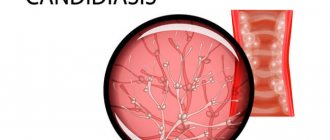
Vaginal candidiasis during pregnancy is diagnosed in 9 out of 10 women. The disease develops against the background of hormonal changes and a decrease in the body's protective functions. The causative agent of the infectious disease is a fungus of the genus Candida (Candida). This microorganism is a conditionally pathogenic microorganism that lives on the skin and mucous membranes of almost any healthy person. The activity and vital functions of candida are controlled by the immune system, however, with the slightest disruption, the balance of the intravaginal microflora is disrupted, which leads to the activation of the infectious pathogen.
Candidiasis in pregnant women is mainly diagnosed at the end of the second and beginning of the third trimester. It is important to identify thrush in time and try to treat it before birth. This will help avoid complications not only in the expectant mother, but also in the child, whose risk of infection is very high when passing through the affected birth canal. Treatment of a fungal disease should be carried out under the strict supervision of a gynecologist, who selects medications, taking into account the patient’s position and the individual characteristics of her body.
Thrush during pregnancy
Candidiasis in women during pregnancy is diagnosed very often. This disease is caused by the yeast fungus Candida, which lives in the body of almost every healthy person. Thrush is not an independent disease, and its progression is associated with a weakening of the immune system, which, under the influence of negative exogenous and endogenous factors, is no longer able to perform its functions and restrain the active growth and activity of opportunistic microorganisms.
At the first symptoms of a fungal disease, you should consult your gynecologist and begin treatment as soon as possible. If there is no therapy, candidiasis becomes chronic, relapsing, from which it is quite difficult and sometimes impossible to cure. In addition, it is important to remember that in the absence of treatment, the risk of infection of the child during intrauterine development or as it passes through the birth canal increases.
Thrush is usually diagnosed in women in the last trimester. The risk of developing the disease at the beginning of pregnancy increases in women who have had candidiasis at least once before conception. Therefore, in order to prevent the progression of thrush during such an important and crucial period, at the time of planning a child, it is advisable to undergo a comprehensive examination and, if necessary, undergo treatment for both partners.
Factors for the appearance of thrush
Immediately after conception, colossal changes begin to occur in the female body, affecting the functioning of internal organs and systems. Hormonal levels change, increased production of progesterone inhibits the activity of the immune system, which ceases to fully perform its functions, one of which is control of the activity of opportunistic microflora. In addition, hormonal changes disrupt the balance of intravaginal microflora, making a woman more susceptible to infection.
In addition to these specific features, candidiasis during pregnancy can be provoked by the following negative internal and external factors:
- Dysbacteriosis of the digestive organs, in which pathogenic intestinal microorganisms penetrate the vagina.
- Infection from a sick partner during sexual intercourse.
- Abuse of foods rich in carbohydrates, which are an ideal environment for fungal growth. A pregnant woman should exclude sugar, baked goods, sweets, pastries, and carbonated drinks from the menu.
- Uncontrolled use of hormonal drugs, antibiotics, immunosuppressants. These medications negatively affect the balance of the body's microflora, promoting the active reproduction of pathogenic microorganisms.
- Chronic endocrine disorders, such as diabetes, thyroid disease, metabolic disorders. Before conception, it is advisable to undergo a comprehensive diagnosis in order to identify pathology in time and normalize the functioning of the affected systems.
- Regular wearing of low-quality underwear made from synthetic fabrics. Synthetic underwear does not allow air to pass through, as a result of which bacteria begin to actively multiply on the mucous membrane of the genital organs, which is an ideal breeding ground for fungal infections. It is recommended to choose comfortable, comfortably fitting models, made from natural fabric that does not disturb natural air exchange.
- Avitaminosis. A deficiency of vital vitamins and elements contributes to a decrease in protective functions, so a pregnant woman becomes more susceptible to various gynecological infections.
