One of the dangerous and insidious diseases in young children is rotavirus infection. According to WHO, the mortality rate from it is 30%. The symptoms are similar to those of many other diseases: food poisoning, intestinal upset, cholera and others. Therefore, if parents try to make a diagnosis on their own, in most cases they are mistaken. Failure to see a doctor in a timely manner or treating “diarrhea” with home remedies can result in tragedy. What is the disease for which vaccination is included in the national calendar of the USA and some European countries?
What are rotaviruses
Rotaviruses are a group of viral particles that are similar in morphological and antigenic characteristics. These are RNA viruses with a 3-layer shell of protein molecules. The particles got their name because of their similar appearance to a wheel (in Latin the word “wheel” is translated as “rota”).
Routes of transmission
Rotavirus infection is transmitted from a sick person in several ways:
- fecal-oral;
- contact and household;
- airborne.
At the onset of the disease, the feces of an infected person contain up to 1011 particles of rotavirus. After about a week, their number decreases, but the person remains a source of infection for almost a month.
What factors influence the transmission of the virus? These are: water, food, household items. When the pathogen enters the aquatic environment, especially into water supply systems, epidemic situations may occur. Among food products, the most dangerous are dairy and meat products, raw vegetables and fruits. The hygienic condition of kitchen equipment, household items, and cleanliness of hands are of great importance.
Who's at risk
The main risk group is children aged six months to five years. During this period, they manage to get sick with rotavirus up to five times. 90% of older children have antibodies to the infection in their blood, which indicates a previous illness.
Rotavirus infection easily penetrates the body - if a person does not have immunity to it, the probability of getting sick is almost 70%. Re-infection is also possible, but how long the immune response to rotavirus lasts and when secondary infection can occur has not been established.
Epidemiology
Rotavirus infection is a typical seasonal disease. According to statistics, in almost 93% of cases the disease develops in the winter months.
The infection often spreads in epidemic outbreaks - especially in kindergartens, hospitals, nursing homes and other institutions where children or adults with weakened immune systems are in close contact.
Children are most susceptible to infection. The share of rotavirus infection is 39.4% of all episodes of diarrhea under the age of 5 years.
How long does the virus live
The pathogen has a fairly high viability - on various surfaces, depending on environmental conditions, it can retain its properties for up to a month, and in feces for up to six months. The virus is resistant to factors such as:
- high temperature (up to 60-70˚С);
- low temperature (withstands even freezing);
- ultrasonic influence;
- UV irradiation;
- antibacterial agents;
- fat solvents;
- chloroform and ether.
Rotavirus can be killed by boiling, treating with strong alkaline solutions or acids. The pathogen has increased sensitivity to ethanol (96˚), formaldehyde, and hydrogen peroxide.
How does infection occur?
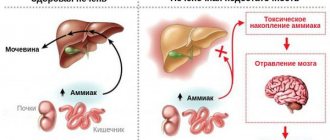
Penetrating into the body through the oral cavity, rotavirus penetrates into the mucous membrane of the small intestine within half an hour. After just 1-3 days, changes begin in it: cells die and exfoliate from the surface of the intestine, food digestion processes are disrupted, absorption of substances and the functioning of enzymes deteriorate. At the same time, intestinal motor activity increases. Undigested residues accumulate in it, acids and other metabolic products are formed, and difficulties arise with the absorption of water. As a result, diarrhea and dehydration develop.
Course of the disease7
The following stages are characteristic of intestinal flu:
- The incubation period is from 12 hours to 5 days.
- Acute onset - as a rule, already in the first hours of illness the patient’s temperature rises sharply, chills appear, a strong cough begins, and the nose gets stuffy. A little later, the main symptoms appear - nausea, diarrhea with watery stools, cramping pain in the stomach and intestines.
- If the infection is properly treated, diarrhea will last from 5 days to a week. In the first 2-3 days, the stool remains watery (in infants it may become colorless), then it becomes clay-like.
- Pain and sore throat, runny nose and cough disappear after 2-3 days. At the same time, the body temperature remains elevated.
