New possibilities for using Venlaxor for the treatment of depression in general medical practice
T.V. Reshetova, T.N. Zhigalova
St. Petersburg Medical Academy of Postgraduate Education, St. Petersburg
Depression is one of the most common mental disorders. At various periods of life, it occurs in 10% of the population, and taking into account minor forms, the frequency of depression in the population increases to 25%. However, only a quarter of such patients are seen by psychiatrists and psychotherapists, the rest are treated by general practitioners.
According to WHO forecasts, by 2021 depression will become the most important factor in disability throughout the world. It should be noted that views on depression are quite different: at different social levels, the same suffering is considered a disease, a consequence of bad upbringing, the sin of despondency, an obsession, a habitual inconvenience or a character trait. Cyclic mood swings in patients in general medical practice sometimes do not reach the level of psychotic maladaptation, but during “bad periods” (for several weeks or months), a person feels lethargy, loss of strength, is burdened by human society, preferring loneliness and inactivity. Appetite and assessment of personal qualities change in tune with mood, and the desire for new acquaintances decreases. By the patient and the doctor, this may be regarded as a decrease in mood associated with life difficulties or illness, but, from the point of view of a psychiatrist, such a condition is subject to diagnosis according to the criteria for depression from ICD-10.
In modern literature, views on mild forms of depression are very contradictory. Some authors consider latent depression to be the equivalent of situational maladaptation, others treat it as a psychiatric disease, emphasizing that insomnia, tachycardia, and autonomic dysfunction do exist in the patient; This is not a delusion of illness, since patients do not insist on their own assessment of health, but one of the clinical manifestations of depression. According to another opinion, latent (somatized, vegetative) depression, “depression without depression” is a link between mental and somatic diseases. According to the ICD-10 criteria, many “everyday” situations encountered in general medical practice should be classified as depression of varying severity and, therefore, may require treatment with antidepressants depending on the register of the lesion and the level of depression.
In general medical practice, in contrast to psychiatric services, “depression is more occupied with its body than other borderline disorders,” and patients actually present depressive complaints less frequently. The core syndrome in the clinic of a depressive state for an internist is often subthreshold asthenia, observed in 60-90% of patients, and only then depression. Somatic suffering or functional pathology of organs, as a rule, comes to the fore, and a decrease in mood is regarded by patients and doctors as an understandable reaction to the disease.
Somatogenic depression caused by the clinical picture of severe somatic illness deserves special attention. Their distinctive feature is the reduction of psychopathological symptoms in parallel with somatic improvement. In general medical practice, patients more often complain of anxiety, rather than of decline, which develops against a vital-asthenic background; half of the patients have suicidal thoughts and fear of death. Pain is the main complaint that the patient usually presents. However, with depression it is not even pain, but a painful, disturbing feeling in some specific place, a painful feeling of heaviness, discomfort, a syndrome of fear and anticipation of future pain.
In 31% of patients, a history of ambulatory depressive phases was assessed by general practitioners as vegetative-vascular dystonia, neurosis or osteochondrosis. At the same time, the patients had characteristic symptoms that allowed the internist to suspect depression behind the somatic facade of the disease: memory deterioration (except for memory for unpleasant things), forgetting successes and updating failures, a change in the sense of time and time perspective (life for today), difficulties in accepting the most ordinary decisions, especially simultaneous fear of doing and not doing something (for example, fear of taking a medicine because of side effects and not taking it because of the risk of worsening the course of the disease - “both are worse”), self-doubt, hyperesthesia in relation to strong or prolonged stimuli, difficulty forming concepts.
Many different schemes have been proposed for the correction of a depressive state in the clinic of internal diseases using drugs from the group of antidepressants. However, data from long-term follow-up studies indicate that in 25% of cases, patients develop persistent asthenic-depressive or depressive-hypochondriacal syndrome, both with and without the most intensive treatment of depression. Two thirds of patients in general medical practice, for various reasons (lack of information about the consequences, financial problems, self-medication), complete treatment for depression without completing the required course of therapy. This leads to rebound syndrome and the formation of resistance. It was the growth of resistant depression and the need to replace complex combined treatment of depression (drugs of several groups) with one drug that became the prerequisite for the creation of new antidepressants with a combined effect.
