops, sometimes with death. The mechanism of development of this syndrome is unclear. When jaundice or a significant increase in the activity of liver enzymes occurs in patients taking ACE inhibitors. you should stop taking the ACE inhibitor and consult a doctor (see section “Side effects”),
In patients with impaired liver function, T1/2 and AUC of amlodipine are increased. Amlodipine should be started with the lowest doses and precautions should be taken both at the beginning of treatment and when increasing the dose. In patients with severe hepatic impairment, the dose should be increased gradually, ensuring careful monitoring of the clinical condition.
Triplixam® has not been studied in patients with liver failure. Considering the effect of each component included in the drug separately, Triplixam® is contraindicated in patients with severe liver failure, and also requires special caution when prescribed to patients with moderate and mild liver failure.
Amlodipine/Indapamide/Perindopril
Renal dysfunction
The drug is contraindicated in patients with severe renal impairment (creatinine clearance less than 30 ml/min) (see section "Contraindications").
In patients with moderate renal impairment (creatinine clearance 30-60 ml/min), the use of Triplixam® in dosages containing 10 mg of perindopril and 2.5 mg of indapamide is contraindicated (i.e., dosage of Triplixam® 5 mg + 2.5 mg + 10 mg and 10 mg + 2.5 mg + 10 mg).
Some patients with arterial hypertension without previous obvious renal impairment may develop laboratory signs of functional renal failure during therapy. In this case, treatment with the drug should be stopped with the further possibility of resuming combination therapy using low doses of the drug, or using the components of the drug in monotherapy.
Such patients require regular monitoring of the content of potassium ions and creatinine in the blood serum - 2 weeks after the start of therapy and then every 2 months. Renal failure occurs more often in patients with severe chronic heart failure or underlying renal dysfunction, including renal artery stenosis.
Triplixam® is not recommended for patients with bilateral renal artery stenosis or stenosis of the artery of a single functioning kidney.
There is a risk of arterial hypotension and/or renal failure (in the presence of chronic heart failure, dehydration and decreased electrolyte levels in the blood plasma, etc.): in some pathological conditions, significant activation of the RAAS may be observed, especially with severe hypovolemia and decreased electrolyte levels blood plasma (against the background of a salt-free diet or long-term use of diuretics), in patients with initially low blood pressure, renal artery stenosis (including bilateral), chronic heart failure or cirrhosis of the liver with edema and ascites.
Blockade of the RAAS by ACE inhibitors may be accompanied by a sharp decrease in blood pressure and/or an increase in the concentration of creatinine in the blood plasma, indicating the development of functional renal failure. These phenomena are more often observed when taking the first dose of the drug or during the first two weeks of therapy. Sometimes these conditions develop acutely and the time of their onset may vary. In such cases, it is recommended to resume therapy starting with lower doses, gradually increasing them. In patients with coronary artery disease and cerebrovascular diseases, a sharp decrease in blood pressure can lead to myocardial infarction or cerebrovascular accident.
Thiazide and thiazide-like diuretics are fully effective only in patients with normal or slightly impaired renal function (plasma creatinine concentration in adult patients below 25 mg/l or 220 µmol/l). In elderly patients, creatinine levels should be assessed taking into account age, body weight and gender.
At the beginning of treatment with diuretics, patients may experience a temporary decrease in glomerular filtration rate and an increase in the concentration of urea and creatinine in the blood plasma due to hypovolemia and hyponatremia. This transient functional renal failure is not dangerous for patients with unchanged renal function, but its severity may increase in patients with underlying renal failure. Patients with renal failure can take amlodipine in standard doses.
Changes in plasma concentrations of amlodipine do not correlate with the degree of renal dysfunction.
No special studies have been conducted on the use of Triplixam® in renal dysfunction. When using the drug Triplixam® in case of impaired renal function, the effects noted when taking individual components of the drug should be taken into account.
Content of potassium ions in blood plasma
Concomitant therapy with indapamide, perindopril and amlodipine does not prevent the development of hypokalemia, especially in patients with diabetes mellitus or renal failure. As with the use of other antihypertensive drugs in combination with a diuretic, regular monitoring of the content of potassium ions in the blood plasma is necessary.
