- Home /
- Branches /
- Vascular surgery and phlebology /
- Thromboangiitis obliterans
11/03/2021 The article was checked by vascular surgeon A.R. Rakhimov. , is for general informational purposes only and does not replace specialist advice.
For recommendations on diagnosis and treatment, consultation with a doctor is necessary. Buerger's disease , or thromboangiitis obliterans , is a systemic immunopathological inflammatory disease of small and medium-sized vessels of the extremities, in which obliteration of the arteries occurs and migratory thrombophlebitis occurs. The disease mainly affects young people under the age of 40.
Diseases of the arteries of the lower extremities
Arterial disease most often manifests itself as pain in the legs (so-called intermittent claudication).
The pain is of a certain nature: when a person begins to walk, after some time, when covering a certain distance, pain appears in the calves (on one or both sides), which may require rest. This is explained by the fact that when under load, the muscles require a large blood flow, and this is limited due to the pathological narrowing of the arteries. Edema is not typical for arterial insufficiency. As the disease progresses, the walking distance decreases, hair falls out on the legs (hypotrichosis), and the leg muscles atrophy due to constant oxygen starvation. In the later stages of the disease, pain is also bothersome at rest, more at night when the legs are in a horizontal position, which reduces blood flow. When the patient lowers his legs down from the bed, the pain decreases. When the first symptoms of arterial insufficiency appear, you should immediately consult a doctor - this will prevent the development of severe complications - gangrene, etc. The simplest, most accessible and informative method for studying the arteries of the lower extremities is ultrasound.
Below is a medical overview of the main surgical arterial diseases
Diagnostic measures
If you have symptoms of the disease, you should not expect that everything will go away on its own: if the listed signs appear, contact the vascular clinic to find out the causes of the ailment. Diagnosis includes examining the patient and taking a medical history. The doctor assesses the external condition of the limbs, listens to the pulse, and measures blood pressure. Additionally, blood tests and instrumental studies are prescribed, including angiography of the vessels of the extremities and Doppler ultrasound.
Etiology
The main etiological aspects of atherosclerosis in the arteries of the lower extremities do not differ significantly from the mechanisms of formation of atherosclerosis in any other localization. The main importance is given to lipid metabolism disorders. Against the background of increased cholesterol levels in the blood, cholesterol infiltrates the vascular wall. In this case, the predominance of low-density lipoproteins (LDL) is most important. An indicator reflecting the balance between the level of atherogenic and antiatherogenic lipids is called the atherogenic index (coefficient) and is an important indicator of predisposition to the development of atherosclerosis.
Another important etiological factor is damage to the vascular wall - smoking, hypertension, immunological disorders, etc.
The course of OASNK is significantly complicated by the presence of concomitant diabetes mellitus and atrial fibrillation.
Causes of the disease
Among the factors that provoke the disease:
• infectious nature of the problem;
• neurogenic factor – damage to nerve fibers;
• neuroendocrine causes - increased adrenal function increases the release of adrenaline, which causes vasospasm;
• trauma, intoxication and allergies;
• genetic influences;
• smoking. This reason has recently been attributed to the spread of the disease in women.
None of these hypotheses have yet been confirmed or refuted. In the last few years, scientists have been inclined to believe that the disease may be genetic or autoimmune in nature. The latter implies that the body, for no apparent reason, begins to secrete antibodies that attack cells of certain tissues.
Pathomorphology
The main changes develop in the intima of the arteries. There are 5 morphological stages of atherosclerosis:
- Prelipidic – characterized by increased endothelial permeability, destruction of the basement membrane, destruction of elastic and collagen fibers.
- Stage of lipoidosis - focal infiltration of the arterial intima with lipids occurs.
- Stage of liposclerosis - a fibrous plaque forms in the intima of the artery.
- Stage of atheromatosis - destruction of the plaque occurs with the formation of an ulcer.
- Stage of atherocalcinosis – plaque calcification occurs.
Based on the type of damage to the vascular bed, segmental and diffuse atherosclerosis are distinguished. In the first case, the process develops in a limited area of the vessel from single plaques to complete occlusion of the lumen. This type is more favorable in terms of the potential for performing bypass reconstructive operations on blood vessels. The diffuse type involves widespread atherosclerotic lesions predominantly in the distal bed, leaving no “window” for the surgeon to apply a shunt or prosthesis. The destiny of such patients is conservative therapy in order to delay the onset of gangrene as much as possible.
Clinical picture
The clinical picture of the disease depends on the stage of chronic arterial insufficiency of the lower extremities (CAI). The main subjective manifestation of the disease is pain in the calf muscles, initially associated with walking at various distances, and then at rest. In the later stages of the disease, pain occurs not only in the legs, but also in the feet and fingers. It should be borne in mind that when the bifurcation of the aorta and iliac arteries is damaged, pain can also occur in the muscles of the thighs and lower back, and impotence often develops (Leriche syndrome). Most clinical classifications of CHANC are based on pain syndrome.
We believe that the Fontan classification with some modifications is most suitable for clinical use.
Stage 1 – patients complain of pain in the calf muscles when walking about 1 km. The pain causes the patient to limp (intermittent claudication), but the lameness goes away with rest. These pains are associated with muscle ischemia caused by difficult access to arterial blood. At this stage, the symptoms are transient, the pulse in the lower extremities is preserved at all levels (may be weakened), the color of the lower extremities is not changed, there is no muscle atrophy, but hypotrichosis (reduced hair growth in the distal extremities) and changes in the nails in the form of brittleness may occur , susceptibility to fungal diseases.
Stage 2A – pain appears when walking a distance of 200 to 500 meters.
Stage 2B – intermittent claudication occurs when walking less than 200 meters. At this stage, one can observe hypotrichosis, changes in the nails, wasting of the muscles of the legs, pallor of the skin of the distal parts of the lower extremities. The pulse in the foot is usually absent; above it, it can be preserved, depending on the level of the lesion. It should be noted that many patients consult a doctor at this stage, because it significantly reduces the quality of life of patients.
Stage 3 is characterized by severe hemodynamic disturbances in the limb, its main symptom being pain when walking less than 50 meters and pain at rest. Pain at rest mainly bothers patients at night, because... horizontal position of the limb in bed reduces the flow of arterial blood to the distal areas. To increase blood flow, and therefore reduce pain, patients have to lower their legs from the bed up to several times a night. Based on this sign, some authors distinguish stages 3A and 3B of the disease.