- Stress, nervous overload, irregular daily routine. Stress factors reduce the protective functions of a pregnant woman, who becomes susceptible to infectious diseases. Therefore, it is important to learn to control your emotional background, try not to take everything to heart, establish a daily routine, rest more, walk outside, and receive only positive emotions.
- Hypothermia. In a woman in a position, the immune defense is already unstable and weakened, and if the body is subjected to stress such as hypothermia, additional problems can occur in the form of candidiasis.
Features of therapy
Instructions for use
Treatment for thrush should begin immediately after the diagnosis is made.
To get rid of candidiasis in a child’s mouth using Candida, you will need to take a cotton swab, drop 3-4 drops of solution on it and lubricate the affected areas of the mucous membrane. It is recommended to remove white plaque after feeding, three times a day. The baby’s mouth should be treated continuously for a week, but the first improvements are observed already on the 3rd day.
Vaginal tablets can cure thrush in women. To do this, you will need to lie on your back, bend your knees and insert the medicine deep into the vagina. The dosage is determined by the attending physician, but is usually 500 mg 1 time before bedtime. “Candide” in powder form is applied to the problem area of the skin 3-4 times a day. In order for the therapeutic course to give the most positive results, it is important to carry out procedures regularly and not stop treatment after the disappearance of painful symptoms.
The main symptoms of candidiasis in pregnant women
The characteristic signs of thrush during pregnancy begin to worry already at the initial stages of the development of the pathology. Women experiencing a fungal infection experience the following pathological symptoms:
- hyperemia, inflammation and swelling of the external genitalia;
- whitish, cheesy vaginal discharge with an unpleasant, sour odor;
- itching in the genitals, intensifying during movement or sex;
- pain, burning when urinating.
In a chronic course, the symptoms of candidiasis are erased and less pronounced. In any case, if a woman discovers suspicious discharge with a cheesy consistency, but there is no itching or burning, you should still not delay a visit to the gynecologist, because in some cases candidiasis is a consequence of the progression of other diseases that are more dangerous for the unborn child.
Diagnosis of candidiasis during pregnancy
After collecting anamnesis and visual examination, the gynecologist will give a referral for a diagnostic examination, which will help identify the pathogen and select the most effective treatment regimen.
To clarify the diagnosis, a referral is given for the following laboratory tests:
- Microflora smear. A smear is taken from the inner walls of the vagina, which is then examined under a microscope. With vaginal candidiasis, fungi and other pathogens are present in large quantities in the vaginal contents.
- Bacterial culture. Allows you to determine which fungi inhabit the vagina, as well as select effective drugs for therapy.
If the diagnosis of vaginal candidiasis is confirmed, the doctor immediately draws up a treatment plan. Treatment of candidiasis during pregnancy involves the use of antifungal drugs approved during pregnancy. Depending on the stage at which the disease is diagnosed, the doctor may prescribe both local and systemic antimycotics. To remove pathological symptoms. Additionally, local anti-inflammatory and antiseptic agents are prescribed. To maintain immunity, the doctor may recommend taking a course of immunomodulating and restorative drugs, probiotics with bifidobacteria.
If thrush occurs against the background of other internal diseases, additional consultations are prescribed with specialists such as:
- endocrinologist;
- gastroenterologist;
- immunologist;
- nephrologist, etc.
In addition to taking medications, a pregnant woman should follow a gentle diet, minimizing the consumption of foods rich in carbohydrates. Treatment in the initial stages helps to quickly get rid of the infection and unpleasant symptoms, and avoid dangerous complications.
The effectiveness of the drug Candide for vulvovaginal candidiasis
An analysis of the medical literature of recent years shows increased interest in the problem of mycoses in general and candidiasis of the mucous membranes in particular. Mycoses are a widespread group of infections caused by a large number (more than 200) species of various pathogenic and opportunistic fungi (1, 2).
