“Faty liver” is a disease that is characterized by excessive accumulation of fat in the liver cells.1 This disease has several names - fatty liver, steatosis, fatty degeneration, but each of them means only one thing - it is not to be trifled with, and its early diagnosis, as well as subsequent treatment, must be timely and comprehensive.
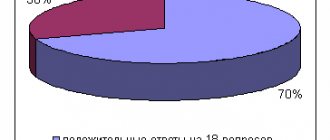
To begin with, it is worth remembering that fatty liver disease can be associated with alcoholic or non-alcoholic liver damage.2 Next we will talk about non-alcoholic damage. Recently, the number of patients with non-alcoholic fatty liver disease (NAFLD) has increased significantly. Thus, according to statistics, in 2007 NAFLD was detected in 27% of patients, while in 2014 this figure increased to 37%. Thus, NAFLD currently ranks first in frequency among chronic liver diseases.1
Risk factors for the development of steatosis 1.3
- Obesity or overweight, with a body mass index of 25 or higher
- Type 2 diabetes mellitus or decreased insulin sensitivity
- Lipid metabolism disorders, in particular dyslipidemia
- Metabolic syndrome
- Age 30 – 59 years
- Physical inactivity
- Binge eating
Classification
By etiology:
- primary or secondary. Secondary develops as a complication of other diseases (diabetes mellitus, obesity, hormonal disorders, etc.). Primary occurs due to poor nutrition, genetic predisposition, etc.;
- alcoholic or non-alcoholic. Alcoholic hepatosis appears against the background of regular consumption of toxic doses of alcohol. Non-alcoholic can be caused by any other reasons not related to the toxic effects of ethanol.
By distribution:
- focal fatty degeneration, in which a local area of liver tissue is affected;
- diffuse hepatosis, in which the affected area affects all tissues of the organ.
By stage:
- 0: damage to single hepatocytes or small groups of them;
- 1: the appearance of medium-, large-droplet fat cells that provoke inflammation;
- 2: intracellular obesity of a diffuse nature;
- 3: extracellular obesity, damage to large droplet fat cells, cyst formation.
Why is NAFLD dangerous?
Fatty hepatosis, especially at the very beginning, can be practically asymptomatic, and the existing symptoms are not specific and, thus, make diagnosis difficult. However, you should not relax - diagnosing fatty hepatosis is important for any suspicion of the presence of this disease. Because this disease, developing gradually, practically without manifesting itself clearly, nevertheless increases the risk of cardiovascular death several times - in other words, it increases the risk of developing strokes and heart attacks.4 In addition, advanced fatty hepatosis can ultimately lead to ultimately, to the development of cirrhosis and liver failure. The likelihood of this event is low, however, if it occurs, the consequences can be fatal. The fact is that cirrhosis usually requires organ transplantation, which can be further complicated in the presence of cardio-metabolic disorders and diseases that often accompany fatty hepatosis.3
Stages of development of NAFLD
- 1
Stage of fatty hepatosis (steatosis)
The initial stage of the disease, often asymptomatic
- 2
Non-alcoholic steatohepatitis
Hepatosis with accompanying inflammation of liver cells
- 3
Fibrosis with further transition to cirrhosis
At this stage, liver tissue begins to be replaced by connective tissue, which leads to disruption of the structure and, ultimately, disruption of the organ.3
What kills a patient with untreated fatty liver: heart attack or cirrhosis?
Fatty liver disease, as fatty liver is also called, is combined with the deposition of fat on the walls of the arteries, and, as a result, accelerates the development of cardiovascular accidents. If fatty liver disease is not treated, it turns into fibrosis, when connective tissue, in other words, a scar, is formed instead of the “workhorses” - liver cells. This is how cirrhosis gradually develops. And these are the consequences of loving sweets, fatty foods, strict diets, “relaxing” with a glass of beer in hand or something stronger.
But the liver is an amazing organ, and the process can be reversed if we start paying attention to ourselves in time.
What are the signs of fatty liver disease?
As we mentioned above, the main feature of this condition is the absence of specific symptoms. Therefore, the disease is often detected by chance, often during a routine medical examination or examination for a completely different disease.