Stage 3A – patients lower their legs out of bed up to 5 times per night.
3B – more than 5 times a night or sleep half-sitting with legs down.
At the third stage of the disease, all of the above disorders (hypotrichosis, atrophy, etc.) increase, and mental disorders caused by constant pain and lack of sleep are added. Patients become irritable, faith in the success of treatment decreases, many try to resort to “folk” remedies, which often worsens the course of the disease, causing the appearance of trophic disorders and sometimes gangrene. The pulse on the foot is not detected, on the popliteal artery - rarely, on the femoral artery, in the case of high occlusion, the pulse is not detected.
The photo shows skin necrosis in the area of the metatarsophalangeal joint against the background of obliterating atherosclerosis of the arteries of the lower extremities.
During treatment, the wound cleared and granulated (began to heal).
Complications of Berger's disease
The course of the disease may vary.
Some people experience no complications for years. Many are not even aware of their illness. Other patients may develop the following complications:
1. Hypertension
.
Damage to kidney cells leads to increased blood pressure, which in turn continues to damage the kidneys. A kind of “vicious circle” is formed.
2. Acute renal failure
.
As a result of Berger's disease, the kidneys catastrophically lose their ability to filter toxins. The patient is forced to undergo hemodialysis, otherwise kidney failure leads to death.
3. Chronic renal failure
.
The mechanism of development is the same as in acute failure, but the deterioration of kidney function occurs gradually. In both cases, the patient may need a kidney transplant.
4. Nephrotic syndrome
.
This is a group of symptoms caused by damage to the renal glomeruli - increased protein and red blood cells in the urine, high cholesterol, swelling.
Gangrene
The development of gangrene marks stage 4 of HUNC. Between the third stage and the appearance of gangrene, a phase of critical limb ischemia has recently been distinguished, which is characterized by intense pain at rest with the formation of superficial distal necrosis and trophic ulcers.
Gangrene manifests itself by the appearance of bluish lesions on the toes or heels, which subsequently become black. The lesions tend to spread, merge, and involve the proximal parts of the foot and lower leg.
Traditionally, dry and wet gangrene are distinguished. Their main difference is the delimitation (demarcation) of the area of necrosis from other tissues. With dry gangrene, there is an area of black skin, clearly demarcated from the surrounding unchanged tissue, with no tendency to spread. The general condition of the patients does not suffer (except for persistent pain), there are no signs of intoxication, and there is no hyperthermia. This type of gangrene with a small affected area (for example, dry gangrene of the distal phalanx of the toe) can be managed conservatively for a long time, without giving indications for surgery; in some cases, self-rejection of the necrotic area is possible. Haste with surgery in such a situation, due to surgical trauma, can cause progression of the necrotic process.
With wet gangrene, there is no demarcation, there are areas of both black and bluish color on the foot, the skin proximal to the focus of necrosis is hyperemic, and from under the necrosis there is a purulent discharge with an unpleasant odor. There are signs of intoxication (thirst, tachycardia, etc.), hyperthermia to subfebrile and febrile levels. The wet process is characterized by rapid progression, with necrosis spreading in the proximal direction.
In stage 4, some authors distinguish between stage 4A - when there is a prospect of preserving the supporting function of the limb (for example, if it is possible to perform amputation according to Sharp or Chopart while maintaining the supporting function of the heel) and 4B - when the patient is shown a high amputation at the level of the thigh or lower leg.
The presence of concomitant atrial fibrillation in a patient can cause a rapid transition from one stage of arterial insufficiency to another. With atrial fibrillation, in many patients, thrombotic masses accumulate in the left ventricle of the heart, the separation of which and migration in a large circle to the lower extremities can aggravate the existing arterial stenosis with transition to a more severe stage of ischemia, up to the development of gangrene.
Some tests can help in diagnosing limb ischemia, for example, the finger pressing symptom, Oppel's plantar ischemia symptom, Goldflam's test, Panchenko's knee phenomenon, etc.
Disorders with similar symptoms
Symptoms of the following disorders may be similar to those of Buerger's disease. Comparisons can be useful for differential diagnosis:
- Vasculitis is inflammation of blood vessels. In people with vasculitis, inflammation damages the lining of affected blood vessels, causing narrowing, blood clots (thrombosis), and/or blockage. As a result, the blood supply of oxygen to certain tissues may be limited (ischemia), which can lead to pain, tissue damage, and in some cases, failure of some affected organs. Vasculitis affects veins and arteries of any type or size; may affect one or more organs and tissues of the body; and be a primary (independent) disease or arise from or in connection with a number of different underlying disorders. Consequently, the range and severity of symptoms and signs associated with vasculitis varies greatly. The specific cause of vasculitis is not fully understood. However, it is believed that in most cases the disease is associated with disorders of the body's immune system.
- Scleroderma is a rare connective tissue disease characterized by abnormal thickening of the skin. Connective tissue is made up of collagen, which supports and connects other tissues in the body. There are several types of scleroderma. Some types affect specific parts of the body, while other types affect the entire body and internal organs (systemic). The exact cause of scleroderma is unknown. The immune system and vascular system, as well as connective tissue metabolism, are known to play a role in the disease process.
- Takayasu arteritis is a rare disease characterized by inflammation of the large elastic arteries. The main artery of the heart and the pulmonary artery are affected. The disorder causes progressive inflammation of many arteries in the body (polyarteritis), resulting in decreased blood flow. Arteries in the head and arms may be affected, which can lead to loss of the body's major pulse points. Some people with this arteritis have irregular narrowing of parts of the large arteries (segmental stenosis) and abnormal backflow of blood from the aorta into the left ventricle of the heart (aortic regurgitation).
Data from laboratory and instrumental examination methods
Laboratory examination allows us to identify patients at risk of developing atherosclerosis (increased blood cholesterol, atherogenicity index), identify patients with diabetes mellitus (increased blood glucose levels), which significantly complicates the course of the disease, and assess the state of the blood coagulation system (coagulogram). Culture from a trophic ulcer allows you to identify the causative agent of infection and prescribe rational antibiotic therapy.
Instrumental methods.
The most accessible and informative method, successfully used in outpatient settings, is currently recognized as duplex ultrasound scanning of the arteries of the lower extremities (USAS) - an ultrasound method that allows you to assess the condition of the vascular wall, identify atherosclerotic plaques, determine the level and extent of arterial occlusion, and assess the type blood flow, measure important indicators (brachial-ankle index, etc.). The study should be carried out in all patients suspected of having any stage of CANDC.
