Published: 10/19/2021 13:10:00 Updated: 10/19/2021
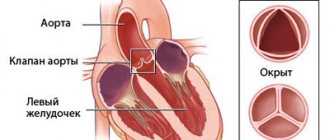
Heart disease is deformation and pathological changes in the structure of valves, septa and chamber walls, which lead to improper functioning of the organ and disruption of intracardiac hemodynamics.
The disease can be congenital or acquired. The chance of transmitting congenital heart disease from mother to child ranges from 3% to 50%. In clinically healthy parents, the risk of having a child with this pathology is 1% [1].
Heart disease is associated with a high risk of intrauterine and child mortality, sudden death in older patients, and also reduces the quality of life and ability to work, leading to disability.
Prevention of the disease includes proper pregnancy planning, a healthy lifestyle, timely diagnosis and treatment of pathology in the early stages. Surgery is considered the most effective therapy.
General information
Congenital heart disease is the most common congenital anomaly leading to mortality. Occurs in approximately 1% of newborns. Congenital heart defects most often appear in childhood. They can progress and, if not treated correctly, lead to death. Source: JIE Hoffman, S. Kaplan The incidence of congenital heart disease // JACC, 2002, Vol. 39, p.1890—1900
CHD can manifest as single anomalies or a combination of several disorders. It is most dangerous when the disease has no external manifestations and passes hidden. In modern conditions, treatment is usually successful, but timely and accurate diagnosis is vital.
The actions of the mother during pregnancy and of both parents during preparation for it are also important. To assess the risk of having a baby with congenital heart disease, you need to contact a geneticist.
CHD entails a number of complications, including bacterial endocarditis, heart failure, early pneumonia with a prolonged course, short-term fainting, pulmonary hypertension, myocardial infarction, attacks of shortness of breath, and angina syndrome.
Diagnosis of heart defects
The doctor may suspect the disease during the initial examination based on external signs such as bluish or pale skin, shortness of breath at rest.
On auscultation, a characteristic heart murmur or rhythm disturbances are heard. Using palpation, the doctor identifies swelling, pulsation of veins, and the borders of the liver. Light and heart sounds are heard percussion, and the boundaries of the heart are determined. It is important to collect anamnesis: patient complaints (for children - symptoms observed by parents), chronic, hereditary and past infectious diseases.
To confirm and clarify the diagnosis, additional examinations are carried out.
Laboratory diagnosis of heart disease includes a general blood test (leukoformula, hematocrit), urine analysis according to Nechiporenko. Instrumental methods include electrocardiogram, 24-hour Holter monitoring, cardiac ultrasound, chest x-ray, MRI of the heart and large vessels, and ECHO-CG.
For those planning pregnancy and pregnant women, it is recommended to undergo a special set of examinations:
- complete blood count, blood group and Rh factor, antibodies to Rh factor;
- cytological examination of smears from the cervix and cervical canal;
- test for TORCH infections (toxoplasmosis, rubella, cytomegalovirus infection, herpetic infection);
- to exclude renal failure: biochemical blood test (creatinine, urea, potassium, calcium, phosphorus, triglycerides, alkaline phosphatase, cholesterol, glucose), ultrasound of the pelvic organs, CT and MRI of the abdominal organs;
- pregnancy-associated plasma protein test;
- molecular study of the number of X chromosomes;
- genetic test to determine polymorphisms associated with the risk of developing arterial hypertension (hypertension) in the blood.
Phases of the disease
CHD occurs in three phases:
- first phase: during it, a compensatory and adaptive reaction to a failure in the dynamics of blood circulation is observed; in case of a serious violation, myocardial hyperfunction occurs.
- second phase: relative compensation occurs. The child’s motor activity and physiological development improves.
- the third phase is terminal. The body has already exhausted the possibilities of compensation; degenerative, dystrophic pathologies of the heart and nearby blood vessels are developing. If a child is sick, especially with complications, then the terminal phase occurs faster. Its outcome is only fatal. Source: E.E. Chepurnykh, E.G. Grigoriev Congenital heart defects // Siberian Medical Journal (Irkutsk), 2014, No. 3, pp. 121-127
Therefore, the earlier the pathology is detected, the more favorable its prognosis.
Treatment of heart disease
With congenital pathology, the diagnosis is usually known even before birth.