- The rehabilitation period after rotavirus gastroenteritis is 5-7 days.
An unpleasant surprise - rotavirus during trips and travels
Many stories have been told on the Internet about how rotavirus ruined a vacation while traveling abroad. This usually happens with small children, but cases are not excluded when the whole family spends several days, what is popularly called, “embracing the toilet.” One of these cases, although it ended happily, was not pleasant enough. Thailand. Vacation. Heat. A family with a 9-month-old child is admitted to the hospital. Diagnosis: rotavirus infection. It was not possible to combat dehydration with improvised means; it is difficult to explain to a child at this age that he needs to drink a lot. Therefore, for 3 days of vacation, instead of swimming in the sea and riding elephants, there were IVs and other treatment. It’s good that insurance was taken out that covered this “entertainment”, because the bill that was presented to the insurance company was about 100 thousand rubles.
Sources
1. Efficacy of probiotic use in acute rotavirus diarrhea in children: A systematic review and meta-analysis Elaheh Ahmadi, MSc, Reza Alizadeh-Navaei, MD, PhD, and Mohammad Sadegh Rezai, MD, PMC - [https://www. ncbi.nlm.nih.gov/pmc/articles/PMC4649266/] (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4649266/) 2. Global, Regional, and National Estimates of Rotavirus Mortality in Children <5 Years of Age, 2000-2013. Tate JE, Burton AH, Boschi-Pinto Parashar; World Health Organization–Coordinated Global Rotavirus Surveillance Network, PubMed - [https://www.ncbi.nlm.nih.gov/pubmed/27059362] (https://www.ncbi.nlm.nih.gov/pubmed/27059362) 3. Rotavirus Vaccine, Family Practice - [https://www.fpnotebook.com/ID/Immunize/RtvrsVcn.htm] (https://www.fpnotebook.com/ID/Immunize/RtvrsVcn.htm) 4. Rotavirus. Vaccination, CDC - [https://www.cdc.gov/rotavirus/vaccination.html] (https://www.cdc.gov/rotavirus/vaccination.html) 5. Risk Factors Associated With Rotavirus Gastroenteritis During a Community Outbreak in Chiapas, Mexico During the Postvaccination Era, Journal of Pediatric Infectious Diseases - 7. Risk Factors for Severe Rotavirus Gastroenteritis Huppertz, Hans-Iko MD; Salman, Nuran MD; Giaquinto, Carlo MD, Journal of Pediatric Infectious Diseases -[https://journals.lww.com/pidj/Fulltext/2008/01001/Risk_Factors_for_Severe_Rotavirus_Gastroenteritis.3.aspx] (https://journals.lww.com/pidj/Fulltext /2008/01001/Risk_Factors_for_Severe_Rotavirus_Gastroenteritis.3.aspx) 8. Rotavirus. Symptoms, CDC -[https://www.cdc.gov/rotavirus/about/symptoms.html] (https://www.cdc.gov/rotavirus/about/symptoms.html) 9. Rotavirus. Overview, Mayo Clinic -[https://www.mayoclinic.org/diseases-conditions/rotavirus/symptoms-causes/dxc-20186931](https://www.mayoclinic.org/diseases-conditions/rotavirus/symptoms-causes /dxc-20186931) 10. Modern manifestations of the epidemic process of rotavirus infection and ways to optimize epidemiological surveillance, Vitaly Vyacheslavovich Kudryavtsev - [https://www.crie.ru/pdf/disser1(kudryavtsev).pdf] (https://www. crie.ru/pdf/disser1(kudryavtsev).pdf) 11. Diarrhoea and Vomiting Caused by Gastroenteritis: Diagnosis, Assessment and Management in Children Younger than 5 Years, NCBI - [https://www.ncbi.nlm.nih.gov /books/NBK63845/] (https://www.ncbi.nlm.nih.gov/books/NBK63845/)
Symptoms of rotavirus infection
Symptoms appear approximately 3-5 days after infection. As a rule, this happens very brightly and suddenly. Among them are:
- heat;
- chills;
- vomit;
- diarrhea;
- pain in the abdomen (especially in the navel area);
- dizziness;
- loss of appetite.