Currently, surgeons in Moscow practically do not use rheovasography (RVG) in the diagnosis of OASNK, because it allows you to determine only the deterioration of the arterial blood supply to the lower extremities, which is easily diagnosed based on clinical signs and USAS data.
Angiography is a radiopaque research method used in a hospital setting to clarify the localization of the process and select the method of surgical intervention. The method is highly informative, but since it is not used in outpatient practice, we will not dwell on it in detail.
Microcirculation disorders are determined using capillaroscopy, transcutaneous determination of oxygen tension in superficial tissues and laser Dopplerography - they are of more scientific than practical interest.
Risk factors
The risk of Berger's disease increases with the following factors:
1. Age. The disease affects people of any age, but most often young people aged 15-25 years.
2. Gender In Western Europe and North America, Berger's disease affects men twice as often as women.
3. Nationality. IgA-type nephropathy is most common among peoples of the Caucasus and Asians, less common among people from Africa.
4. Family history. Often Berger's disease can be traced in a certain family for several generations.
Treatment
OASNK is a chronic, continuously progressive disease that requires constant treatment and monitoring of the patient. Treatment tactics depend on the stage of the disease, immediate clinical manifestations, and concomitant pathology.
All patients diagnosed with OASNK must immediately and permanently quit smoking. It is extremely important to control blood cholesterol levels and correct them, which can be carried out together with a cardiologist. All patients need an ECG and consultation with a therapist (cardiologist) to identify risk factors for atherosclerosis such as atrial fibrillation and hypertension. If diabetes mellitus is detected, the patient should be observed by an endocrinologist.
At stages 1 and 2A of the disease, the patient is prescribed a course of treatment with vascular drugs (antiplatelet agents, angioprotectors, agents that improve microcirculation, etc.) - trental, aspirin, nicotinic acid, reopolyglucin, actovegin, etc.
The following treatment regimen can be recommended:
Trental 400 mg x 3 times a day – 1 month
ThromboASS 50 mg/day 2 months
Nicotinic acid 1.0 x 3 r per day IM (can be 1 t x 3 r) – 3 weeks
If intravenous drips are possible (for example, in the presence of a day hospital) -
Reopoliglucin 400.0 IV drip, every other day No. 5.
Actovegin 10.0 in saline solution 400.0 IV drip, every other day No. 5.
Up to three such courses are required per year. The effect is assessed by increasing the walking distance and improving blood flow indicators according to USAS. If, despite the therapy, no positive effect is observed, it makes sense to hospitalize the patient as planned for inpatient examination and treatment.
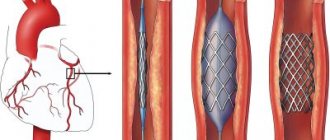
Stages 1 and 2A CHANC are always subject to conservative treatment. In the presence of stage 2B, as well as in stage 3 CHANC, the patient should be referred for a consultation with an angiosurgeon to decide on the advisability of surgical treatment. Currently, shunt and prosthetic operations are used, as well as lumbar sympathectomy (the effectiveness of the latter method has recently been disputed by many authors). Stenting is gaining increasing acceptance.
In case of stage 3 CHANC, it is advisable to hospitalize the patient as planned for treatment in a hospital setting. If the patient refuses hospitalization, it is advisable to carry out the following course of treatment:
Trental 400 mg x 3r – 1 month
Xanthinol nicotinate 1.0 x 2p – 3 weeks
ThromboASS 50 mg/day continuously
Aevit 1 tablet x 3p 10 days
Neuromultivitis 1t x 3p – 2 weeks
Reopoliglucin 400.0 IV drop daily No. 10
Alprostan 100 mcg per 250 ml of saline solution IV drop, slowly 1 r per day, No. 14. or Vazaprostan 20 mcg per 250 ml saline solution IV drop for at least 2 hours 1 r per day No. 14.
Alprostan and vazaprostan should be administered with caution, under the control of blood pressure, due to the possibility of its decrease in elderly and debilitated patients.
In the complex therapy of OASNK, such drugs as Vesel Due F, Tanakan are also successfully used.
For pain syndrome, it is necessary to prescribe analgesics per os and parenterally (depending on the severity of pain). Both non-narcotic analgesics (ketorol, pentalgin, etc.) and centrally acting drugs (tramal) or combined ones (zaldiar) are used.
In patients with concomitant diabetes mellitus, it is advisable to include in the treatment regimen thioctic acid preparations that improve carbohydrate and lipid metabolism (for example, Espa-lipon or Berlition 600 mg per 250 ml of saline solution intravenously for 2 weeks, then in tablets for 200 mg x 3-4 times a day for 3 months).
At stages 2B – 3 of CANDC, it is advisable for patients to avoid physical activity, especially those related to walking, hypothermia or, conversely, overheating of the lower extremities. It is especially dangerous to steam your feet in hot water, because... disruption of arterial blood flow to the limb due to overheating causes the appearance of trophic disorders, including the development of gangrene.
Critical ischemia, the development of dry or wet gangrene are indications for emergency hospitalization of the patient
Particularly difficult is the treatment of trophic disorders in the form of ulcers against the background of stage 3 A-B CHANK or critical ischemia of the lower limb. In such patients, pain is constantly present, the ulcers are poorly cleaned, and often with the most adequate and persistent treatment, there is a progression of the necrotic process, ultimately leading to amputation. All patients with trophic disorders should be consulted by an angiosurgeon to decide on the possibility of performing reconstructive vascular surgery or stenting. If such an operation can be performed, it significantly improves hemodynamics in the limb, which significantly accelerates the healing of ulcerative defects. Contraindications to reconstructive operations are usually: damage to the distal vascular bed, which excludes the possibility of applying a shunt, severe concomitant pathology, which gives a high surgical and anesthetic risk of intervention. In such a situation, if appropriate conditions exist (short extent of stenosis, etc.), stenting can be performed as a minimally invasive and fairly safe method.
Lifestyle and diet
Patients can take the following steps to help their body:
1. Switch to a low-salt diet. This will help keep your blood pressure under control, and the pressure, in turn, will not damage the kidney cells. This diet will help minimize fluid retention and eliminate swelling.
2. Eat less protein. A diet low in protein and cholesterol helps slow the progression of Berger's disease and protects the kidneys.
3. Monitor your blood pressure at home. You need to measure your blood pressure daily, record the results in a diary and show them to your doctor so that he can evaluate the effectiveness of the treatment.