Among the symptoms that often occur with fatty hepatosis, but can be ignored, you should pay attention to:
- Discomfort in the area of the right hypochondrium, without a clear connection with food intake
- Fatigue
- Weakness
If these symptoms are detected and there is concern about the condition of the liver, then to clarify the diagnosis, you should consult a doctor who can prescribe a diagnostic method such as ultrasound. Ultrasound will help identify increased liver volumes and changes in the echogenicity of the organ. The doctor may also recommend testing liver enzymes - ALT, AST. In some cases, a specialist may see the need for a liver biopsy (examination of liver tissue under a microscope), which provides the most reliable information about the condition of the organ.1,4
Symptoms
The danger of non-alcoholic hepatosis is its asymptomatic course. The disease does not manifest itself in any way until the damage to hepatocytes becomes serious. At stages when the process is reversible and treatment does not require serious efforts, fatty liver degeneration has no symptoms and can only be diagnosed by consulting a doctor.
As hepatosis develops, symptoms appear:
- decreased performance, fatigue, frequent weakness;
- a feeling of discomfort or heaviness in the hypochondrium on the right side, gradually turning into pain;
- loss of appetite or attacks of hunger with rapid satiety when eating;
- nausea and then vomiting, which becomes regular, contains bile;
- the skin, mucous membranes, and whites of the eyes may acquire a yellowish tint;
- itching of the skin may occur;
- immunity gradually decreases, a person suffers from colds more often.
How to treat fatty hepatosis?
The earlier the diagnosis is made, the better. To avoid serious consequences, it is better to treat fatty hepatosis at an early stage - steatosis. When treating hepatosis, if possible, exclude the action of those factors that can affect the condition of the liver. The treatment regimen must include proper nutrition and diet (in the case of alcoholic hepatosis, strict cessation of drinking alcoholic beverages).
Patients with fatty hepatosis should adhere to the so-called Mediterranean type of diet: eat a lot of fish, avoid fatty meats, and limit the consumption of sugary drinks and foods containing simple carbohydrates. At the same time, you need to increase your consumption of foods high in dietary fiber, such as fruits (taking into account their calorie content) and vegetables.1
In addition to proper nutrition, it is worth changing your lifestyle in general. Move more, follow the regime and daily routine, and find a place in it for daily physical activity. For example, swim, ride a bike, or just walk at a moderate pace for at least 20 minutes and at least 5 times a week.1
Drug therapy for hepatosis may include taking drugs from the group of essential phospholipids, which in case of fatty liver have anti-inflammatory, antioxidant and membrane-stabilizing effects.5 And, of course, if you have any concerns about your health, consult a doctor and do not forget to monitor the condition of the liver - one one of the most important organs in our body!
Old and new approaches to the treatment of non-alcoholic fatty liver disease
Total duration: 16:20
00:00
Presenter: Now with great pleasure I present to everyone a well-known colleague, Professor Alexey Olegovich Bueverov, who will introduce us to modern approaches to the treatment of various forms of non-alcoholic fatty liver disease.
Alexey Olegovich Bueverov, Doctor of Medical Sciences:
— Dear Chairman, dear colleagues.
Non-alcoholic fatty liver disease today has already replaced such common liver pathologies as alcoholic liver disease and viral hepatitis in economically developed countries, taking first place in prevalence.
Indeed, the prevalence of non-alcoholic fatty liver disease in the general population reaches 20%. The likelihood of non-alcoholic steatohepatitis is significantly lower, but still this is not a small figure. In obese patients it reaches 75–100%. The frequency of non-alcoholic steatohepatitis is 25 – 75%.
If we take the population of patients with type 2 diabetes mellitus, non-alcoholic fatty liver disease occurs on average in 60% of cases. Recently, data were published showing that 6.3% of men and 2.6% of women (patients with type 2 diabetes mellitus) die from liver cirrhosis as a result of non-alcoholic steatohepatitis, and not from cardiovascular diseases, which are as the leading cause of death in such patients.
In 1998, two renowned researchers, Oliver James and Christopher Day, proposed a “two-hit” theory for the development of non-alcoholic fatty liver disease. The first blow is the development of steatosis, the second blow is the development of steatohepatitis.
Just recently, these same authors have been very skeptical about this theory. Clinical practice shows that in most patients, steatosis remains steatosis for the rest of their lives, without leading to the development of significant inflammation. With the development of steatohepatitis, steatosis and inflammation usually progress simultaneously. Perhaps in the near future the concept of “two strikes” will be replaced by the concept of “one strike”.
It is well known that adipose tissue cells - adipocytes - are biologically very active cells. They produce a huge number of different substances that affect a variety of parts of the life of the cell and various tissues. In particular, tumor necrosis factor α, a well-known pro-inflammatory, propathogenic cytokine, can lead to impaired phosphorylation of the insulin receptor.
