Pharmacological properties of the drug Calcitriol
An active metabolite of vitamin D3, it is formed in the kidneys from its precursor 25-hydroxycolecalciferol. Promotes the absorption of Ca2+ in the intestine, regulates bone mineralization, stimulates the activity of osteoblasts. It is quickly and almost completely absorbed from the gastrointestinal tract when taken orally. The maximum concentration in blood plasma when taken orally at a dose of 1 mcg is achieved after 4–6 hours. Metabolized to form active metabolites. The half-life is 3–6 hours, however, due to its high lipophilicity, calcitriol and its metabolites can partially accumulate in adipose tissue, and therefore the pharmacological effect can last up to 3–5 days. Excreted in bile. Subject to enterohepatic recirculation.
What is Vitamin D?
What does Vitamin D have to do with joint diseases?
Vitamin D takes an active part in the formation and maintenance of the quantity and quality of bone tissue.
Story.
Since opening in 1913. interest in this vitamin changed from an ordinary vitamin to a hormone, taking into account ultra-modern views on metabolic processes in the body and the formation of diseases.
In 1928 A. Windaus was awarded the Nobel Prize for isolating vitamin D and establishing the structure of plant steroids.
Vitamin D has been studied for more than 100 years, and no one can say that they know everything about it.
Professor M. Holik, a global authority and expert on the problem of vitamin D deficiency, points out that up to 80% of humanity suffers from vitamin D deficiency. The level of deficiency is well below critical, everyone is at risk!
Theory.
What is Vitamin D?
Vitamin D is presented in the main natural forms:
— D2 (ergocalciferol), found in food products, supplied up to 20% of the requirement;
— D3 (cholecalciferol) is formed in the body from a precursor found in the skin.
(7-dehydrocholesterol) under the influence of ultraviolet irradiation from sunlight. This transformation occurs short-term and not permanently.
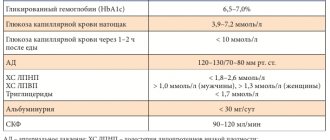
Vitamin D (D2 (ergocalciferol) supplied with food and D3 (cholecalciferol) converted in the skin) as a result of the 25-hydroxylation reaction in the liver is converted into 25 (OH) D, which very quickly leads to its increase in the blood serum. The level of this substance reflects both the formation of vitamin D in the skin and intake from food and is used as a marker of vitamin D status (the transport form has no effect). In the human body, the main part of 25(OH)D is hydroxylated in the tubules of the renal cortex, slightly in blood cells and bone tissue, turning into 1α25-dihydroxyvitamin D3 (the active metabolite is calcitriol). Partially the transport form of 25(OH)D enters adipose and muscle tissue, forming a depot.
More than 99% of the resulting active metabolite of vitamin D3 enters the blood, where it binds to a transport protein and enters target organs and interacts with specific vitamin D receptors (VDR).
Specific vitamin D receptors (VDRs) are present in 37 organs and tissues, not only in the classic target organs for vitamin D - in the intestines, kidneys, bones, but also in the brain, heart, pancreas, parathyroid and prostate glands, excretory and reproductive system, immune, musculoskeletal, respiratory, endocrine systems, connective tissue, etc.
The active metabolite of vitamin D - calcitriol - has a powerful genomic effect, activating more than 2727 genes in target cells, providing an effect on RNA and DNA, in particular, encodes the formation of proteins involved in the implementation of long-term (hours, days) effects of vitamin D: osteocalcin and osteopontin - in osteoblasts, integrin - in osteoclasts and blood macrophages.
Vitamin D binds to the specific vitamin D receptor (VDR), which regulates the expression of many genes, including the ion channel genes TRPV6 (ensures the absorption of calcium in the intestine), CALB1 (calbindin; ensures the transport of calcium into the bloodstream), BGLAP (osteocalcin; ensures bone mineralization tissue and calcium homeostasis), SPP1 (osteopontin; regulates osteoclast migration), REN (renin; regulates blood pressure, being a key element of the RAAS), IGFBP (insulin-like growth factor binding protein; enhances the action of insulin-like growth factor), FGF23 and FGFR23 (growth factor fibroblasts 23; regulate the levels of calcium, phosphate anion, processes of cell division of fibroblasts), TGFB1 (transforming growth factor beta-1; regulates the processes of cell division and differentiation of osteocytes, chondrocytes, fibroblasts and keratinocytes), LRP2 (LDL receptor-related protein 2 ; is a mediator of endocytosis of low-density lipoproteins), INSR (insulin receptor; ensures the effects of insulin on any cell type).
The active metabolite vitamin D has a non-genomic effect through membrane cell receptors, causing rapid, within a minute, physiological and biochemical reactions, activating tubular channels, regulating ionic currents, stimulating the transport of Ca+ ions, muscle contraction, etc.
Let's move from theory to practice!
In our center, 277 people diagnosed with aseptic necrosis of the femoral head (154 women and 123 men) were examined to determine the indicators of the vitamin D metabolite (25(OH)D.
The data is simply terrifying...