Conservative therapy of trophic disorders comes down to two areas
1. Conducting drug therapy aimed at improving microcirculation in the affected limb and relieving pain according to the above schemes. At the beginning of treatment of purulent-necrotic ulcers, it is necessary to carry out antibacterial therapy; a culture should be taken from the wound to determine the sensitivity of the microflora to antibiotics. Pending culture results, a broad-spectrum antibiotic such as a fluoroquinolone or cephalosporin may be prescribed. Further antibacterial therapy is carried out based on the culture results. The parenteral route of administration of the antibiotic is preferable, but if injections are not possible, tablet forms can be prescribed.
2. Local treatment - dressings. When treating a necrotic ulcerative defect, you must first ensure that it is cleansed of necrotic masses. To do this, daily dressings are carried out with enzymes (Chymotrypsin, Himopsin, Daltsex-trypsin wipes, etc.) or water-soluble ointments (Levomekol, Levosin). In case of severe pain in the area of the ulcer, it is preferable to use Levosin, which contains a local anesthetic.
After cleansing the ulcer, you can use ointment-based products for dressings - Solcoseryl, Actovegin, Panthenol-ratiopharm, etc.
For the treatment of almost clean, flaccid granulating ulcers, the drug “Curiosin” in drops has proven itself well - 1-2 drops per 1 cm2 of the wound surface.
If the wound has cleared, but is poorly granulated and epithelialized, Solcoseryl 2 ml intramuscularly, daily, No. 14 can be added to therapy.
Dressings are carried out as follows: a surgeon wearing sterile gloves treats the wound surface with a ball on tweezers moistened with a 3% solution of hydrogen peroxide, achieving maximum leaching of tissue detritus and remnants of medicinal substances from the wound. Then the wound is dried with a dry gauze ball, a medicinal substance is applied, and the wound is closed with sterile gauze pads, which are fixed with a gauze bandage. The bandage should not be applied tightly so as not to impair blood circulation in the limb.
In the initial stages (CHANK stage 1-2) of the disease, patients are prescribed sanatorium treatment - hydrogen sulfide baths, as well as physiotherapy.
More about atherosclerosis of the arteries of the lower extremities
Russian National Atherosclerosis Society
Obliterating atherosclerosis of the lower extremities
The concept of obliterating atherosclerosis of the extremities
Obliterating atherosclerosis (that is, that atherosclerosis that leads to “overgrowth” of the lumen of the vessel) is classified as occlusive lesions of the arteries.
Occlusion (from the Latin word occlusus - “locked” [2]), in turn, is the blockage of any vessel due to various reasons, including as a result of atherosclerotic lesions. Obviously, blockage of an artery, for example, the femoral one, leads to a cessation of blood flow through it and disruption of the blood supply to the leg. Thus, obliterating atherosclerosis is a special case of occlusive disease of the arteries, in which the progressive growth of an atherosclerotic plaque inside the vessel leads to blockage of the arteries. Obliterating atherosclerosis can develop in any of the arteries of the extremities, but more often it occurs in the arteries of the legs. Therefore, in this section we will talk about atherosclerotic lesions of the arteries of the legs or lower extremities. Diabetes mellitus is quite often combined with obliterating atherosclerosis of the arteries. Unlike obliterating atherosclerosis, which occurs with damage to arteries of large and medium diameter, with diabetes mellitus occlusion of small arteries, mainly of the foot, develops. The result is a condition called diabetic foot.
Obliterating atherosclerosis of the legs is most common in older people, but this disease can also be observed at an earlier age (up to 50 years). Men, especially smokers, become ill approximately 10 times more often than women [3, 9]. Often there is so-called multifocal atherosclerosis, in which atherosclerotic arterial lesions develop simultaneously in the arteries of several organs or parts of the body. Obliterating atherosclerosis of the legs can be combined, for example, with atherosclerosis of the coronary arteries of the heart, when damaged, coronary heart disease (CHD) develops. In such cases, the manifestations of combinations of these diseases may be different. As a rule, damage to the arteries of the legs during physical activity will make itself felt earlier than manifestations of coronary artery disease (angina pectoris, etc.) occur.
Concept of blood supply to the lower extremities
Impaired blood supply to the legs can develop with atherosclerotic lesions of various arteries, starting from the final (terminal) section of the abdominal aorta and ending with small vessels of the leg and foot. The terminal portion of the abdominal aorta gives rise to two common iliac arteries. This location of the abdominal aorta is called the bifurcation. The common iliac arteries are in turn divided into internal and external iliac arteries. The internal iliac artery supplies blood mainly to the organs of the pelvic region (bladder, rectum, external and internal genital organs) and partially to the gluteal muscles. The external iliac artery in its initial section supplies blood mainly to the soft tissues (muscles, skin, etc.) of the anterior abdominal wall. The direct continuation of the external iliac artery, starting from the groin region, is the femoral artery, which supplies blood to the leg.
The femoral artery directs its course to the popliteal fossa, simultaneously giving off the so-called deep and superficial branches (arteries). In the knee area, the femoral artery is called the popliteal artery, which subsequently divides into the anterior and posterior tibial arteries, which supply blood to the lower leg and foot. The most important branch of the posterior tibial artery is the peroneal artery, which supplies blood to the calf muscles. The arteries of the leg are connected to each other through their branches (anastomoses), mostly in the area of the lower leg and foot. It is for this reason that if only one of the arteries of the same leg is affected by atherosclerosis, pronounced disturbances in the blood supply to the leg and foot cannot develop. This is due to the fact that the blood supply to the leg in this situation will be provided by collateral (roundabout) arteries. Significant disturbances in the blood supply to the leg and foot will occur either when all arteries of the leg are affected, or when the arteries above are blocked (popliteal, femoral, external iliac, etc.).
Development of obliterating atherosclerosis of the legs
As mentioned above, obliterating atherosclerosis is a special case of occlusive damage to the arteries. There are acute occlusion, which occurs suddenly, and chronic occlusion, which develops gradually. A transition from chronic to acute occlusion is possible, for example, when an atherosclerotic plaque ruptures with subsequent formation of blood clots on its uneven surface (arterial thrombosis). But still, in the vast majority of cases, obliterating atherosclerosis of the arteries of the legs develops gradually. Until, as a result of the growth of an atherosclerotic plaque, the lumen of a particular artery narrows by more than half, manifestations of the disease do not occur.