As a result, disruption of a number of intracellular processes leads to a decrease in glucose entry into the cell due to a decrease in the activity of the glucose transporters GLUT-4. As a result, the development of insulin resistance, which underlies both non-alcoholic fatty liver disease and the initial stages of type 2 diabetes mellitus.
03:22
With obesity, adipose tissue cells not only increase in size, but also undergo apoptosis in greater numbers than normal. In addition, macrophages and other inflammatory cells are attracted to adipose tissue. As a result, a so-called cellular dialogue develops, which is carried out through the interaction of various cytokines with the corresponding receptors.
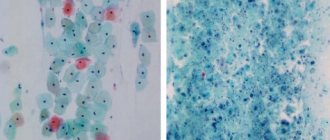
A well-known diagram demonstrating the effect of lipid peroxidation as a result of the formation of reactive oxygen species. It is typical for both non-alcoholic steatohepatitis and alcoholic steatohepatitis. We see almost identical changes in the histological specimen (death of hepatocytes by apaptosis and necrosis, formation of Mallory bodies, varying degrees of fibrosis (up to sarotic transformation) and infiltration of polymorphonuclear leukocytes (PMN) .
At the Immuno-thematic Conference of the European Association for the Study of the Liver, which took place in Bologna in September 2009, several reports were devoted to the question of which patients still need a liver biopsy.
Histological studies remain the gold standard in the diagnosis of non-alcoholic steatohepatitis. Considering millions of such patients, experts suggest primarily using this invasive method in motivated patients (patients with type 2 diabetes mellitus with android obesity and even a borderline platelet count, a high level of insulin resistance and any indirect signs of liver cirrhosis).
Non-invasive risk factors for the progression of non-alcoholic steatohepatitis include:
- older age (over 50 years old);
- presence of obesity;
- type 2 diabetes;
- arterial hypertension;
- hypertriglyceridemia;
- the ratio of aspartic transaminase to alanine is greater than one (according to some other data, more than 1.3);
- infection with the hepatitis C virus, which itself acts as an independent factor in the development of liver steatosis.
05:46
There are two known parts of the pathogenesis of non-alcoholic steatohepatitis: insulin resistance and oxidative stress. They dictate the theoretical possibility of using appropriate treatment methods. With regard to insulin resistance, this means following a hypoglycemic diet, prescribing the drug Orlistat (which will be discussed in more detail), physical activity and prescribing insulin sensitizers.
Regarding oxidative stress. These are primarily drugs of the antioxidant group, also possibly anti-cytokine drugs and drugs with hypolipidemic action.
As for weight loss, of course, it is indicated for all patients who are not only obese, but also overweight, not yet reaching the stage of obesity. Their approaches are well known. This is a low-calorie diet and physical activity.
Practically the only remaining approved drug in most countries is Orlistat. Finally, a patient with morbid obesity undergoes gastroplasty. Weight loss must be gradual. Very rapid weight loss can lead to a decrease in steatosis, but a simultaneous progression of inflammation primarily due to the release of free fatty acids and progression of liver fibrosis.
A meta-analysis of 29 liver studies with a follow-up period of at least 2 years demonstrated that intense physical activity leads to a significant reduction in body weight. They are significantly more effective than even a very low-calorie diet.
Another question is that such recommendations cannot practically be given to all patients. For example, a patient with a high cardiovascular risk, of course, should exercise in doses.
07:45
Interesting data have now been accumulated on long-term therapy of the drug Orlistat, well known under the name Xenical. "Xenical" is a drug that inhibits intestinal triglyceride lipase.
It is prescribed in a standard dose, regardless of body weight - 120 mg 3 times a day with meals or within one hour after meals (meals that contain a certain amount of fat). One-year, and even more so four-year treatment with Xenical significantly exceeds the effectiveness of weight loss using a hypocaloric diet. It turns out that long-term therapy with Xenical leads not only to a decrease in body weight, but also to an improvement in lipid status, a decrease in total cholesterol and the atherogenic fraction of low-density lipoprotein cholesterol.
Data published in the last 1.5 - 2 years indicate that the mechanism of action of Orlistat (perhaps even the key one) is the effect on adiponectin. A number of studies have shown that with a loss of more than 5% of body weight during treatment with Xenical, there is a significant increase in the level of serum adiponectin. With a loss of more than 9% of body weight, an increase in adiponectin clearly correlates with a decrease in the severity of steatosis, balloon degeneration and the activity index of non-alcoholic steatohepatitis according to puncture biopsy.