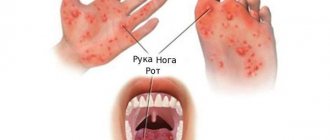
In some cases, the disease begins with sensations reminiscent of a cold: sore throat, nasal congestion, and a slight cough. After this, rotavirus infection manifests itself with intestinal symptoms and fever.
ON A NOTE! In most cases, rotavirus manifests itself as a monodisease. However, recently its combination with other infections has become increasingly common. This may be a viral-viral form of the disease, for example, with an enterovirus, or a viral-bacterial one (for example, with salmonella).
Signs and symptoms5
- Uncontrolled diarrhea is the most dangerous symptom of rotavirus gastroenteritis. In some cases, diarrhea leads to dehydration, which can in turn be fatal. 17.8% of deaths from diarrhea under 5 years of age are due to rotavirus infection.
- Excessive vomiting is another symptom that leads to dehydration.
- Severe stomach and intestinal cramps, flatulence.
- Dry cough, nasal congestion, sore throat are symptoms due to which, in the early stages, rotavirus infection can be confused with the flu or tonsillitis (sore throat).
- Conjunctivitis, enlarged lymph nodes.
- General weakness, apathy.
- Appetite disturbances - up to complete refusal to eat and drink in severe forms of the disease.
- Pale skin, dry mouth, chapped lips.
- Severe increase in body temperature.
Treatment methods
In its normal course, rotavirus infection can be treated on an outpatient basis, at home, under the supervision of a pediatrician. Hospitalization is required if very severe intoxication is observed, which threatens rapid dehydration of the child’s body.
For treatment use:
- enterosorbents;
- antiviral drugs;
- symptomatic drugs, for example, antipyretics;
- probiotics;
- antibacterial drugs (if necessary);
- special solutions that replenish the loss of microelements.
The main goal of therapy is to stop fluid loss, remove toxins, and normalize intestinal functions.
The prognosis for mild to moderate disease is most often favorable.
How dangerous is the infection?
Rotavirus infection primarily poses a danger to the child’s body, since the child has not yet developed resistance to dehydration, and it occurs faster than in an adult. In addition, according to experts, rotavirus, transmitted even in a mild form (especially repeated infections) can subsequently cause:
- gallbladder problems;
- secondary lactase deficiency;
- food allergies;
- functional disorders of the gastrointestinal tract.
In adults, the infection can cause complications from the endocrine and cardiovascular systems if they have chronic diseases, for example, diabetes mellitus, a tendency to blood clots. A healthy adult can contract rotavirus without consequences.
Preventive measures
Prevention of rotavirus consists of strengthening the immune system and observing hygiene rules. Regarding infants, this also includes breastfeeding. In addition, there is a vaccination against rotavirus infection.
How does vaccination help?
Vaccination against rotavirus is already included in the National Vaccination Calendar of the USA, Germany, France and some other countries. In Russia this is just being planned, so for now it can be done on a paid basis; Only the wishes of the parents are enough. And here it is important not to miss deadlines - now we will explain why.
There are 2 vaccines against rotavirus: Rotarix (monovalent) and RotaTek (pentavalent). The RotaTek vaccine is available in our country (Manufacturer: Merck Sharp and Dome B.V., the Netherlands). It helps fight rotaviruses of serotypes G1, G2, G3, G4 and serotypes G containing P1A[8] (for example, G9). The vaccine is a drinking solution (not an injection).
According to the instructions, the vaccination course consists of three doses with an interval between doses of 4 to 10 weeks. And now, as promised, we pay attention to the deadlines. The first vaccination is given no later than 12 weeks from birth! That is, active immunization of children is carried out between the ages of 6 and 32 weeks.
Why can't you vaccinate after 32 weeks?
As mentioned above, the instructions stipulate that the course of vaccination should be completed at 32 weeks, and the child should receive the first dose no later than 12 weeks of age. The effect of the vaccine at later stages of the course of vaccinations has not been studied, and in the absence of data on effectiveness and safety, the drug cannot be used.