The latter include, in particular, Venlaxor. Venlaxor inhibits the reuptake of serotonin and norepinephrine, and is also a weak inhibitor of dopamine reuptake and weakens b-adrenergic reactions. Venlafaxine blocks serotonin reuptake approximately 5 times more strongly than norepinephrine reuptake. The degree of influence on neurotransmitter systems depends on the prescribed dose of venlafaxine: in small doses it only affects the uptake of serotonin; in medium and large - is an inhibitor of the reuptake of serotonin and norepinephrine; in very large cases, it blocks the reuptake of dopamine, serotonin and norepinephrine with equal effectiveness.
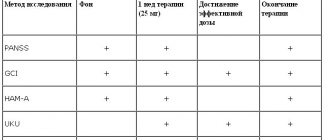
A serious issue is the time of onset of the effect. The effect of most known antidepressants usually appears in the third week of treatment. By this time, the doctor and the patient are relieved to note positive changes in the condition, and side effects are decreasing. The antidepressant effect of Venlaxor is detected somewhat earlier. Thus, in patients suffering from major depression from 6 months to 10 years, treatment with Venlaxor at a dose of 75-225 mg/day led to a significant improvement in the condition starting from the 7th day of therapy. The first response to treatment with Venlaxor was noted already on the 2-3rd day of use and was described by patients as a feeling of comfort. Significant changes in the PANSS, Beck, Hamilton and Taylor scales were observed in the 2nd week of therapy. In schizophrenia, the onset of the therapeutic effect, assessed on the PANSS scale, was observed from the 2nd week from the start of treatment with Venlaxor.
The rapidity of achieving an initial clinical response leads to a reduction in the risk of suicide, the frequency of treatment refusals and the number of hospitalizations in outpatients. Meta-analyses revealed the same effectiveness of venlafaxine with the most powerful tricyclic antidepressants and its advantage over selective serotonin reuptake inhibitors.
A high level of therapeutic response in the treatment of symptomatically different depressions has been demonstrated with the use of Venlaxor both in monotherapy and when combined with other drugs. Venlaxor has been noted to be highly effective in severe depression. The best results were obtained in patients with recurrent depression and bipolar affective disorders.
It should be noted that effectiveness is not the only necessary characteristic of therapy provided to patients with depression. Its tolerability is also the most important factor, especially in the treatment of somatogenic depression, in which patients are forced to take a large number of medications for somatic pathology.
Venlaxor is well tolerated. Side effects, if they develop, are more often observed at the beginning of therapy and usually disappear during the first week of treatment. The spectrum and severity of side effects are dose-dependent. When using venlafaxine in small and medium doses, it is possible to develop side effects inherent in all antidepressants from the group of selective serotonin reuptake inhibitors: dry mouth, nausea, insomnia, loss of appetite, fatigue, agitation, headache. Some side effects (decreased appetite and body weight) can be rationally used to treat related associated disorders (for example, eating disorders and nutritional obesity, which are often associated with depression).
When venlafaxine is prescribed in large doses, noradrenergic effects are possible: nausea, vomiting, sinus tachycardia, transient increase in blood pressure. If patients with somatic pathology (myocardial infarction or unstable angina in history, epilepsy, mania, glaucoma, renal or hepatic failure) require high doses of venlafaxine - more than 200 mg / day, it is necessary to monitor liver and kidney function, blood pressure levels during treatment and heart rate.
The good tolerability of Venlaxor with long-term use at a dose of 75 mg/day is confirmed by the absence of side effects in 95% of patients with post-stroke depression and an improvement in the quality of life of patients who have suffered a stroke.