Hyperkalemia may develop in some patients during treatment with ACE inhibitors, including perindopril. Risk factors for hyperkalemia include renal failure, deterioration of renal function, advanced age (> 70 years), diabetes mellitus, certain concomitant conditions (dehydration, acute cardiac decompensation, metabolic acidosis), concomitant use of potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene, amiloride), potassium preparations or potassium-containing substitutes for table salt, as well as the use of other drugs that increase the content of potassium ions in the blood plasma (for example, heparin, co-trimoxazole, i.e. the combination of trimethoprim + sulfamethoxazole). The use of potassium supplements/preparations, potassium-sparing diuretics, and potassium-containing table salt substitutes can lead to a significant increase in potassium levels in the blood, especially in patients with reduced renal function. Hyperkalemia can lead to serious, sometimes fatal, heart rhythm disturbances. If combined use of the above drugs is necessary, treatment should be carried out with caution, against the background of regular monitoring of the content of potassium ions in the blood serum (see section “Interaction with other drugs”).
Therapy with thiazide and thiazide-like diuretics is associated with a risk of hypokalemia. Hypokalemia (less than 3.4 mmol/L) should be avoided in the following high-risk patients: elderly and/or malnourished patients (even if not receiving concomitant drug therapy), patients with cirrhosis with edema and ascites, patients with coronary heart disease, chronic heart failure. Hypokalemia in these patients increases the toxic effect of cardiac glycosides and increases the risk of developing arrhythmia.
The risk group also includes patients with a prolonged QT interval, and it does not matter whether this increase is caused by congenital causes or the effect of drugs.
Hypokalemia, like bradycardia, contributes to the development of severe cardiac arrhythmias, in particular polymorphic ventricular tachycardia of the “pirouette” type, which can be fatal. In all the cases described above, regular monitoring of the content of potassium ions in the blood plasma is necessary. The first measurement of potassium ion content should be carried out within the first week from the start of therapy.
If hypokalemia is detected, appropriate treatment should be prescribed.
Elderly patients
Before starting to take the drug, it is necessary to assess the functional activity of the kidneys and the content of potassium ions in the blood plasma. At the beginning of therapy, the dose of the drug is selected taking into account the degree of reduction in blood pressure, especially in the case of a decrease in circulating blood volume (CBV) and loss of electrolytes. Such measures help to avoid a sharp decrease in blood pressure.
In elderly patients, increasing the dose should be done with caution (see sections “Dosage and Administration” and “Pharmacokinetics”).
Excipients
Sodium level
The sodium content in the drug Triplixam® is insignificant, as it is less than 1 mmol of sodium (23 mg) per tablet.
Side effects
Each drug has certain contraindications and side effects. Sirepar is no exception. When taking it, unpleasant phenomena may also occur, which need to be studied before using the drug.
In case of diseases of this organ, the first priority should be to begin adjusting your diet.
Contraindications
The medication should not be used in the following cases:
- Lactation;
- Pregnancy;
- Children under one year old;
- Hypersensitivity, tendency to allergies;
- Hepatitis during exacerbation.
In case of individual intolerance, this drug is also prohibited from use. Chronic diseases during the period of exacerbation can also cause refusal of Sirepar.
Side effects
The drug has side effects:
- Allergy;
- Pain and tingling in the abdominal area;
- Redness of the skin;
- Rash;
- Temperature increase;
- Itching and burning of the surface of the epidermis;
- Dizziness;
- Nausea.
If at least one of the presented symptoms appears, the drug should be stopped immediately. It is worth seeking help from a doctor. He will reduce the dosage of the medicine or prescribe another remedy that will not cause side effects in the patient.
During pregnancy
Used in pregnant and lactating women only for health reasons. During pregnancy and lactation, taking Sirepar is prohibited, as it can lead to complications and deterioration of the woman’s well-being. Milk may develop a specific taste.
During this period, the drug can harm not only the woman, but also the baby, because Sirepar cannot be taken by a child under one year of age. Injections can have a negative impact on the child's health.
If during pregnancy you experience discomfort in the liver area or the digestive system is not working properly, you should consult a doctor who will select the optimal medicine. You should not take risks with Sirepar.
Experience with the use of ademetionine in cancer patients receiving antitumor treatment
The problem of cancer is very relevant for modern society. Statistics show that over the past 100 years, in terms of morbidity and mortality, oncopathology has moved from 10th place to 2nd place, second only to diseases of the cardiovascular system. In addition, according to World Health Organization forecasts, the incidence and mortality from cancer worldwide will double from 1999 to 2021: from 10 to 20 million new cases of disease and from 6 to 12 million registered deaths. Chemotherapy occupies a leading place in modern treatment of cancer patients. Chemotherapy is a method of treating malignant neoplasms using cytotoxic drugs. Polychemotherapy (PCT) is the most common approach. It can be used as the only treatment method or in combination with other methods - surgery and radiation. In the case of combination treatment, chemotherapy may either precede other methods or complete treatment.