Another common question is why a vaccine is not developed to vaccinate older children or adults. Perhaps such a vaccine will also appear someday, but for now it is only possible to vaccinate children. Yes, it is understandable that the vaccine was primarily developed for those who suffer this infection the hardest: children in the first years of life. A child's weak immune and digestive system cannot cope with intoxication, which leads to a severe course of the disease and complications. 3 doses of the vaccine are the conditional 3 first “meetings” with the virus. If the virus is real, i.e. wild - the consequences of such contacts are unpredictable, but if it is vaccine - it is transferred almost unnoticed. As a result of the vaccine, the child acquires immunity. It is valid for up to 5 years, that is, precisely the period when rotavirus is especially dangerous for humans.
About rotavirus infection, as well as about other vaccinations that are not included in the National Calendar of the Russian Federation, see our video (narrated by allergist-immunologist Natalya Nikolaevna Nagornaya):
For all questions related to rotavirus and vaccination, you can contact the specialists of our center. Sign up for vaccination now.
Rotavirus - treatment and prevention
Moiseeva Tatyana Sergeevna
Pediatrician, Infectious disease specialist
April 25, 2021
intestinal infections sooner or later. After acute respiratory viral infections (ARVI and influenza), this is the most common reason for visiting a doctor in childhood. They are a problem not only for the child, but also for the whole family. Perhaps the most common intestinal infection at the moment is rotavirus or, as parents often call it, “intestinal flu”.
Regardless of the social status of the family and the sanitary and hygienic situation in the house, from birth to 5 years, almost all children suffer from rotavirus gastroenteritis . According to statistics, more than 137 million people worldwide suffer from this infection every year, approximately a quarter of whom are hospitalized. Unfortunately, there are cases with fatal outcomes, including in children. Rotavirus gastroenteritis is most severe in children when they first encounter the virus, which usually happens between the ages of 6 and 18 months. In babies who are bottle-fed, the risk of infection and a more severe course is slightly higher.
Adults are also susceptible to this infection. You can become infected repeatedly during your life, since natural immunity to the virus is type-specific (it protects only against a specific type of rotavirus and does not protect against others). With repeated contact with the virus, the disease is usually less severe, but the person is contagious and can spread the infection.
So, what is rotavirus? There is an opinion that rotavirus got its name because it enters the human body through the mouth, this is not true, the virus is called that because its external structure resembles a wheel (from the Latin - rota), hence the name. There are several types, slightly different from each other in structure, but causing the same clinical picture of the disease.
The route of transmission of this infection is fecal-oral, that is, to put it simply, it is a “disease of dirty hands.” The virus is very contagious; just 10 particles of the virus are enough to make you sick. Rotavirus persists for a long time on any surface, even with thorough cleaning. Therefore, very often several family members, including adults, are sick with this infection at the same time, and outbreaks occur in children's groups. It is worth noting that you can only become infected from a sick person; pets do not get sick from “human” rotaviruses.
The incubation period for rotavirus infection ranges from several hours to 5-7 days. It is characterized by general malaise, weakness, refusal to eat, increased body temperature and symptoms of damage to the gastrointestinal tract (frequent watery loose stools, vomiting, abdominal pain). At the first signs of illness, you must seek medical help! After examining the child, the doctor will assess his condition, the need for hospitalization, and prescribe examination and treatment.
To diagnose the infection, stool testing for rotavirus is used using the PCR (polymerase chain reaction) and ELISA (enzyme-linked immunosorbent assay) method; the result is usually ready in 1-2 days. But treatment must begin at the first symptoms of the disease, without waiting for results. Therapy is carried out according to symptoms, and practically does not depend on test results. Tests are prescribed to make sure that it is a rotavirus infection and in case of complications, so that doctors understand what exactly they are dealing with.
To treat children who do not need hospitalization and remain at home under the supervision of a pediatrician, so-called pathogenetic therapy is used, aimed at replacing the fluid that the child loses during illness with loose stools and vomit.