Table 1. Clinical manifestations of acute vulvovaginal candidiasis
Table 2. Frequency of isolation of yeast species from vaginal discharge in patients with vulvovaginal candidiasis
Table 3. Comparative assessment of the state of vaginal microcenosis before and after treatment with VVC in patients of group I
A brief analysis of the current state of the complex problem of mycoses shows:
- a sharp recent increase in the frequency and severity of fungal infections, including those with a chronic course;
- the importance of immunodeficiency states in the occurrence, pathogenesis, course and outcome of the disease, especially in connection with the initial immunodeficiencies;
- a large share of mycoses in the problem of so-called opportunistic infections;
- the influence, paradoxically, of advances in other areas of medicine (successes in antibiotic and hormonal therapy, combination therapy, a number of surgical interventions) on the increase in the frequency and duration of mycoses;
- difficulties in treating mycoses due to the variety of fungal species with different properties and the localization of the pathological process.
In modern conditions, in many countries of the world, including Russia, there has been an increase in vaginal infections, which firmly occupy a leading place in the structure of obstetric and gynecological morbidity. It is known that vaginal discharge is a symptom of infectious diseases of various etiologies, an indicator of trouble and the risk of infection spreading to the upper parts of a woman’s reproductive system. Therefore, timely differential diagnosis using clinical and laboratory research methods followed by adequate etiotropic therapy is extremely important (3, 4, 5).
One of the most common reasons for women to visit a doctor is genital lesions caused by yeast-like fungi of the genus Candida
– vulvovaginal candidiasis (VVC).
According to summary data, asymptomatic carriage of Candida
is found in the intestines of 20-50% of healthy people, on the oral mucosa in 20-60%, and in the vagina in 15-20% of non-pregnant women. According to the literature, 75% of women of reproductive age have at least one episode of vaginal candidiasis. In pregnant women, this disease occurs in 30-40% of cases; before childbirth, this figure can reach 45-50%. In this case, yeast-like fungi are found in small quantities (3 CFU/ml).
At the same time, yeast-like fungi of the genus Candida
are part of the normal vaginal microflora and 10-20% of women are candida carriers. This contingent of women has no clinical manifestations of the disease when yeast-like fungi are detected in a low titer according to microbiological research methods. Under the influence of certain exo- and endogenous factors, candidiasis can become clinically pronounced and cause disease (1, 6, 7).
It should also be noted that there is a high incidence of vaginal candidiasis during pregnancy, which is due to a number of factors: changes in hormonal balance; accumulation of glycogen in the epithelial cells of the vagina; immunosuppressive effect of high levels of progesterone and the presence of immunosuppressive factor associated with globulins in the blood serum. A direct relationship has been established between gestational age and the incidence of vaginal candidiasis.
Candidiasis infection is often associated with disturbances of the vaginal microcenosis. Depending on the state of the vaginal microcenosis, 3 forms of Candida
-vaginal infections (6, 8, 9):
- asymptomatic candidiasis, in which there are no clinical manifestations of the disease, yeast-like fungi are detected in a low titer (4 CFU/ml), and lactobacilli absolutely dominate among the microbial associates of the vaginal microcenosis;
- true candidiasis, in which fungi act as a monopathogen, causing a clinically pronounced picture of the disease. Candida
fungi (> 104 CFU/ml), lactobacilli (> 106 CFU/ml) are present in high titers in the vaginal microcenosis in the absence of diagnostically significant titers of any other opportunistic microorganisms; - a combination of vaginal candidiasis and bacterial vaginosis, in which yeast-like fungi participate in polymicrobial associations as causative agents of the disease. In these cases, yeast-like fungi (usually in high titer) are found against the background of a massive amount (> 109 CFU/ml) of obligate anaerobic bacteria and gardnerella with a sharp decrease in the concentration or absence of lactobacilli.
It is fundamentally important to distinguish between 2 variants of damage to the mucous membranes: with invasion of Candida spp.
and without the last one (1, 10).
Invasive candidiasis of the mucous membranes is characterized by the development of fibrinous inflammation (in typical cases, the so-called thrush), and morphological studies of smears and biopsies reveal pseudomycelium and budding yeast cells.