09:28
Studies were conducted directly with Orlistat for non-alcoholic steatohepatitis. Even a short six-month course of treatment with Xenical at a standard dose of 120 mg three times a day leads to a decrease in steatosis, a decrease in alanine transaminase levels, insulin resistance, cholesterol, triglycerides and low-density lipoprotein levels.
Another study (although it contained a small number of patients - only 14) demonstrated, along with an improvement in other histological parameters, also a decrease in fibrosis. Moreover, in three patients the decrease in fibrosis was two points compared to the baseline according to the paired biopsy.
Other drugs that increase insulin sensitivity are primarily represented by Metformin (an activator of adenosine monophosphate-dependent protein kinase) and thiazolidinediones, of which only Pioglitazone remains on the market.
Rosiglitazone has been withdrawn from the market in most countries due to an increased risk of cardiovascular complications. It should be remembered that these drugs can be prescribed to patients who do not have diabetes mellitus, since they extremely rarely cause glypoglycemia.
Studies with Metformin, in particular with the drug Glucophage, indicate that its administration leads to a decrease in the severity of steatosis and necroinflammatory activity. In the Bugianesi study, it reduced fibrosis. Metformin leads to normalization of alanine transaminase or a slight decrease in its level in patients who are not on a diet, and the effect of diet and the use of Ursodeoxycholic acid.
Another study demonstrated that a year's administration of Metformin leads to improvement in insulin resistance, normalization of glucose levels and normalization of adiponectin levels.
Another insulin sensitizer from a different group is Pioglitazone. There was a large study called Pivins, where Pioglitazone was compared with vitamin E 800 mg per day or placebo. It demonstrated greater reductions in steatosis and lobular inflammation compared with vitamin E or placebo. The dynamics of fibrosis in these patients was not reliable, despite the fact that the study lasted almost 2 years.
12:09
“Pentoxifylline” – an inhibitor of tumor necrosis factor synthesis? – has serious side effects when used in large doses. It is in these doses that it is used for non-alcoholic and alcoholic steatohepatitis, which significantly limits its use. Early studies demonstrated both biochemical and histological dynamics during the use of Pentoxifylline. More recent studies demonstrate a lack of histological effect, making the drug's prospects in patients with nonalcoholic steatohepatitis questionable, at least in the near future.
"Ursodeoxycholic acid." The most famous study here is “Ratzui”, which was published in 2009, demonstrating a statistically significant decrease in the levels of alanine and aspartic transaminases, as well as gamma-glutamyl transpeptidase.
However, the Leuschen study published last year only showed a reduction in lobular inflammation. However, the authors note that the best results from the use of Ursodeoxycholic acid were observed in men under 50 years of age with slight excess body weight and the presence of arterial hypertension.
"Adenosylmethionine." Here you can refer to domestic experience. This is a study by Professor A. Yu. Baranovsky from St. Petersburg. Unfortunately, it was carried out without a histological assessment of the liver. However, the use of Heptral for 6 months at a dose of 1200 mg per day led to normalization of transaminases in the vast majority of patients. The effect was achieved very quickly.
As an additional effect of using Adenosylmethionine, a decrease in serum cholesterol levels was noted during six-month therapy with this drug. This allows it to be considered as a promising drug for the treatment of patients with non-alcoholic fatty liver disease.
14:20
Data from a very large number of studies have been obtained on non-alcoholic fatty liver disease. The large number of these studies is due to the fact that this problem is extremely relevant, primarily in view of the wide prevalence of this nosological form.
What conclusion can be drawn about the most effective treatment method? Unfortunately, an unambiguous conclusion cannot be drawn today. Of course, these patients (especially those with signs of metabolic syndrome) are indicated for lifestyle modification, represented by diet and adequate physical activity.
Unfortunately, long-term maintenance is difficult, sometimes for objective, sometimes for subjective reasons. Medicines such as Orlistat, insulin sensitizers, Metformin and Pioglitazone, antioxidants, anti-cytokine and lipid-lowering drugs, which I did not dwell on. There are some studies that suggest that lipid-lowering drugs such as statins and fibrates may also be effective in treating non-alcoholic steatohepatitis in some patients.
The research results to date are contradictory. Studies on the effect of Orlistat (the drug Xenical) demonstrate that the drug helps not only to reduce and maintain body weight, but also in a number of studies to improve the biochemical and histological picture.
Thus, today we can conclude that patients with non-alcoholic fatty liver disease require a complex of therapeutic measures, taking into account the individual characteristics of the disease and comorbidity. Evaluating the effect of a particular drug or combination of drugs appears to require many years of research.