Only surgical treatment aimed at completely eliminating the cause is considered effective. The sooner an operation to correct a heart defect is performed, the greater the chance that the defect will not affect the child’s development, and the lower the risk of postoperative complications. If such intervention is not possible, then the child is prescribed a special regimen of physical activity and nutrition. The treatment tactics for an acquired disease require an integrated approach. In this subgroup of patients, medication (symptomatic) treatment, diet therapy, and lifestyle correction are first used. If there is no effect, worsening symptoms or risk of complications, surgery is prescribed.
There are several types of surgical intervention for heart defects:
- bypass (creating a new path for blood flow bypassing the affected area of the vessel);
- endoprosthetics (replacement of the affected valve with a prosthesis);
- separation (valvuloplasty) and dissection (valvotomy) of the valve leaflets.
Causes of pathology
CHD may develop if:
- parents smoke;
- parents drink alcohol;
- the fetus is affected by external factors during the period of development and formation (high background radiation, lack of vitamins, viruses carried by the mother, polluted air, water, a number of chemicals, including heavy metals). Source: L.N. Falyush, V.V. Florensov Risk factors for congenital heart defects // Clinical medicine. Bulletin of the All-Russian Scientific Center SB RAMS, 2010, No. 6(76), p.67-69
Prevention and recommendations for heart defects
Congenital heart disease can be prevented only through a comprehensive assessment of the health status of parents when planning pregnancy, adherence to a nutritious diet and proper conditions for the pregnant woman.
Prevention of acquired heart disease consists of timely and complete cure of the underlying disease that caused the pathology. General recommendations include following a cardiotrophic diet, quitting smoking and alcohol, moderate physical activity, avoiding colds and infectious diseases, and undergoing regular examinations by a cardiologist.
Symptoms of congenital heart disease
They are divided into two large groups according to the color of the child’s skin: “white” and “blue”. A changed skin tone is the first reason for parents and pediatricians to be wary.
"Blue" vices
They usually appear either immediately at birth or a little later. In this case, the ears, lips and body skin are susceptible to cyanosis. Blue discoloration can occur during exertion (screaming, crying of a newborn), during breastfeeding. The “blue” appearance is usually manifested by a mirror arrangement of the great vessels, atresia of the pulmonary artery, and tetralogy of Fallot.
CHD of the “white” variety
Accompanied by pallor and coldness of the extremities. When listening with a stethoscope, noises are heard. They are not direct symptoms, but a heart examination is still required. With “white” pathologies, heart failure is often detected. Changes are detected on x-rays, ECG, ECHO-CG. This type of congenital heart disease is most often a pathology of the interatrial septum and interventricular septum.
Unfortunately, not all types of congenital heart disease occur in newborns. A child can feel well even up to 10 years of age. But sooner or later the vice will appear:
- delay in physiological development;
- pallor or cyanosis;
- shortness of breath during exercise.
Symptoms of heart disease
With a minor violation, the symptoms of the disease do not appear for a long time.
If hemodynamics are seriously impaired, shortness of breath, bluish skin, swelling, pain in the heart, rapid heartbeat, causeless cough, increased fatigue, decreased ability to work, dizziness and fainting, high or low blood pressure are observed. Auscultation also reveals a heart murmur. In newborns, heart disease is manifested by the appearance of cyanosis during breastfeeding, cold extremities and the tip of the nose, poor weight gain, and developmental delays.
Treatment methods
Treatment of congenital heart disease is carried out only by surgery . Cardiac surgeons perform complex reconstructive interventions, successfully curing those forms of congenital heart disease that were previously considered inoperable. If the diagnosis is made early and treatment is carried out promptly, heart function can be restored to 100%.
Non-invasive therapy (medication, physiotherapy, etc.) may be prescribed as an auxiliary measure. Such treatment is also carried out in cases where it is possible to postpone the operation to a later time or there is a “white” congenital heart disease that has little impact on the child’s well-being during growth and development.
Treatment for the diagnosis of congenital heart disease in newborns
Treatment methods depend on the type of heart defect:
- Minimally invasive procedures
- Radical surgery
- Heart transplant
- Drug therapy
- Long-term therapy
If the heart defects are not very serious, minimally invasive procedures can be used. Their essence is that a thin catheter is inserted into the heart through the femoral vein, and the necessary instruments are delivered to the defect inside the catheter.