A decrease in the diameter of the artery lumen causes chronic ischemia (oxygen starvation or hypoxia) of the leg tissues, especially its muscles. Initially, leg ischemia occurs only when performing physical activity and manifests itself as so-called intermittent claudication. This sign (symptom) of the disease consists of the appearance of various kinds of pain, cramps, and sometimes just fatigue in the legs. The main thing is that all these sensations develop when performing physical activity, initially when walking quickly “uphill” or when climbing stairs. The appearance of pain or discomfort in the legs forces the patient to stop. During rest, blood flow in the leg muscles is restored and the amount of chemicals that accumulate in them due to oxygen starvation is reduced. It is these chemicals, particularly lactic acid, that are believed to cause pain in the leg muscles.
The most interesting thing is that for the ischemia of the leg muscles to disappear, it is enough to stop for only a few minutes. There is no need to sit down or lie down. As soon as the discomfort in the leg muscles passes, the same brisk walking can be continued until the attack of leg muscle ischemia resumes. Over time, intermittent claudication occurs during normal walking. The progression of the disease leads to the fact that the distance that can be covered without the appearance of intermittent claudication is steadily decreasing, day by day. Pain with intermittent claudication can occur in various muscles of the legs, which depends on the level of location of atherosclerotic lesions of the abdominal aorta and arteries of the legs. If atherosclerosis develops in the terminal part of the abdominal aorta with a transition to the common iliac arteries, then pain occurs in the muscles of the buttocks, thighs and legs. When atherosclerosis affects the femoral and popliteal arteries, pain occurs in the calf muscles of the leg where atherosclerosis is present. It is believed that with isolated obliterating atherosclerosis of the arteries of the leg, intermittent claudication does not occur. With further growth of the atherosclerotic plaque, the lumen of the artery can decrease significantly. This leads to the fact that pain in the legs can be observed at rest, and the pain becomes prolonged. Increased pain is observed as a result of giving the leg an elevated position.
Significant pain in the legs occurs when, in addition to the main artery, blood flow through the collateral arteries is also disrupted. In addition to pain, in such cases, persistent numbness of the toes may occur along with a sensation of “crawling goosebumps” (paresthesia). In advanced cases, with obliterating atherosclerosis of the legs, tissue necrosis (gangrene) of the foot develops, as well as poorly healing skin ulcers, primarily on the legs and feet. With atherosclerotic lesions of the terminal (end) section of the abdominal aorta, involving the common iliac arteries, men may experience impotence. To be more precise, we are talking about impaired erection of the penis. The combination of intermittent claudication, erectile dysfunction, decreased muscle mass in the legs, as well as constant pallor of the legs and feet with atherosclerosis of this location is called Leriche syndrome (i.e., a set of symptoms).
If a patient with atherosclerosis of the legs has diabetes mellitus, disturbances in the local nervous regulation of tissues, mainly the legs and feet, may be observed. This leads to the loss of so-called pain sensitivity, i.e. when the skin is irritated by any sharp object, for example, a needle, no pain occurs. Skin ulcers in such patients are also painless and difficult to cure. When an atherosclerotic plaque ulcerates on its uneven surface, as mentioned above, blood clots can form, which can contribute to the development of acute arterial occlusion as a result of arterial thrombosis (see above). Manifestations of this life-threatening condition occur below the location of the thrombosis, for example, with thrombosis of the external iliac artery, the blood supply to the thigh, leg and foot is disrupted.
Complaints of patients with obliterating atherosclerosis of the legs
The main complaint of patients with obliterating atherosclerosis of the leg arteries is muscle pain. It can be sharp or dull, sometimes bursting pain, often accompanied by muscle cramps. At first, the pain occurs with intense activity, such as running, fast walking, or climbing stairs. The appearance of pain forces the patient to stop. On average, after 1-5 minutes the pain goes away, and it may be replaced by a feeling of fatigue in the legs. With further exercise, the pain appears again. After a certain period of time, depending on the speed of progression of the atherosclerotic process, there is a reduction in the duration of the distance that the patient can walk without pain. Pain in the legs occurs every time you start walking. At this stage of the disease, there may be no other complaints at rest, with the exception of erectile dysfunction due to atherosclerotic lesions of the terminal abdominal aorta.
With the increase of chronic occlusion of the arteries of the legs, patients note the appearance of pain at rest. These pains are usually intense and aching. To reduce pain, patients often dangle their legs off the bed while sleeping, which promotes additional blood flow to the leg muscles. Subsequently, due to impaired blood supply to the legs, cracks in the skin of the sole of the feet appear. Even the most minor injury to the legs can contribute to the appearance of long-lasting wounds and ulcers on the legs, which are painless in diabetes mellitus. These skin manifestations cause a lot of concern to patients. Leg skin ulcers in this case are trophic, i.e. associated with malnutrition of the lower extremities. Due to poor blood supply, the legs “lose” their muscle mass, as if they dry out. Numbness in the legs and a “crawling” sensation are often noted.
Diagnosis of obliterating atherosclerosis of the legs
A doctor can often suspect the presence of this disease in a patient as a result of a routine interview. When establishing a diagnosis of obliterating atherosclerosis of the lower extremities, it is mandatory to study the pulsation of the arteries of the legs. Usually the pulsation of the femoral artery (in the groin area), the popliteal artery (in the popliteal fossa) and the arteries of the lower leg (at the ankle) are determined. The pulse weakens or disappears below the level of arterial occlusion. In some cases, especially with narrowing (stenosis) of the terminal abdominal aorta, a noise can be detected above it using a phonendoscope. If the patient only has intermittent claudication, the appearance of the legs may not change. In advanced cases of the disease, the leg may look shrunken and its skin reddened. Hair growth on the legs may also stop and the growth of nails on the toes may be impaired. Non-healing wounds and skin ulcers are often found. The main methods for diagnosing obliterating atherosclerosis of the legs are ultrasound examination of the arteries in combination with an assessment of the speed of blood flow through them (Dopplerography). The combination of these techniques is called duplex scanning.
The use of modern equipment makes it possible to accurately determine the severity of narrowing of the abdominal aorta and leg arteries, including when they are completely occluded. These methods are usually complemented by a comparative assessment of the “upper” (systolic) blood pressure (BP) in the brachial artery and in various arteries of the legs using a conventional blood pressure measuring device. Normally, systolic blood pressure is higher in the legs than in the arms. With obliterating atherosclerosis of the legs, systolic blood pressure at the level of the ankles decreases in proportion to the severity of atherosclerosis of the arteries of the legs. If you supplement the measurement of blood pressure in the legs with methods of reproducing everyday exercise in an office environment, for example, using a “treadmill” (treadmill), then when muscle pain occurs, blood pressure in the legs will decrease.