Venlaxor (venlafaxine) is a drug for the treatment of depression in patients of different age groups. It is well tolerated by elderly patients, does not cause dependence or sedation, is characterized by low toxicity and a low risk of interaction with other drugs. Normally, in a healthy person, interoceptive sensations from working organs are subliminal and do not reach consciousness. In organic pathology, interoceptive sensations in places of the pathological process go far beyond the subthreshold level and are perceived as real pain. Also M.I. Astvatsaturov noticed that sensations from an organ with subclinical pathology are perceived to a slightly greater extent than from a healthy one. Lability of mood, weakness of concentration, decrease in higher integrative functions of the brain disrupt the adequate perception of sensations from one’s own body. Thus, both conditions for the formation of non-psychotic hypochondria are met, resulting in an incorrect interpretation of increased interoceptive sensations. Further, such a “pathological algic system” independently develops according to the laws of pathological dominance, greatly changing the clinical picture of any somatic disease that an elderly patient already has. With depression in older people, all perception thresholds change, including pain, and this creates an excellent basis for enhancing interoceptive sensations. Anxiety, usually observed in elderly patients, forces them to “listen” to their organs, and such an excessive anxious state can lead to cardio- and cancerophobia. Both serotonin and norepinephrine mediation are involved in many of the mechanisms of pathogenesis of this torpid clinical condition.
Venlafaxine, having a pathogenetic effect on the links of the pathological process, helps fight anxiety and hypochondriacal depression. Let us recall that depression in old age is characterized not so much by a strong decrease in mood as by an excessive clinical picture of existing somatic diseases, hypochondriacal fixation on them and pseudodementia. Unlike other antidepressants, Venlaxor helps improve memory and attention - indicators of the cognitive sphere that suffer from depression in older people. No dose adjustment is required when prescribing Venlaxor to elderly patients.
Thus, venlafaxine (Venlaxor) is one of the most promising representatives of the class of antidepressants, which has a dual mechanism of action (serotonergic and noradrenergic), which provides a more balanced effect on neurotransmission and synergism of psychopharmacological effects. Combining the high effectiveness of tricyclic antidepressants with the good tolerability and safety of selective antidepressants, Venlaxor can be successfully used in a wide range of depressive conditions of varying severity, in patients with anxiety and depressive disorders, in somatogenic and post-stroke depression, for the treatment of generalized anxiety, as well as in therapy depression resistant to selective serotonin reuptake inhibitors. The speed of onset of the initial clinical response determines the quality and durability of remission, and also reduces the total cost of treatment.
Venlaxor®
Concomitant use of monoamine oxidase inhibitors
(MAO) and venlafaxine are contraindicated. Taking Venlaxor® can be started no less than 14 days after the end of therapy with MAO inhibitors. If a reversible MAO inhibitor (moclobemide) was used, this interval may be shorter (24 hours). Therapy with MAO inhibitors can be started no less than 7 days after discontinuation of Venlaxor®.
Venlafaxine does not affect the pharmacokinetics of lithium
.
When used simultaneously with imipramine
the pharmacokinetics of venlafaxine and its metabolite EDV do not change.
Haloperidol:
the effect of the latter may be enhanced due to an increase in the level of the drug in the blood when used together.
When used simultaneously with diazepam
the pharmacokinetics of the drugs and their main metabolites do not change significantly. There was also no effect on the psychomotor and psychometric effects of diazepam.
When used simultaneously with clozapine
There may be an increase in its level in the blood plasma and the development of side effects (for example, epileptic seizures).
When used simultaneously with risperidone
(despite the increase in AUC of risperidone), the pharmacokinetics of the sum of the active components (risperidone and its active metabolite) did not change significantly.
Increases the effects of alcohol
on psychomotor reactions.
While taking venlafaxine, special caution should be exercised during electroconvulsive therapy.
, since there is no experience with the use of venlafaxine in these conditions.
Drugs metabolized by cytochrome P 45 isoenzymes
0:
The enzyme CYP2D6 of the cytochrome P 450 system converts venlafaxine into the active metabolite EDV. Unlike many other antidepressants, the dose of venlafaxine does not need to be reduced when administered simultaneously with drugs that inhibit CYP2D6 activity, or in patients with a genetically determined decrease in CYP2D6 activity, since the total concentration of the active substance and metabolite (venlafaxine and EDV) will not change. The main route of elimination of venlafaxine involves metabolism by CYP2D6 and CYP3A4; therefore, special caution should be exercised when prescribing venlafaxine in combination with drugs that inhibit both of these enzymes. Such drug interactions have not yet been studied.