The most radical but effective method of treating congenital heart disease is surgery. This is a traditional open intervention with opening of the chest and the heart itself. Most of these operations are performed using a heart-lung machine. After heart surgery, a child faces a long and difficult recovery period, but sometimes it is the only possible way to cure.
Heart transplantation is used in the most severe cases, in which traditional surgery is helpless in case of severe congenital heart disease.
Drug therapy is used mainly for auxiliary purposes, improving the functioning of the heart and blood flow.
Long-term therapy involves several consecutive operations on congenital heart disease.
We invite you to “SM-Clinic”
Our clinic’s staff includes some of the best specialists in the Northern capital. We employ experienced pediatricians and pediatric cardiologists who will promptly identify the presence of alarming symptoms and prescribe all the necessary examinations. “SM-Clinic” is well equipped; we can conduct all tests for the presence of congenital heart disease.
Make an appointment with us as soon as possible if you notice signs of congenital heart disease in your child. Time plays a huge role in this disease.
Sources:
- HER. Chepurnykh, E.G. Grigoriev. Congenital heart defects // Siberian Medical Journal (Irkutsk), 2014, No. 3, pp. 121-127.
- L.N. Falyush, V.V. Florensov. Risk factors for congenital heart defects // Clinical medicine. Bulletin of the All-Russian Scientific Center SB RAMS, 2010, No. 6(76), p.67-69.
- J. I. Hoffman, S. Kaplan. The incidence of congenital heart disease // JACC, 2002, Vol. 39, p.1890—1900.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Diagnosis of congenital heart disease in newborns
Naturally, the earlier a congenital heart defect in newborns is detected and timely treatment begins, the more favorable the prognosis. However, due to the absence of clearly defined symptoms and, accordingly, no treatment at all, there are cases of death among children under 1 year of age (occasionally even older).
Usually, during preventive examinations, the doctor must listen to the baby’s heart. If murmurs are heard there, this is a reason for a detailed examination of the heart (although not necessarily a symptom of congenital heart disease).
For this purpose, parents and children are referred to specialists with a narrower profile - a cardiologist and a cardiac surgeon.
If you suspect a heart defect, the baby’s parents do not need to immediately turn to Internet search engines with the request “congenital heart defect surgery.” Not all defects require radical surgical intervention. And the main thing is to first establish the correct diagnosis.
Changes characteristic of congenital heart disease in a newborn are revealed by the following research methods:
- X-ray of the chest (as well as ventriculography - x-ray with contrast injection).
- Echocardiography (using ultrasound to examine the condition of the heart muscle, valves, blood flow in the heart cavities).
- Electrocardiogram – ECG (or methods based on it: stress ECG (treadmill test, bicycle ergometry), ECG Holter monitoring).
If the above examination methods reveal the presence of a serious disease - congenital heart disease, then further diagnostics are carried out in the cardiac surgery department on an inpatient basis. Surgeons, if necessary, conduct examinations using procedures such as angiocardiography and probing of the heart chambers.
Modern high-tech medical equipment allows you to conduct a full comprehensive examination of the heart and blood vessels in order to establish the most accurate diagnosis and choose the necessary treatment tactics.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a cardiologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Electrocardiography (ECG) | 1400 rub. |
| Echocardiography (ultrasound of the heart) | 3500 rub. |
Causes of congenital heart disease
The main leading causes in the formation of defects are most often structural and quantitative chromosomal abnormalities and mutations, i.e.
primary genetic factors. It is also necessary to pay attention to potentially teratogenic environmental factors: various intrauterine infections (rubella viruses, cytomegalovirus, coxsackie, infectious diseases in the mother in the first trimester), medications (vitamin A, antiepileptic drugs, sulfasalazine, trimethoprim), constant contact with toxic substances ( paints, varnishes). In addition, it must be remembered that maternal factors have a negative impact on intrauterine development: reproductive problems preceding a given pregnancy, the presence of diabetes mellitus, phenylketonuria, alcoholism, smoking, age, but also factors from the father - age, drug use ( cocaine, marijuana).
The leading role belongs to the multifactorial theory of the development of congenital heart defects (up to 90%).