There are many other bloodless (non-invasive) methods for assessing blood flow disturbances in the arteries of the legs (rheovasography, etc.), but all of them are complementary to Dopplerography. Angiography of the aorta and other arteries is the reference method for diagnosing occlusive lesions. The method consists of introducing a special catheter tube into the vascular bed under local anesthesia by puncturing a large artery of the arm or leg. This catheter is then brought to the site of occlusion and a contrast agent is injected through it. At the same time, X-ray photography is carried out. Angiographic examination is usually performed to decide on surgical treatment of the disease. Currently, there are various angiographic techniques in combination with computer technologies, but traditional angiography still remains the “gold” diagnostic standard.
Treatment of obliterating atherosclerosis of the legs
All patients with intermittent claudication are advised to walk regularly for at least one hour a day. This is necessary for the development of blood supply to the leg muscles through collaterals, as well as for increasing the duration of the pain-free period of walking. The essence of the technique is that the patient must walk until pain appears, then pause until it stops completely, and then continue walking again. Among the medications that are used in the treatment of this disease, vasodilators can be noted. The most effective vasodilators used in the treatment of obliterating atherosclerosis are the so-called prostaglandin E1 drugs, for example, alprostadil.
The use of alprostadil leads to dilation of the arteries and improved blood supply to the leg muscles. Alprostadil also reduces thrombus formation. Since this drug dilates the arteries not only of the legs, but also, in particular, of the heart, there is an increase in heart rate, which may be undesirable with concomitant coronary artery disease. There are also other vasodilators (so-called calcium ion antagonists, thromboxane inhibitors or buflomedil), but their effectiveness is currently being clarified. In the treatment of obliterating atherosclerosis, medications are used that reduce blood viscosity and improve the flexibility of red blood cells (erythrocytes), in particular pentoxifylline. This drug is prescribed in large doses, up to 1200 mg per day. Treatment of concomitant diabetes mellitus is necessary, since such a condition as diabetic foot has a poor prognosis due to the lack of effective treatment.
With the development of trophic ulcers and wounds of the skin of the legs, the use of special ointments and creams, including those containing antibiotics, may be required. Surgical treatment of patients with obliterating atherosclerosis of the lower extremities is carried out mainly in cases of severe disturbances in the blood supply to the legs, when complaints appear at rest. Surgical treatment includes the so-called balloon angioplasty, endarterectomy, bypass grafts, removal (resection) of the damaged section of the artery with its subsequent replacement, and the so-called sympathectomy [9].
The choice of surgical treatment method is determined by the location and extent of vascular changes, as well as the general condition of the patient and the presence of other (concomitant) diseases. As mentioned above, many patients with obliterating atherosclerosis of the legs also have severe atherosclerosis of the coronary arteries of the heart (CHD). During vascular bypass surgery or resection of a section of leg arteries in such patients, acute myocardial infarction or other heart complications may develop. Therefore, such patients often undergo heart surgery first. For narrowings of limited extent or complete occlusions of the arteries, balloon angioplasty is effective. The essence of this method is that, under local anesthesia, a large artery of the leg (arm) is punctured (pierced) and a special catheter tube is brought to the place of narrowing (occlusion) of the vessel. At the end of such a catheter there is a special balloon in a collapsed state, which is filled with liquid and inflated under high pressure.
As a result of this manipulation, the atherosclerotic plaque is destroyed and the patency of the artery is restored. Using this method, you can eliminate various narrowings in the arteries of the body, including the coronary arteries of the heart. Sometimes the method is supplemented by installing a special metal spacer spring (stent) in the place of the former narrowing. Balloon angioplasty can be performed without prior surgical treatment of coronary artery disease. In case of multiple narrowing of the artery, especially in combination with its calcification (calcification) or in the case of extended narrowing, vascular bypass surgery is performed, which consists in bypassing the narrowing using a vascular bridge-shunt. It is also possible to remove a section of the artery and then replace it with a vascular synthetic prosthesis.
When narrowing of the aorta and large arteries is limited in extent, they resort to endarterectomy - removal of their inner layer along with the atherosclerotic plaque. Sympathectomy is a surgical interruption of the vasoconstrictor effect of the nervous system. This method is performed when it is impossible to use other types of surgical treatment. Unfortunately, if small arteries of the leg and foot are damaged, especially with diabetes mellitus, restoration of arterial patency is impossible. In particular, it is technically impossible to apply a vascular bypass, since the arteries of the leg and foot can be closed (occluded) along their entire length. If such patients develop gangrene of the foot, then it is necessary to resort to amputation. As a rule, the level of amputation is sufficient to enable the possibility of prosthetic replacement of part of the leg in the future.
Prevention of obliterating atherosclerosis of the legs
General preventive measures boil down to eliminating risk factors for the development of atherosclerosis (impaired metabolism of cholesterol and its derivatives, obesity, detection and treatment of diabetes mellitus, smoking cessation, etc.). It has been noted that complete cessation of smoking, along with drug treatment, contributes to a significant improvement in the condition of patients and slows down the progression of the disease. Preventive foot care is extremely important for patients with foot ischemia. It is necessary to use moisturizing creams, avoid the use of irritating chemicals (callus fluids, etc.), beware of injuries, in particular when cutting toenails, for which it is recommended to seek the services of a pedicurist. Do not use electric heating pads or hot water containers to warm your feet. Carrying heavy objects should be avoided as this impairs the blood supply to the legs. To reduce the risk of various foot injuries, it is not recommended to walk barefoot; you should wear comfortable or orthopedic shoes.
Thromboangiitis obliterans (Buerger's disease)
Thromboangiitis obliterans (Buerger's disease) is a disease of an unknown nature, in which inflammatory changes in arteries of medium and small diameter, as well as in veins, lead to obliteration (overgrowth) of their lumen with disruption of blood movement through them. The disease occurs predominantly in young (20-40 years old) smoking men, and only in 5-20% of cases it is observed in women [6, 9]. It is believed that the basis of the disease is an altered reaction of the body to tobacco, which either causes or provokes inflammatory changes in blood vessels. The development of this disease cannot exclude a hereditary predisposition, as well as an altered response from the immune system. With thromboangiitis obliterans, the terminal sections of the arteries and veins of the legs and forearms, as well as the arteries and veins of the feet and hands, are affected. All layers of the walls of arteries and veins are involved in the inflammatory process, starting with the smallest ones, then inflammation of the arteries of medium diameter joins.