Thank you for your attention.
16:20
Diet features
General recommendations for diet for fatty hepatosis:
- Refusal of alcoholic beverages;
- Limiting fatty, fried, smoked, sweet foods;
- Food at least 3 times a day;
- Increase fluid intake per day;
- Baked, boiled, steamed food;
- Increase in the diet of vegetables and seafood;
- A sufficient amount of calories in the diet (moderate deficit if necessary to lose weight);
- Limiting salt in the diet to 6-8 g per day;
- Limiting spices and spicy foods.
Following a healthy diet early in the course of the disease can be a key component of treatment.
Diagnostics
Fatty liver disease is often found in people who are overweight or have insulin resistance (diabetes).
Diagnostics for liver dystrophy are also carried out for people who have systematically consumed or are consuming alcohol. In rare cases, pathology is detected due to a patient’s complaint about liver function. The diagnostic complex, in addition to standard questioning and examination, includes:
- General blood analysis;
- Blood chemistry;
- Coagulogram;
- Blood glucose level;
- Glucose tolerance test;
- Lipidogram;
- Ultrasound examination of the liver;
- Computed tomography of the abdominal organs (with or without contrast) or magnetic resonance imaging;
- Liver biopsy;
- Elastography.
The research results make it possible not only to confirm dystrophic changes in the liver, but also to assess their severity and identify the most likely causes. Diagnosis is carried out by a gastroenterologist or a more specialized specialist - a hepatologist. Only after confirming the diagnosis and identifying the exact causes of the disease, a treatment plan is developed.
Causes
The accumulation of fatty molecules in liver cells is due to either their excessive intake or impaired excretion. Risk factors for this process may include:
- Overweight;
- Impaired glucose tolerance or diabetes mellitus;
- Hereditary predisposition;
- Taking medications (corticosteroids, oral hormonal contraceptives, NSAIDs, antibiotics, cytostatics);
- Dyslipidemia and atherosclerosis;
- Disorders of the thyroid gland;
- Adrenal gland disorders;
- Hypertension, coronary heart disease;
- An unbalanced diet with an excess of fats, fried foods, simple carbohydrates;
- Lack of physical activity.
Separately, fatty hepatosis is distinguished as part of the general mechanism of development of alcoholic liver disease. In this case, ethanol consumption is a key factor in the disruption of the structure of hepatocytes and the development of dystrophic changes.
How does the disease manifest itself?
At first, the disease is asymptomatic. Over time, it causes liver failure, which can take years or decades to develop. The first signs appear with significant fatty liver, which causes:
- weakness;
- confusion;
- redness of the palms;
- fatigue;
- yellowing of the sclera, skin;
- dyspepsia (nausea, vomiting);
- expansion of subcutaneous vessels;
- loss of appetite and weight loss;
- ascites (accumulation of fluid in the abdominal cavity).
Treatment tactics for patients with NAFLD and metabolic syndrome due to hepatitis C
If concomitant liver damage is detected in patients with HCV as a result of metabolic syndrome (non-alcoholic fatty liver disease - steatosis), it is necessary to conduct additional examination for indicators of metabolic and hormonal disorders characteristic of this disease.
To assess the degree of liver damage, it is recommended to use a blood test - Fibromax, which makes it possible to separately assess the degree of liver damage by the virus and separately by metabolic syndrome.
Treatment tactics depend on the degree of liver damage as a whole, and separately for each damaging factor. Treatment with antiviral drugs can be started immediately, and further treatment of metabolic syndrome after receiving SVR.
If the degree of liver damage from the virus is significantly less than from metabolic syndrome, it is possible to begin antiviral therapy after treatment of metabolic syndrome.
In cases of concomitant liver diseases, it is necessary to set the goal of treatment not only to obtain SVR, but also to preserve and restore the liver damaged by other pathological factors.
The most important component of successful treatment of NAFLD and fatty liver disease is proper nutrition.
up
How can we help you?
Examine . Ultrasound and elastography will show how much the liver tissue has changed, whether there is fibrosis, and the analyzes will make it clear whether there are disorders of fat and carbohydrate metabolism. If ultrasound results reveal fatty liver, the hepatologist will recommend testing for viral hepatitis. Viral hepatitis often occurs under the guise of fatty liver.
The liver does not hurt, fat accumulates unnoticed. Think about it before it's too late. Get examined and make sure everything is ok. And if a problem exists, do not close your eyes to it and seek help. We are ready to help.