The most important rule for a mother with rotavirus is to give her child a few sips every 5-10 minutes. If the child refuses, then feed him from a spoon or from a syringe (after removing the needle). You should not let your child drink large amounts of liquid at one time, even if they are very thirsty, as this may cause vomiting. You need to be patient and constantly, despite the protests, give him water, water, water. It is desoldering that helps avoid dehydration and hospitalization.
In addition to water, special saline solutions from the pharmacy are used to water the child, containing salts that are lost by the body during illness (Hidrovit, Humana, Electrolyte, Gastrolit, Regidron, etc.). In the absence of special drugs, you can use a homemade solution until you purchase them. You can prepare it by taking a liter of boiled water, adding 1-2 tablespoons of sugar (without a slide), half a teaspoon of table salt and one-third of a teaspoon of baking soda. The prepared solution can be stored for no more than a day. Children should not be fed with milk, juices, fruit drinks, vegetable broths, or carbonated drinks.
The second important component of the treatment of rotavirus infection is diet therapy . During the acute illness and 2-3 weeks after it, the child is prescribed a gentle diet, with the exception of dairy products, juices, raw fruits and vegetables. The child should eat more often than usual, in small portions. Food should be as gentle as possible on the stomach - not spicy, not fatty, not hot, not fried.
For young children who are breastfed or bottle-fed, the issue of further feeding is decided individually with a pediatrician. If frequent loose stools persist in bottle-fed children, the option of temporarily switching to a formula with a reduced lactose content (lactose-free, low-lactose, etc.) is possible. For infants, the issue of partially replacing breast milk with a formula with a reduced lactose content or adding special enzymes to breast milk that help the milk to be absorbed in the baby’s intestines (lactase enzyme preparations) is being resolved.
Also used in therapy are such groups of drugs as: enterosorbents (Smecta, Filtrum-sti, Enterosgel, etc.), probiotics (Enterol, Linex, Bifiform, Acipol, etc.), prebiotics (Hilak-forte, Duphalac, etc.), enzymes (Creon 10000, Mezim-forte, Pancreatin). You should not give these drugs to your child on your own; you should consult a doctor, as you need to understand the advisability of taking them at different periods of the disease.
, antiviral and immunomodulatory therapy can be carried out . The decision to prescribe drugs in this group is made only by the doctor.
Antibacterial therapy is worth considering separately. Antibacterial therapy is not carried out for uncomplicated rotavirus infection. But in some cases, doctors still prescribe antibiotics. And it's not just a matter of habit. This is due to the fact that acute intestinal infections are not only of a viral nature, but also of a bacterial nature (Escherichia coli, Salmonella, Yersinia and some others). And it is not always possible to determine with 100% accuracy from the symptoms what caused the symptoms: a viral infection, a toxic infection or a bacterial one. There are also mixed causes and atypical course of the disease, so the issue of prescribing antibacterial drugs remains at the discretion of the attending physician.
Very important! If watering the child turned out to be ineffective and the child continues to vomit, weakness increases, he urinates less than usual (the interval is 3-4 hours), then there are direct indications for hospitalization of the baby in a hospital, where he will be prescribed infusion therapy (intravenous fluid).
Currently, there is a unique opportunity to protect your baby from rotavirus infection . The Rotatek® vaccine has been certified in Russia and has been successfully used abroad for several years. The vaccine protects against the five most common types of rotavirus and prevents severe forms of other types of the virus. For a full course of vaccination, 3 vaccines must be administered. The convenience of using the vaccine lies in the fact that it is presented in the form of drops for oral administration, and not in the form of a syringe for intramuscular injection. The first dose of the vaccine is at 6-12 weeks of age, then 2 more at an interval of at least 4 weeks. Revaccinations, that is, repeated injections of the vaccine after a full course of vaccination from 3 stages, are not required.
The vaccine is intended for children from 6 weeks to 32 weeks , and is not used in adults. This is due to the fact that the first encounter with the virus and the most severe course of the disease occurs during this period. In the future, after the immune system has become “acquainted” with the virus, the likelihood of developing a serious illness decreases and immunoprophylaxis with a vaccine is no longer so relevant.