Macropen® tablets are used for the following indications:
- infections of the respiratory and genitourinary tract caused by mycoplasmas, legionella, chlamydia and Ureaplasma urealyticum;
- infections of the respiratory tract, skin and soft tissues and other infections caused by bacteria sensitive to midecamycin and penicillin in patients with hypersensitivity to penicillin;
- enteritis caused by Campylobacter spp. bacteria;
- treatment and prevention of diphtheria and whooping cough.
Side effects
From the blood and lymphatic system: eosinophilia.
From the gastrointestinal tract: nausea, loss of appetite, vomiting, diarrhea, stomatitis, abdominal pain, pseudomembranous colitis.
From the skin and subcutaneous tissues: rash, urticaria and itching, angioedema, Stevens-Johnson syndrome.
From the liver and biliary tract: increased levels of transaminases and jaundice.
If severe adverse reactions occur, treatment should be discontinued.
Pharmacological properties of the drug Midecamycin
Macrolide antibiotic. Binds to ribosomes and thus inhibits protein synthesis in bacterial cells. In low doses the drug acts bacteriostatically, and in higher doses it is bactericidal. After oral administration, midecamycin is well absorbed. In adults, after oral administration of 600 mg of the drug, its maximum concentration in the blood serum is achieved after 40 minutes. Food intake does not have a significant effect on the concentration of midecamycin in the blood serum. Midecamycin penetrates well into tissues, especially into the parotid and submandibular glands, lymph nodes, skin and lungs. The concentration of midecamycin in tissues significantly exceeds its concentration in blood plasma. Two metabolites of midecamycin have antimicrobial effects. Excreted in feces and urine. Gram-positive aerobes and anaerobes, some gram-negative bacteria, as well as mycoplasmas, chlamydia and legionella are sensitive to midecamycin. Midecamycin is highly effective against streptococci, pneumococci, staphylococci and mycoplasma pneumoniae. Effective against staphylococci resistant to penicillin, tetracyclines, etc. Acts on some strains of Staphylococcus aureus resistant to erythromycin and ampicillin.
Note!
Description of the drug Macropen table. p/o 400 mg No. 16 on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use.
Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug). Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.
Use of the drug Midecamycin
The daily dose for adults is usually 1200 mg of midecamycin in 2-3 divided doses. For severe and moderate infectious diseases, children are prescribed 30–50 mg/kg per day in 2 divided doses. For milder forms of infections, the daily dose can be reduced to 20 mg/kg. The duration of treatment is 7–10 days; if necessary, treatment can be extended. The suspension is usually prescribed to children. a single dose for a child weighing less than 5 kg is 130 mg, 5-10 kg - 265 mg, 11-15 kg - 350 mg, 16-20 kg - 525 mg.
The use of midecamycin in pediatric practice
Antibiotic therapy occupies one of the leading places in the complex of therapeutic measures for various infectious diseases. When it comes to choosing a drug for a small patient, safety and the absence of serious side effects come to the fore. Currently, macrolides are recognized as drugs with a minimal spectrum of adverse effects and favorable pharmacokinetic properties. A prominent representative of the macrolide group is midecamycin. Due to its high efficiency, absence of significant adverse effects, ease of use, and the availability of two pediatric dosage forms (tablets and suspension), the antibiotic has become widespread in pediatric practice.
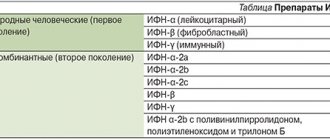
Table. Classification of macrolides
Macrolide antibiotics are used for many infections, primarily of community-acquired origin. The history of their use goes back over 40 years. The first macrolide antibiotic to find clinical use was erythromycin, obtained in 1952 from a culture of the soil fungus Streptomyces erythreus
. To date, about 20 macrolide antibiotics have been created, eight of them are actively used in clinical practice [1]. Macrolides are considered one of the rapidly developing classes of antibiotics due to their high efficiency and relative safety. They are characterized by a wide spectrum of antimicrobial activity and favorable pharmacokinetic properties and are well tolerated by young patients. An important component of the clinical success of macrolides is activity against not only common pathogens, but also intracellular pathogens [1, 2].