Based on the characteristics of the clinical picture, pseudomembranous (thrush) and erythematous/atrophic forms of the disease are distinguished. In addition, the terms complicated and secondary vaginal candidiasis are often used in foreign literature. Complicated candidiasis includes both chronic forms and atypical etiology, pronounced clinical manifestations, course against the background of severe predisposing conditions (diabetes mellitus, immunodeficiency, etc.), that is, cases that are difficult to treat. Secondary vulvovaginal candidiasis usually refers to cases of infection occurring against the background of existing non-infectious lesions of the genital organs.
With non-invasive candidiasis, the clinical picture varies significantly. The transition of candidiasis to disease is facilitated by the presence in the macroorganism of disturbances in the nonspecific and specific components of resistance at the local and systemic levels.
Currently, there is a large selection of various antimycotic agents of both local and systemic action (11, 12, 13, 14).
According to the recommendations of the CDC, the European standards for the diagnosis and treatment of sexually transmitted diseases, therapy for vulvovaginal candidiasis involves the administration of systemic azole or topical antifungal agents. In addition, it should be noted that drugs used by pregnant women for the treatment of vaginal candidiasis must meet the following requirements: low toxicity to the fetus and mother, effectiveness, tolerability, minimal frequency of development of resistance in pathogens, etc. Intravaginal use of antimycotics should be considered preferable due to a sharp decrease in systemic absorption of drugs, which minimizes the potential for undesirable effects (13, 15, 16, 17, 18, 19).
To this day, the issue of the effectiveness of using different doses of antifungal agents, in particular, drugs containing clotrimazole, remains controversial. In this regard, it seems appropriate to conduct this study.
Purpose of the study
It is necessary to evaluate the clinical and microbiological effectiveness and safety of using the drug Candide (500 mg once or 100 mg 6 times) in the treatment of acute vulvovaginal candidiasis, as well as (500 mg once) for sanitation of the birth canal before childbirth.
Materials and research methods
The study included 70 women, with an average age of 27.4 ± 1.3 years, with acute vulvovaginal candidiasis (with clinical manifestations and microbiological verification of the diagnosis).
Inclusion criteria: clinical manifestations of vulvovaginal candidiasis, as well as laboratory confirmation of an episode of this disease (budding cells, or hyphae, determined by microscopic examination; a positive result of a cultural examination of vaginal discharge to identify fungi of the genus Candida
with species identification and quantitative assessment).
To make a diagnosis of acute vulvovaginal candidiasis, a clinical and gynecological examination was used: collection of anamnestic data, patient complaints, examination of the vulva, vaginal mucous membranes and cervix in the speculum, bimanual gynecological examination. Microbiological diagnosis was based on assessment of the state of the vaginal microcenosis based on the results of a comprehensive study: microscopy of vaginal smears stained with Gram and cultural examination of vaginal contents.
Patients with a confirmed diagnosis of VVC were divided into the following groups:
- Group I – 20 patients treated with Candide B1, 500 mg (clotrimazole) vaginal tablets administered intravaginally once;
- Group II – 20 patients who received therapy with Candide B6, 100 mg (clotrimazole) vaginal tablets, 1 tablet intravaginally at night for 6 days;
- Group III - 30 women with full-term pregnancy who received the drug Candide B1 500 mg (clotrimazole) vaginal tablets administered intravaginally once for sanitation of the birth canal.
Monitoring the effectiveness of therapy was assessed after 7-10 days and after 1 month. (outside of pregnancy) from the start of treatment based on the dynamics of the patient’s complaints, clinical signs of the disease: the presence of characteristic vaginal discharge, itching, burning, hyperemia and swelling of the vaginal and vulvar mucosa. In microbiological examination, treatment was considered effective in the absence of a pronounced leukocyte reaction according to microscopy and elimination of the fungus during microscopy and cultural examination during dynamic observation.