Advances in modern chemotherapy have made it possible to achieve success in curing many malignant neoplasms that were previously considered fatal. Increased effectiveness of treatment has been achieved through intensification of chemotherapy regimens. However, the negative side of PCT is the side effects of antitumor drugs due to the low selectivity of most cytostatics, which serves as a serious limitation in achieving maximum therapeutic effect.
Antitumor therapy destroys tumor cells, but at the same time damages normal rapidly dividing cells, which include bone marrow, the mucous membrane of the oral cavity and gastrointestinal tract, hair follicles, etc. The occurrence of side effects during chemotherapy in cancer patients is associated with the specificity of the antitumor drug effect of drugs, their low selectivity, as well as the need to maintain a sufficiently high therapeutic dose. The severity of side effects depends on the type of drug, its total and total dose, as well as the duration of chemotherapy.
Given the role of the liver in the metabolism of chemicals, it can be argued that there are no drugs that, under certain conditions, will not cause liver damage. Antitumor chemotherapy drugs occupy a leading position in the frequency and severity of hepatotoxic reactions they cause. However, establishing a cause-and-effect relationship between the use of a particular drug and liver changes is often difficult, especially in cancer patients receiving various drugs. The criteria for such a connection can be chronological dependence (the appearance of symptoms 5–90 days after the first dose of the drug), however, a delayed liver reaction to taking drugs is also observed in cancer patients receiving antitumor treatment. In general, the diagnosis of “drug-induced liver damage” is justified if, in connection with taking drugs, an increase in the activity of alanine aminotransferase (ALT) or the level of direct bilirubin (more than 2 norms) or a simultaneous increase in the levels of aspartate aminotransferase (AST), alkaline phosphatase (ALP) and total bilirubin is detected ( more than 2 norms for at least one of these indicators). Regular monitoring of aminotransferase activity and timely discontinuation of the drug if liver tests are abnormal are of great importance for the prevention of serious hepatotoxic reactions.
For the purpose of unification, the hepatotoxicity (HT) criteria of the US National Cancer Institute are currently used (Table 1).
Due to liver damage, all its functions are inhibited, especially detoxification. Cytostatics block the function of detoxification and cell regeneration, and this promotes the accumulation of the drug and increases the damaging effect on the liver.
In this regard, the development and use in clinical practice of drugs that reduce the toxicity of cytostatics on the body without reducing their antitumor effect is an urgent problem in modern oncology.
Hepatoprotectors are widely used for the treatment and prevention of hepatotoxic reactions.
A clinical observation was conducted at the palliative treatment department of the Moscow City Oncology Hospital No. 62, the purpose of which was to study the effectiveness and tolerability of the drug Heptor in cancer patients receiving PCT to prevent serious hepatotoxic reactions.
Heptor is a preparation of ademetionine, which is a natural substance endogenously synthesized from methionine and adenosine. Ademetionine is involved in three vital biochemical reactions: transmethylation, transsulfuration and aminopropylation and thus plays a critical role in a complex of metabolic processes. Ademethionine, being a methyl group donor, takes part in the synthesis of phosphatidylcholine, the main structural component of the cell membrane. In addition, ademetionine has an antioxidant, detoxifying effect, accelerates the regeneration of liver tissue, slows down the development of fibrosis, and also has an antidepressant effect. In addition, ademetionine plays a key role in the metabolism of nucleic acids and polyamines and is a precursor of glutathione. These processes are significantly affected during antitumor treatment in cancer patients and require the administration of exogenous ademetionine.
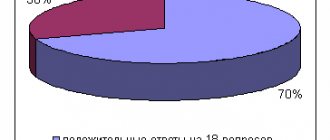
The observation included 41 patients (22 women and 19 men) aged 45 to 75 years with a morphologically (histologically and/or cytologically) verified oncological diagnosis, not subject to radical surgical treatment (stage 3) or after cytoreductive surgery, and also patients with distant metastases (stage 4) who have previously received chemotherapy and/or radiation therapy.
In the presence of hepatotoxicity, before starting the subsequent cycle of chemotherapy, patients were prescribed Heptor orally at a dose of 400 mg 2 times a day for 28 days. For patients with risk factors for developing HT, Heptor was prescribed for the entire period of chemotherapy.