Venlafaxine is a relatively weak inhibitor of CYP2D6 and does not suppress the activity of the CYP1A2, CYP2C9 and CYP3A4 isoenzymes; therefore, it should not be expected to interact with other drugs that are metabolized by these liver enzymes.
Cimetidine
suppresses the “first pass” metabolism of venlafaxine and does not affect the pharmacokinetics of EDV. In most patients, only a slight increase in the overall pharmacological activity of venlafaxine and EDV is expected (more pronounced in elderly patients and with impaired liver function).
Clinically significant interactions of venlafaxine with antihypertensive (including beta blockers, ACE inhibitors and diuretics) and hypoglycemic drugs
not detected.
Drugs bound to plasma proteins:
Plasma protein binding is 27% for venlafaxine and 30% for EDV. Therefore, it does not affect the concentration of drugs in the blood plasma that have a high degree of protein binding. When taken simultaneously with warfarin, the anticoagulant effect of the latter may be enhanced.
When taken simultaneously with indinavir
the pharmacokinetics of indinavir changes (with a 28% decrease in the area under the AUC curve and a 36% decrease in the maximum concentration of Cmax), and the pharmacokinetics of venlafaxine and EDV do not change. However, the clinical significance of this effect is unknown.
Venlaxor, 30 pcs., 37.5 mg, tablets
Discontinuation of Venlafaxine: As with other antidepressants, abrupt cessation of venlafaxine therapy - especially after high doses of the drug - may cause withdrawal symptoms, and therefore it is recommended to gradually reduce the dose before discontinuing the drug. The length of the period required to reduce the dose depends on the dose size, duration of therapy, as well as the individual sensitivity of the patient.
When prescribing Venlaxor® tablets to patients with lactose intolerance, the lactose content in the drug should be taken into account (30 mg in each tablet 37.5 mg; 60 mg in each tablet 75 mg).
In patients with depressive disorders, the possibility of suicide attempts should be considered before starting any drug therapy. Therefore, to reduce the risk of overdose, the initial dose of the drug should be as low as possible, and the patient should be under close medical supervision.
In patients with affective disorders when treated with antidepressants, incl. venlafaxine, hypomanic or manic states may occur. Like other antidepressants, venlafaxine should be used with caution in patients with a history of mania. Such patients require medical supervision.
Like other antidepressants, venlafaxine should be administered with caution to patients with a history of epileptic seizures. Treatment with venlafaxine should be interrupted if epileptic seizures occur.
Patients should be warned to immediately consult a doctor if a rash, urticaria or other manifestations of allergic reactions occur.
In some patients, while taking venlafaxine, a dose-dependent increase in blood pressure was noted, and therefore regular blood pressure monitoring is recommended, especially during the period of selecting or increasing the dosage.
An increase in heart rate may occur, especially during high doses. Caution is recommended for tachyarrhythmia.
Patients, especially the elderly, should be warned about the possibility of dizziness and impaired balance.
Like other serotonin reuptake inhibitors, venlafaxine may increase the risk of bleeding into the skin and mucous membranes. Caution is necessary when treating patients predisposed to such conditions.
While taking venlafaxine, especially in conditions of dehydration or decreased blood volume (including in elderly patients and patients taking diuretics), hyponatremia and/or syndrome of insufficient secretion of antidiuretic hormone may occur.
Mydriasis may occur while taking the drug, and therefore it is recommended to monitor intraocular pressure in patients prone to increased pressure or suffering from angle-closure glaucoma.
Venlafaxine has not been studied in patients with recent myocardial infarction and decompensated heart failure. The drug should be prescribed to such patients with caution.
It is necessary to monitor patients for signs of drug abuse, especially for patients with a history of such symptoms.
Women of childbearing potential should use appropriate contraception while taking venlafaxine.
Although venlafaxine does not affect psychomotor and cognitive functions, it should be taken into account that any drug therapy with psychoactive drugs may reduce the ability to make judgments, think or perform motor functions. The patient should be warned about this before starting treatment. If such effects occur, the degree and duration of restrictions should be determined by a physician. Drinking alcohol is also not recommended.