With thromboangiitis obliterans, there is a proliferation of cells in the inner layer of arteries and veins, causing a narrowing of their lumen. Subsequently, blood clots form in the lumen of the vessels, i.e. vascular thrombosis develops. As a result of these changes, the movement of blood through the vessels is disrupted, up to complete cessation. In advanced cases of the disease, hardening of the tissue around the arteries may develop, affecting nearby nerves. Rare cases of thromboangiitis obliterans of the arteries of internal organs have been described [6]. The disease begins with inflammation of the subcutaneous veins (phlebitis), most often of the legs and feet, which is manifested by the formation of sensitive nodules along the veins with redness of the skin over them. These nodules may subsequently disappear in one part of the vein and appear in another. The appearance of obvious signs of arterial damage is preceded by various temperature sensations from the vessels, mainly the hands and feet: patients note either a feeling of cold or heat in the hands and feet. And a number of patients have an abnormal reaction to cold: the fingers and toes, when exposed to cold, first turn white, then turn blue, and finally turn red (Raynaud's phenomenon).
Since the disease develops gradually, disturbances in the blood supply to the same hands and feet do not become noticeable immediately. With a significant narrowing of the lumen of the arteries, pain appears that occurs when walking and goes away with rest. The epicenter of pain is the arch of the feet and the lower part of the legs. Pain may also be felt in the hands when moving your fingers. As the disease progresses, muscle pain appears even at rest. When the lumen of the arteries is completely overgrown, the greatest disturbances in blood supply are observed in the fingers and toes. Trophic ulcers often form at their tips, and in advanced cases of the disease, irreversible necrosis (gangrene) of tissue, mainly the fingers and toes, can develop. The initial diagnosis of the disease is based on the study of patient complaints, as well as on the study of pulsation of the arteries of the arms and legs.
With thromboangiitis obliterans, pulsation in the large arteries of the extremities persists, but pulsation in the arteries of the hands and feet, as well as in the adjacent areas of the forearms and legs, disappears. Accurate information about the patency of blood vessels can be obtained by duplex scanning (a combination of ultrasound diagnostics with an assessment of the speed parameters of blood flow - Dopplerography). Determining blood pressure (BP) at various limb levels may also be useful. At the site of the vascular lesion, a sharp decrease in blood pressure is observed. To confirm the diagnosis, angiography can be used - injection of a contrast agent directly into the arteries, followed by x-rays. Treatment of the disease involves complete cessation of smoking; you should not even chew tobacco. Smoking contributes to the accelerated development of the disease. When you quit smoking, the disease does not reverse, but it may not progress further. To improve blood supply to the legs, daily walking is recommended, up to 30 minutes twice a day, which promotes the development of roundabout (collateral) blood circulation in the leg muscles. Careful care of the skin of the hands and feet is necessary, since any wounds and abrasions may not heal for a long time and may even fester.
For the same reasons, it is recommended to wear comfortable shoes. With the help of medication, temporary improvement can be achieved. Vasodilators, particularly alprostadil, may be helpful. There is currently no effective surgical treatment for thromboangiitis obliterans. As an auxiliary measure, surgical interruption of the vasoconstrictor effects of the so-called sympathetic nervous system (sympathectomy) can be performed.
Temporal arteritis
Temporal (cranial, giant cell) arteritis is a disease of unknown origin, in which, as a result of inflammatory changes in the wall of the arteries, the movement of blood through them is disrupted. The disease occurs in people over 50 years of age, somewhat more often in women. The inflammatory process primarily involves arteries of medium diameter, most often the head and neck. Often there is damage to the aorta and its branches. As a result of inflammation, a pronounced thickening of the inner layer of the arteries occurs, followed by a narrowing of their lumen. Patients are usually bothered by a throbbing headache, often in the temples and back of the head. Quite often there is pain or discomfort in the masticatory muscles when chewing, and sometimes during a long conversation. At the onset of the disease, general fatigue, weakness and increased body temperature may also be a concern. When the arteries of the eyes are involved in the inflammatory process, various visual impairments develop, including complete blindness.
If the disease is accompanied by so-called polymyalgia rheumatica, soreness in various muscles may be noted along with severe weakness. The arteries in this disease, in particular the temporal ones, are somewhat dilated, painful and knotty to the touch (rather than smooth). It should be noted that the arteries can be changed from the inside in the complete absence of corresponding external manifestations. A clinical (general) blood test usually reveals a decrease in hemoglobin levels and the number of red blood cells, an increase in the number of leukocytes and platelets. The erythrocyte sedimentation rate (ESR) in this disease is significantly increased. Ultrasound diagnostics in combination with assessment of blood flow velocity parameters (Doppler sonography) can be useful in identifying temporal arteritis. The main method for diagnosing this disease is a biopsy (obtaining pieces) of the temporal artery and then examining them under a microscope. To ensure diagnostic reliability, pieces of both temporal arteries are usually taken for biopsy. Treatment of the disease is medication. It is aimed primarily at preventing the development of complete blindness. Patients are prescribed so-called glucocorticosteroids, in particular prednisolone, for a long period (months, years). If there is no effect from glucocorticosteroids, the antitumor drug methotrexate is sometimes prescribed [6].
Raynaud's disease and syndrome
Raynaud's phenomenon refers to attacks of involuntary contraction (spasm) of small arteries (arterioles), accompanied by sudden pallor or blue discoloration (cyanosis) of the skin supplied by these arterioles to parts of the body. Raynaud's phenomenon can be either an independent manifestation (Raynaud's disease) or a consequence of other diseases and conditions (Raynaud's syndrome). The most common phenomenon is Raynaud's phenomenon of the fingers, less often - the toes, and sometimes the nose, tongue, etc. The origin of this phenomenon is not entirely clear; it is possible that it is associated with abnormalities of the arterioles themselves. It is also assumed that the so-called sympathetic nervous system is involved in the development of Raynaud's phenomenon, when irritated, a spasm of arterioles develops. Raynaud's disease predominantly affects young women. The disease usually occurs suddenly. Attacks are triggered by exposure to cold or emotional experiences.