Types of congenital heart defects
- Atrial septal defect (ASD) or patent foramen ovale is diagnosed when one or more holes are identified in the interatrial septum. One of the most common congenital heart defects. Depending on the location of the defect, its size, and the strength of blood flow, more or less pronounced clinical signs are determined. ASD is often combined with other cardiac anomalies and is associated with Down syndrome.
- Ventricular septal defect (VSD) is diagnosed when the interventricular septum is underdeveloped at various levels with the formation of a pathological communication between the left and right ventricles. It can occur either alone or together with other developmental anomalies. With a small defect, there is often no pronounced lag in physical development. VSD is dangerous because it can lead to the development of pulmonary hypertension, and therefore must be promptly corrected surgically.
- Coartation of the aorta is a segmental narrowing of the aortic lumen with disruption of normal blood flow from the left ventricle to the systemic circulation. Up to 8% of all cases of congenital heart disease are detected, more often in boys, and are often combined with other anomalies.
- Patent ductus arteriosus is diagnosed when the duct of Batallus is not closed, which is detected in newborns and becomes overgrown in the future. As a result, a partial discharge of arterial blood from the aorta into the pulmonary artery occurs. With this congenital heart disease there are often no severe clinical manifestations, however, the pathology requires surgical correction, since it is associated with a high risk of sudden cardiac death.
- Pulmonary atresia - underdevelopment (full or partial) of the pulmonary valve leaflets with the development of backflow of blood from the pulmonary artery into the cavity of the right ventricle is diagnosed. Subsequently leads to insufficient blood supply to the lungs.
- Pulmonary valve stenosis is an anomaly in which narrowing of the pulmonary valve opening is diagnosed. As a result of pathology, most often of the valve leaflets, normal blood flow from the right ventricle to the pulmonary trunk is disrupted.
- Tetralogy of Fallot is a complex combined congenital heart disorder. Combines ventricular septal defect, pulmonary stenosis, right ventricular hypertrophy, and aortic dextraposition. With this pathology, a mixture of arterial and venous blood occurs.
- Transposition of the great vessels is also a complex congenital disorder. With this pathology, the aorta originates from the right ventricle and carries venous blood, and the pulmonary trunk originates from the left ventricle and carries arterial blood, respectively. Paroxysm is severe and is associated with high mortality in newborns.
- Dextrocardia is an anomaly of intrauterine development characterized by the right-sided placement of the heart. Often, there is a “mirror” arrangement of other unpaired internal organs.
- Ebstein's anomaly is a rare congenital heart defect, diagnosed when the location of the tricuspid valve leaflets changes. Normally - from the atrioventricular fibrous ring, with an anomaly - from the walls of the right ventricle. The right ventricle is smaller, and the right atrium is elongated, including abnormal valves.
Diagnosis of congenital heart disease
The data from laboratory and instrumental research methods are variable depending on the specific defect. Among the leading methods are:
- ECG (right or leftogram, various variants of arrhythmias, etc.).
- Plain radiography of the heart (mitral configuration for defects with enrichment of the pulmonary circulation, aortic configuration with depletion) and contrast radiological techniques (angiography, ventriculography, etc.).
- Echo-CG (the main technique allows you to see the morphology of the defect and determine the functional state of the heart).
- Doppler echo-CG (allows you to determine the direction of blood flow - to identify regurgitation and turbulence).
How do heart valve diseases manifest?
Most often, patient complaints are nonspecific: shortness of breath, rapid pulse, arrhythmia, fatigue, cyanosis, dizziness.
The severity and nature of symptoms depend on the location of the affected valve. With valve defects of the left half of the heart (mitral and aortic), the lungs are primarily affected, because Blood stagnates in their vessels, which manifests itself as shortness of breath. There are also signs of insufficient blood supply to all organs and systems, primarily the brain and the heart itself. Dizziness, fainting, and angina occur. If the functioning of the valves of the right half of the heart (tricuspid and pulmonary valves) is disrupted, blood stagnates in the vessels of the systemic circulation, i.e. all organs except the lungs are affected. Swelling of the legs and feet, ascites (fluid in the abdominal cavity), enlargement of the liver, etc. develop (LIVER INCREASES, ETC.).
Heart valve defects are dangerous due to their complications and impact on the body, so the main prevention of pathological conditions is regular examinations and treatment of diseases leading to the formation of valve defects.