Based on their origin, macrolides are divided into natural and semi-synthetic. According to their chemical structure, 14-, 15- and 16-membered macrolides are distinguished depending on the number of carbon atoms in the lactone ring (see table).
Midecamycin, roxithromycin, spiramycin, josamycin, and azithromycin are widely used in pediatric practice.
Midecamycin is a natural 16-membered macrolide produced by the fungus Streptomyces mycarofaciens
. The drug has been used in clinical practice since 1985. The semi-synthetic derivative of midecamycin, midecamycin acetate, has improved antimicrobial and pharmacological properties compared to its natural analogue. It is better absorbed in the gastrointestinal tract and creates higher tissue concentrations. The mechanism of action of midecamycin is to bind to the catalytic peptidyl transferase center of the 50s subunit of ribosomes, which leads to disruption of the processes of translocation and transpeptidation, premature cleavage of the growing tRNA polypeptide chain and, as a consequence, suppression of protein synthesis in the ribosomes of microbial cells [1, 3] .
Midecamycin is highly effective against gram-positive microorganisms Streptococcus pneumoniae, St.
pyogenes, Staphylococcus aureus, Corynebacterium diphtheriae, Listeria monocytogenes ,
gram-negative cocci and bacilli
Neisseria gonorrhoeae, Moraxella catarrhalis, Bordetella pertussis, Campylobacter jejuni, Helicobacter pylori.
Low sensitivity is observed in
Haemophilus influenzae.
Like other macrolides, midecamycin is active against intracellular microorganisms (
Chlamydia trachomatis, Chlamydophila pneumoniae, Mycoplasma pneumoniae, M. hominis, Ureaplasma urealyticum
).
Midecamycin acetate has a post-antibiotic effect, which, according to some scientists, is due to irreversible changes in the ribosomes of the pathogen, leading to blocking of translocation [1, 3, 4]. The group of macrolides in general and midecamycin in particular are characterized by anti-inflammatory and immunomodulatory effects. Macrolides increase the activity of T-killers, accumulate in neutrophils and macrophages, enhance their phagocytic activity and migration to the site of inflammation. In addition, macrolides influence oxidative reactions in phagocytes and promote their degranulation, increase the production of anti-inflammatory cytokine (interleukin (IL) 10) by monocytes, reduce the production of pro-inflammatory cytokines by monocytes (IL-1, tumor necrosis factor alpha) and lymphocytes (IL-2) , reduce the formation of inflammatory mediators - prostaglandins, leukotrienes and thromboxanes. The anti-inflammatory effect occurs even at subtherapeutic concentrations of macrolides and is comparable to the effect of non-steroidal anti-inflammatory drugs.
Acquired resistance to macrolides develops quickly, but after stopping contact with the antibiotic, sensitivity to it is restored over time. MLS-type resistance (modification of the target of action - the ribosomal 50s subunit) does not develop to midecamycin. In addition, the development of other resistance mechanisms (changes in cell wall permeability, antibiotic inactivation, and efflux) is less common [1, 3].
Midecamycin, compared to erythromycin, has better organoleptic and pharmacokinetic properties, is better absorbed in the gastrointestinal tract, is stable in an acidic environment, is quickly and quite completely absorbed in tissues, creating high concentrations in internal organs due to its high solubility in lipids, in particular tonsils , bronchi and lungs. Trace concentrations are found in the maxillary sinuses.
Midecamycin is excreted in significant quantities into breast milk. The drug is rapidly absorbed into the blood, reaching peak serum concentrations in children 1–3 hours after administration at a dose of 10–30 mg/kg (0.76–2.3 mg/l).
After a single dose, two peaks of maximum concentration are recorded. The second peak (often exceeding the first) is due to the ability of drugs to accumulate in bile with subsequent reabsorption from the intestine.
Plasma protein binding is about 47%.
The drug and its metabolites are excreted mainly through the liver (70%) and kidneys (10%).
The results of a clinical multicenter study conducted in Russia confirmed the advantages of midecamycin over erythromycin in terms of safety in children. Adverse reactions with the use of erythromycin were observed twice as often as with the use of midecamycin.