The clinical effectiveness of the drugs used was assessed according to the following criteria:
- good effect – cure: absence of subjective symptoms (itching, pain, burning) and laboratory signs of the underlying disease, absence of relapses of VVC within 12 months. from the start of therapy;
- satisfactory effect - improvement: absence of laboratory signs of the underlying disease, positive dynamics of subjective (itching, pain, burning) and objective symptoms, insufficient to classify the effect as a “good effect”;
- unsatisfactory effect - lack of effect from the therapy or worsening of subjective and objective symptoms, repeated relapses of vulvovaginal candidiasis.
Research results
All 70 patients included in the study were diagnosed with VVC based on complaints, gynecological examination, clinical manifestations of the disease and confirmed by microscopy of vaginal smears and cultural examination of vaginal contents. Clinical symptoms noted in patients before the start of therapy are presented in Table 1.
Most patients complained of heavy discharge from the genital tract - 67 (95.7%) women, accompanied by itching in the vaginal area - in 68 (97.1%) and vulva - in 63 (90%). Dyspareunia was noted in 39 (55.7%) women; burning in the area of the external genitalia – in 27 (38.6%), dysuric disorders – in 20 (28.6%) patients. It is worth noting that during a gynecological examination, all patients noted hyperemia and swelling of the mucous membrane of the vagina, cervix and vulva, which were pronounced.
Microbiological examination of patients showed that 59 women (84.3%) were diagnosed with the classic variant of VVC, 10 (14.3%) had a combined form of bacterial vaginosis and VVC, in 1 case (1.4%) fungi were isolated in association with Escherichia coli and Staphylococcus epidermidis in high titer in the absence of lactobacilli. When identifying yeast fungi (Table 2), it was found that they were represented by the genus Candida
. In 68 women (97.1%), yeast fungi were isolated in monoculture and in 2 (2.9%) - in association.
A total of 72 fungal strains were identified: 69 strains (95.8%) of Candida
albicans
and 3 strains (4.2%) of non-
albicans
(
Candida glabrata
- 2 and
Candida parapsilosis
- 1).
The effectiveness of VVC treatment was assessed during a control microbiological study 7 days after treatment. Comparative results of assessing the state of the vaginal microcenosis, according to microscopy of a vaginal smear and cultural examination, are presented in Table 3.
It was found that during a control study, the elimination of yeast fungi from vaginal discharge was achieved in 69 women (98.6%). In 1 patient (1.4%), the microscopic picture of the vaginal microcenosis corresponded to the norm, but a cultural study isolated Candida
glabrata
in a low titer (3 lg CFU/ml).
There were no clinical manifestations or complaints from the patient. The coincidence of the biocode and sensitivity to antimycotics of Candida glabrata
before and after treatment indicates their identity.
As for sensitivity to antimycotics, the Candida glabrata
retained sensitivity to all drugs studied, including imidazoles, which include clotrimazole, the basis of the drug Candide.
In all patients with the classic form of VVC, when yeast fungi vegetate against the background of normal flora, elimination of fungi was achieved after treatment. The microcenosis in 57 of 59 patients met the normal criteria, and in 2 cases, NV caused by Escherichia coli was diagnosed. Of the 10 patients with a combined form of VVC and BV, in 6 cases, elimination of not only the yeast fungus, but also the microflora associated with BV was achieved with subsequent restoration of lactoflora. In 4 cases, no fungi were found after treatment, and the titer of obligate anaerobes remained virtually unchanged. In the case of a combination of VVC caused by Candida
glabrata
and NV associated
with E. with oli ,
after treatment there was a significant decrease in the titer of
Candida glabrata and E. with oli
(up to 3 lg CFU/ml).
During the subsequent long-term (after 28-31 days) examination, no relapse of VVC was detected in any woman (groups I and II). None of the patients reported any adverse reactions associated with topical use of clotrimazole. In a survey conducted after the end of treatment, the majority of pregnant women considered the therapy convenient and effective.