As criteria for the effectiveness of taking the drug, we assessed the dynamics of biochemical activity (levels of ALT, AST, ALP and GGPP, bilirubin) on the 14th and 28th days. All adverse events were recorded during the observation process.
results
Cytolysis rates decreased in all patients already on the 14th day of treatment and practically returned to normal by the 28th day of therapy.
In patients with liver metastases, HT was characterized by higher levels of aminotransferases than in patients without liver damage. However, the response rate to treatment with Heptor (decrease in liver enzyme activity by more than 30% compared to baseline levels) was similar in patients with and without metastases. The data obtained indicate that liver metastases do not affect the results of treatment with the drug. No significant side effects or allergic reactions were recorded.
conclusions
The results of treatment showed that the use of the drug Heptor normalizes transaminase levels in 100% of patients with grade 1 HT within 4 weeks without changing chemotherapy regimens. In addition, significant positive dynamics of somatic and vegetative manifestations were established, namely: a decrease in nausea, bitterness in the mouth, itching of the skin, and flatulence.
The data obtained indicate the advisability of including the drug Heptor in the complex pharmacotherapy of cancer patients receiving cytostatics in order to correct their hepatotoxicity, which will allow not to interrupt chemotherapy and not reduce the dosage of cytostatics.
Literature
- Ostapowicz G., Fontana R., Schiodt F. et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States // Ann Intern Med. 2002; 137:947–954.
- Lopatkina T. N., Burnevich E. Z. Drug-induced liver damage. In the book. Mukhin N. A. (ed.) Practical hepatology. M., 2004. pp. 133–136.
- Lee W. Drug-induced hepatotoxicity // N Engl J Med. 2003; 349:474–485.
- DeLeve L., Shulman H., McDonald G. Toxic injury to hepatic sinusoid: sinusoidal obstruction syndrome (veno-occlusitis disease) // Semin Liver Dis. 2002; 22: 27–42.
- Santini D., Vincenzi B., Massacesi C. et al. S-Adenosylmethionine (Heptral) in the treatment of liver damage caused by chemotherapy // Anticancer Res. 2003; 23:5173–5180.
- Lieber C. S-Adenosyl-L-methionine: its role in the treatment of liverdisorders // Am J Clin Nutr. 2002; 76:1183–1187.
- Mato J., Corrales F., Lu S. et al. S-Adenosylmethionine: a control switch that regulates liver function // FASEB J. 2002; 16:15–26.
- Poonawala A. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis, a case control study // Hepatology. 2000; 32:689–692.
- Angulo P. Non-alcoholic fatty liver disease // N. Engl. J. Med. 2002; 346:1221–1231.
- Powell EE, Cooksley WG, Hanson R. et al. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years // Hepatology. 1990; 11: 74–80.
- Caldwell SH et al. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying dis-ease // Hepatology. 1999:29:664–669.
N. V. Babanina
GBUZ Moscow City Oncology Hospital No. 62 DZ Moscow, Moscow
Contact information for authors for correspondence
Analogs
If for some reason you cannot find Sirepar in a pharmacy, you should pay attention to analogues.
In terms of their effectiveness, they are not inferior to the above-mentioned medicine:
- Gepatomax Forte;
- Hepaforte;
- Silarsil;
- Geparsil;
- Silibor Forte;
- Forsliv;
- Livonorm;
- Liv-Ker;
- Larnamin;
- Hepanex;
- Hepa-Ess;
- Hepatosan;
- Maxar.
These products have certain features and possible contraindications. Before using drugs, you need to carefully read them. Then unpleasant phenomena can be avoided, and recovery will not take long to arrive.
Reviews
The medicine helps relieve pain in the abdominal area, eliminate the feeling of nausea and dizziness. The product is able to fight harmful microorganisms. The medicine fights pathogens.
You can read reviews about this product at the end of this article.
Patients say that their health improved within a few days. Full recovery occurred within two weeks. Not only adults, but also children are allowed to take the medicine.
In cases of poisoning and food allergies, this medication can be indispensable.
Digestion is restored. Patients feel full of energy. According to them, after taking this medicine, dizziness disappears. My health improves noticeably. Injection procedures are tolerable and do not cause pain.
According to patients, the drug is highly effective. With its help you can cure the liver, normalize the functioning of the digestive system and gastrointestinal tract.