According to the results of a three-year post-marketing clinical observation in Japan, which included 12,169 children (87% of patients under six years of age) receiving midecamycin acetate syrup, side effects developed in only 66 of them (0.54% of cases, in children under one year of age - 0.97 %). At the same time, only in 0.38% of cases were there adverse events from the gastrointestinal tract, in 0.15% - skin rash and in 0.01% - increased activity of liver enzymes. No serious side effects have been reported. None of the 26 patients with an allergy to beta-lactam antibiotics had allergic symptoms when prescribed midecamycin [5]. Based on the results of a study of midecamycin, acetate was recognized as the safest macrolide [4, 6, 7].
The Research Center for Children's Health also conducted a study of the side effects of midecamycin and midecamycin acetate in 76 children. Adverse reactions in the form of abdominal pain and dyspeptic symptoms were observed in three patients. One child with a history of food and drug allergies developed an allergic rash on the third day of treatment, which was relieved within 24 hours after stopping the drug. This indicated the presence of adverse reactions in only 4% of patients [2].
The results of studying the problem of drug-drug interactions showed that midecamycin, unlike erythromycin, is a weak inhibitor of the microsomal cytochrome P450 system [1]. Therefore, it does not have a significant effect on the concentration of theophylline and antihistamines, which allows its use according to indications in children with allergic diseases.
Midecamycin in Russia is available in two dosage forms - 400 mg tablets and powder for the preparation of a suspension - 175 mg of midecamycin acetate in 5 ml of suspension. The tablet form has age restrictions and is contraindicated for children under three years of age. There are no age restrictions for the suspension form.
Midecamycin is widely used in clinical pediatric practice. The results of numerous studies conducted in many domestic and foreign medical centers have confirmed the high clinical and bacteriological effectiveness of midecamycin (98–85%) in children with nasopharyngitis, tonsillitis, sinusitis, pneumonia and chronic bronchitis [7, 8].
The causative agents of acute tonsillitis can be not only viruses and bacteria, but also protozoa and fungi. As a rule, in children under three years of age, acute tonsillitis is associated with viruses. In children over the age of five, bacterial forms predominate. However, the peak incidence of group A beta-hemolytic streptococcus (GABHS) occurs between the ages of five and ten years. GABHS is the cause of acute bacterial tonsillitis in 25–30% of cases. But with recurrent tonsillitis, GABHS is isolated in 50% of children, including in association with Staphylococcus aureus and Staphylococcus epidermidis, H. influenzae
,
H. parainfluenzae
,
St.
pneumoniae ,
M. catarrhalis
in 52% of children [6].
In recent years, there has been a tendency to increase the proportion of intracellular pathogens (mycoplasmas and chlamydia) in the etiology of tonsillopharyngitis in children, especially preschool age. Detection rates can exceed 10% [4]. Of course, the high activity of macrolides against intracellular pathogens, which occur in 40–45% of children with recurrent chronic tonsillitis and adenoiditis, provides them with a leading position in the fight against this pathology. These pathogens are especially common in immunocompromised children, in children with a lymphatic constitution, with intermittent infections of the lower and upper respiratory tract, and in children who are often ill. Macrolides are the only safe drugs for children infected with these pathogens. This is confirmed by the experience of using the 16-membered macrolide midecamycin in the treatment of exacerbation of chronic tonsillitis in children with peritonsillar abscesses. Excellent results, that is, almost complete recovery, in 87% of children indicate the sustainable effect of midecamycin in the treatment of recurrent complicated chronic tonsillitis [6]. The drug was used at a dose of 30–50 mg/kg/day, both in the form of tablets and as a suspension, for seven to ten days for acute tonsillitis and from ten to 14 days for exacerbation of chronic tonsillitis.
Thus, at present, macrolides can become the first choice drugs for acute, exacerbations of chronic tonsillitis and their complications in children. At the same time, macrolides cannot be the first choice drugs in children with diseases of the ENT organs such as acute otitis media, acute sinusitis. That is, we are talking about diseases in 15–32% of cases associated with H. influenzae.