Summarizing the results of our evaluation of therapy with the vaginal drug Candide (clotrimazole 100 and 500 mg), we can state that the introduction of a vaginal Candide tablet using an applicator is a convenient, effective and safe option for the treatment of acute vulvovaginal candidiasis. In our clinical evaluation, the administration of clotrimazole was no less effective than the use of other widely recommended drugs. At the same time, in the majority of patients receiving Candid, a rapid disappearance of the symptoms of the disease was noted, which is obviously due to the peculiarities of the pharmacokinetics of this drug. Like other investigators, we noted that treatment failure of vulvovaginal candidiasis with clotrimazole may be associated with massive colonization of the vagina with C. albicans
or the presence of non-
C. albicans
(
C. glabrata, C. parapsilosis
, etc.), therefore, in the latter case, repeated courses of therapy are advisable.
Thus, a clinical assessment of the effectiveness and tolerability of therapy with Candida vaginal tablets in the treatment of acute vulvovaginal candidiasis showed good tolerability and high efficiency of therapy with this drug. Almost all women experienced clinical recovery and microbiological cure. Repeated courses of therapy were required for patients with remaining mild clinical symptoms of vulvovaginal candidiasis. No side effects of therapy were noted in any case. High efficiency, tolerability and safety of therapy with the vaginal drug Candida, as well as the economic aspects of therapy, that is, the affordable price of the drug. It should be noted that the possibility of a single dose allows us to recommend therapy with Candida vaginal tablets as an effective method of treating vulvovaginal candidiasis.
The danger of candidiasis in pregnant women
If the treatment of candidiasis in women during pregnancy is correct and timely, neither she nor the unborn child is in any danger in terms of health. It’s another matter when the disease progresses, and the pregnant woman refuses to take the medications prescribed by the doctor for fear of harming the fetus. But it is worth noting that the modern pharmaceutical market sells many antifungal drugs that are allowed to be used already in the early stages of pregnancy. They effectively destroy fungal infection and at the same time do not have any effect on the growth and development of the fetus.
Description of the consequences of the disease
It is rare, but it happens that Candida yeast fungi penetrate the placental barrier, contributing to intrauterine infection of the fetus. But basically, a child becomes infected with thrush at the time of birth, when he moves through the birth canal affected by the fungus. Infection during childbirth can cause severe damage to the skin and mucous membranes, and the membranes of internal organs.
Candidiasis is dangerous not only for the unborn child, but also for the pregnant woman herself. Fungi negatively affect the condition of the tissues of the vagina and birth canal, helping to reduce their strength and elasticity. Therefore, immediately at the time of birth, the risk of serious injuries increases, which can cause heavy blood loss and other complications.
In addition, untreated vaginal candidiasis often causes the progression of erosive processes in the uterus. Erosion can subsequently negatively affect women's health and cause infertility.
Indications
The use of "Candida" is advisable for patients who have been diagnosed with the following pathologies:
- dermal candidiasis;
- infectious skin lesions caused by dermatophyton fungi;
- localization of fungi of the genus Candida on the mucous membrane of the vagina and vulva, and in men on the surface of the glans penis;
- stomatitis;
- candidiasis of the anorectal area;
- onychomycosis (nail fungus);
- trichophytosis;
- dermatophyte of the body, limbs, face;
- microsporia;
- erythrasma;
- dermatomycosis.
Cost of treating candidiasis in women
The cost of treating candidiasis in a medical setting is the most conservative and affordable. Before prescribing a treatment plan, our specialists will conduct a thorough examination, study in detail the results of the diagnostic examination, assess the general health of the pregnant woman, and only then select an effective therapeutic regimen, which will allow you to quickly and safely get rid of the infection and prevent the disease from becoming chronic.
You can find out how much it costs to treat vaginal candidiasis at the Healthy Family medical clinic by calling +7 (495) 185 93 07 or ordering a call back. Our administrators will contact you and answer all your questions.