The essence of the attacks is the development of a sudden spasm of arterioles and an associated decrease in blood flow, for example, to the fingers. A lack of blood supply is manifested by a sharp pallor of the skin, up to absolute whiteness. In this case, the same fingers temporarily stop feeling anything, but as a rule there is no pain in them. The attack lasts from several minutes to several hours and ends as suddenly as it began. At the end of the attack, the skin acquires a blue tint, and then, as a result of a rush of blood, the blue color changes to red. In some patients, pallor of the skin may be absent, but blueness and redness occur. It has been noted that exposure to heat reduces the duration of the attack. The attacks do not have any clear periodicity. As a result of repeated attacks, the inner layer of arterioles becomes thinner, and accumulations of blood cells, in particular platelets, often form in them (thrombosis).
After several years of illness, the skin over the arterioles becomes smooth, thinned and tense, and the subcutaneous structures seem to disappear (atrophy). In cases where the attack lasts several hours, tiny skin ulcers may develop, for example, on the fingertips. Raynaud's syndrome, as mentioned above, is a manifestation of other diseases and conditions. This syndrome is often observed in atherosclerosis obliterans and thromboangiitis of the extremities, so-called systemic connective tissue diseases: systemic lupus erythematosus, rheumatoid arthritis, etc. In some cases, Raynaud's syndrome develops as a result of side effects of drugs, in particular the so-called? - (beta) adrenergic blockers. It can be difficult to distinguish between attacks that are due to either the disease or Raynaud's syndrome. Raynaud's syndrome can occur in people of both sexes; unilateral lesions are more common, i.e. attacks occur, for example, only with the participation of one of the hands. If no other possible causes of Raynaud's phenomenon are identified within an average of two years, then they speak of Raynaud's disease. One of the methods for diagnosing Raynaud's phenomenon is plethysmography of fingers before and after their contact with cold water. This method is bloodless (non-invasive); it consists of a graphical recording of vascular tone.
General measures to treat Raynaud's disease include avoiding hypothermia and wearing gloves in cold weather. Smoking patients are advised to give up this bad habit, as nicotine promotes arterial spasm. In some cases, psychotherapy and sedative medications can be effective. Drug treatment of Raynaud's disease consists of taking vasodilating and antispastic medications, in particular the so-called? - (alpha) adrenergic blockers (doxazosin, prazosin). In rare cases, especially when skin ulcers that are resistant to treatment are formed, surgical interruption of the influences of the sympathetic nervous system (sympathectomy) is resorted to. Treatment of Raynaud's syndrome comes down to treating the diseases and conditions that caused it, as well as eliminating drug overdose. Measures and medications used to treat Raynaud's disease may also be effective.
Treatment
An important point is to eliminate etiological factors - smoking, hypothermia, etc.
Complex therapy includes antispasmodics (No-spa 2t x 3 times a day or Halidor 200 mg x 2 times a day), desensitizing drugs - for example, Claritin 1t x 1 time a day.
Otherwise, conservative therapy for the disease is practically no different from that for obliterating atherosclerosis. Course treatment should be carried out at least 2 times a year.
For obliterating endarteritis, lumbar sympathectomy is more widely used, which is currently performed using minimally invasive methods. Carrying out reconstructive operations on blood vessels, as a rule, is not possible due to diffuse damage to the arterial bed.
The possibilities of physiotherapy are wider - UHF therapy, Bernard currents, electrophoresis.
Sanatorium-resort treatment is indicated in the form of radon and hydrogen sulfide baths.
In our clinic we perform:
- Microsurgical bypass of the arteries of the leg and foot
The Innovative Vascular Center has been developing technology for microsurgical operations for obliterating endarteritis for more than 10 years. Given the poor condition of the vascular bed and the lack of target arteries for bypass surgery, these operations are labor-intensive and not as successful as for atherosclerosis. However, our clinic has developed original approaches to include 3rd-4th order arteries into the bloodstream using 25-40x optical magnification and special surgical instruments. Our surgeons manage to restore blood circulation and preserve the leg in 80% of patients with gangrene of the fingers against the background of obliterating endarteritis.
- Transplantation of a feeding flap on a vascular pedicle
In approximately 40% of patients with Buerger's disease, target arteries for bypass grafting cannot be found in the foot. Until 2011, we, like most vascular surgeons in the world, considered such cases hopeless from the point of view of restoring blood flow. However, in 2011, our center began to develop methods of plastic microsurgery to improve blood supply to tissues. The idea is to transplant a complex of tissues onto a vascular pedicle. In a certain area, a section of tissue is taken that receives blood supply through the feeding vessels. This tissue complex is then transplanted onto the lower leg or foot of a patient with endarteritis.
Since this flap receives independent nutrition, it begins to grow into surrounding tissues with poor blood circulation. During the growth of this flap, new vessels grow into the ischemic tissue, improving nutrition. This unique method allows you to restore blood circulation, eliminate the symptoms of critical ischemia and save the leg for most patients with Buerger's disease. In Russia, such operations are performed only at the Innovative Vascular Center. The greater omentum, radial or thoracodorsal flap can be used as a donor tissue complex. The choice of flap for transplantation depends on the degree of damage to surrounding tissues and the shape of the wound defect. It is very important to prepare the wound defect for flap transplantation, which is carried out using modern wound cleansing technologies.
Thromboangiitis obliterans (Buerger's disease)
The disease is quite rare. The course and clinical manifestations are similar to obliterating endarteritis, but differ in a more aggressive course. One of the main symptoms that distinguishes Buerger's disease from other obliterating diseases of the extremities is migrating thrombophlebitis, mainly of the superficial veins. The disease is characterized by a chronic course with periodic exacerbations and remissions.
Treatment of thromboangiitis obliterans is not much different from therapy for endarteritis obliterans. If venous thrombosis occurs, they are treated according to the general rules (see treatment of venous thrombosis).
Affected Populations
Buerger's disease is a very rare disease, most cases affecting young or middle-aged smokers with the onset of symptoms before the age of 40-45 years. In recent years, more women have been reported in the medical literature. Some scientists suggest that this is due to an increase in the number of women smoking. While the ratio of affected men to women was once 100:1, recent articles in the medical literature suggest that the ratio may be 10:1 or more. In very rare cases, the disease has been observed in non-smokers.
Buerger's disease is extremely rare in Europe, but is more common in other parts of the world, especially parts of Asia and the Far and Middle East. The estimated incidence ranges from 12.6 to 20 per 100,000 people in the general population. The disease is more common in countries with heavy tobacco use.
Although the majority of cases are associated with tobacco smoking, the disorder has also been observed in people who do not smoke but use smokeless tobacco (such as chewing tobacco).