Midecamycin, along with other macrolides, is the drug of choice for acute bronchitis and exacerbation of chronic bronchitis, atypical pneumonia caused by intracellular pathogens, as well as community-acquired pneumonia, especially in children with allergies and hypersensitivity to penicillin drugs [2, 7].
In case of community-acquired pneumonia in children aged one to six months, atypical pathogens are detected in more than 30% of cases, more often C. trachomatis
, less commonly
M. hominis
.
In children under one year of age, staphylococcus plays a significant role as the causative agent of complicated forms of pneumonia (58%). St.
begins to play a significant role as an infectious agent. pneumoniae .
In children aged six months to six years, M. pneumoniae
is detected in 10–15% of cases.
Between the ages of seven and 15 years, the proportion of atypical pneumonias caused by M. pneumoniae
(20–40%) and
C. pneumoniae
(7–24%) increases.
Frequency of release of St.
pneumoniae in children aged from one to three years increases to 62%, in children over three years old - up to 70%.
A domestic controlled comparative study was conducted on the effectiveness of erythromycin and midecamycin in children aged from one to 15 years with uncomplicated community-acquired pneumonia, exacerbation of chronic bronchopulmonary diseases and recurrent bronchitis [2]. Erythromycin was prescribed at a dose of 30–50 mg/kg/day four times a day, midecamycin – at a dose of 30–50 mg/kg/day two to three times a day. The course of treatment for pneumonia and bronchitis was seven to ten days, for chronic respiratory diseases - from ten to 14 days or more. Erythromycin and midecamycin, like other oral antibiotics, were prescribed for mild and moderate respiratory diseases. The basis for the use of midecamycin for community-acquired pneumonia and exacerbations of chronic bronchopulmonary diseases was data indicating the high sensitivity of pneumotropic flora, including atypical pathogens, to it, as well as its ability to form high concentrations in bronchial secretions and lungs. The results of this study showed the effectiveness of the oral drug erythromycin against community-acquired pneumonia in 75% of children. However, quite often (16% of cases) adverse reactions were observed (dyspeptic symptoms, nausea, vomiting, abdominal pain), which required discontinuation of the drug in some patients. During exacerbation of chronic bronchopulmonary diseases, erythromycin was effective in 71% of cases, but the frequency of adverse events in this group was even higher (19%). A higher effectiveness of midecamycin was recorded in community-acquired pneumonia (70%). Only one child had adverse reactions from the gastrointestinal tract (abdominal pain). A more pronounced therapeutic effect was obtained in children with exacerbation of recurrent bronchitis (93%). Only one child had adverse reactions from the gastrointestinal tract [2].
Taking into account the fact that macrolides have an equally good effect on both extracellular and intracellular pathogens, midecamycin can be used in the treatment of a number of urogenital infections caused by chlamydia, mycoplasma, etc. Urogenital chlamydia and mycoplasmosis currently occupy a significant place among sexually transmitted diseases. In newborns, colonization of the genital tract with mycoplasmas occurs during childbirth. According to the World Health Organization, 60–70% of children born to mothers with chlamydial and mycolasma infections were infected [9]. Typically, infections are latent and asymptomatic, exacerbating during stressful situations. Treatment involves the mandatory use of immunostimulating therapy and macrolides. Midecamycin may be the drug of choice.
Macrolides have also found application in gastroenterology - in the treatment of chronic gastroduodenitis associated with H.
pylori
.
Midecamycin is also active against H. pylori
, which makes it possible to consider its inclusion in eradication therapy regimens if the use of clarithromycin is not possible.
Midecamycin is effective in the treatment of children with pyoderma, which is also confirmed by research results [3, 10]. Midecamycin is used for whooping cough in children (moderate and severe form) and is included in the complex of therapeutic measures for diphtheria of the pharynx.
High sensitivity to midecamycin of typical pneumotropic and atypical pathogens that cause infections of the respiratory tract and urogenital tract in children, ease of use, the presence of two children's dosage forms (tablets and suspension), frequency of administration up to two times a day, high efficiency and absence of pronounced adverse effects allow us to recommend the antibiotic for widespread use in pediatric practice.