The use of aceclofenac in patients with acute back pain - effectiveness and safety
Kamchatnov P.R., Radysh B.B., Mikhailova N.A., Kutenev A.V.
Low back pain (LBP) is an extremely common clinical syndrome. Depending on factors such as body weight, the nature and regularity of physical activity, age, etc., LBP occurs in 70-90% of adults. There are nonspecific LBP, compression of the spinal root (radiculopathy), as well as LBP caused by specific lesions of the spine. Depending on the duration, there are acute (lasting less than 4 weeks), subacute (from 4 to 12 weeks) and chronic (lasting more than 12 weeks) LBP.
Nonspecific LBP is caused by osteoarthritis, osteochondrosis, and changes in periarticular tissues. It usually has a benign course and regresses or decreases significantly within 4-6 weeks [30]. The most common cause of root compression is a herniated disc. Rarely (less than 1%) LBP is caused by compression fractures due to osteoporosis, ankylosing spondylitis, tumors, and infectious processes.
Establishing a diagnosis is helped by a detailed clarification of the anamnesis - the peculiarities of the occurrence of pain, the factors that provoke its appearance and ensure its reduction, the identification of concomitant somatic diseases that can lead to damage to the spine, spinal cord membranes, and nervous structures [3].
Radiological examination (CT and MRI) is the main method of instrumental diagnosis of LBP. Tomographic examination is indicated to exclude specific causes of pain in patients with increasing pain, in the presence of neurological deficits, and in cases of severe somatic diseases. Radiography does not allow obtaining reliable information about the presence and size of a herniated intervertebral disc, the true size of the spinal canal in case of stenosis, etc. If indicated, radioisotope scintigraphy is used, which makes it possible to identify local accumulation of radiopharmaceuticals in the lesions, densitometry, and ultrasound examination.
Treatment
Complete and early elimination of pain is desirable in order to actively involve the patient in the process of treatment and rehabilitation, explain to the patient the benign nature of the disease, and teach him methods of preventing exacerbation. Ensuring an optimal level of daily physical activity is important. Excessive immobilization is undesirable not only in patients with isolated LBP, but also in most patients with radiculopathy. Early activation of the patient is of exceptional importance in preventing the development of depressive disorders and the formation of pain behavior [38].
In accordance with European recommendations for the treatment of patients with acute LBP, the first-line drug for its relief is paracetamol. In terms of analgesic effect, it is equivalent to acetylsalicylic acid and is comparable to or slightly inferior to most nonsteroidal anti-inflammatory drugs (NSAIDs). The anti-pain effect is realized due to the inhibition of cyclooxygenase activity in peripheral tissues and the central anti-inflammatory effect.
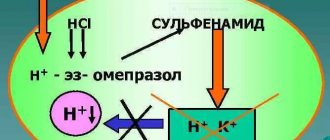
Experimental study of aceclofenac
NSAIDs are widely used - non-selective cyclooxygenase (COX) inhibitors, which have high analgesic and anti-inflammatory activity. This group includes aceclofenac (Aertal), a derivative of phenylacetylic acid (2-[2,6 - dichlorophenyl) amino] phenylacetoacetic acid), which is close in structure to diclofenac. In addition to inhibition, COX inhibits the expression of cell adhesion molecules (in particular, L-selectin), suppresses the adhesion of neutrophils to the endothelium, providing a pronounced anti-inflammatory effect [16], also due to the activation of the synthesis of interleukin-1 receptor antagonists and the suppression of the formation of nitric oxide [27].
Aceclofenac itself has a moderate inhibitory effect on COX types 1 and 2, however, under conditions of local inflammation by polymorphonuclear leukocytes and monocytes, aceclofenac is partially metabolized into diclofenac and 4-hydroxydiclofenac, due to which COX activity is inhibited [43].
Aceclofenac is able to prevent the degeneration of cartilage tissue. In the experiment, it demonstrated chondroprotective properties, providing interleukin-1-mediated suppression of the production of metalloproteinases, which stimulated the synthesis of proteoglycans by chondrocytes [4]. In a culture of cartilage tissue cells from patients with osteoarthritis, the use of aceclofenac was accompanied by an increase in the synthesis of proteoglycans and hyaluronic acid [6]. Aceclofenac, while ensuring the preservation of cartilage tissue, does not significantly affect the proliferation of tendon cells, without causing their hyperplasia.
Clinical effectiveness of aceclofenac
To date, considerable experience has been accumulated in the use of aceclofenac in patients with articular pathology. Analysis of the effectiveness of the drug in inflammatory diseases and in relieving pain syndromes allowed us to establish its anti-inflammatory effect, equivalent to ketoprofen, indomethacin and diclofenac in patients with rheumatoid arthritis, diclofenac and piroxicam for osteoarthritis of the knee joint, and indomethacin and naproxen for ankylosing spondylitis.
It is believed that the analgesic activity of 100 mg of aceclofenac in its duration of action exceeds that after taking 650 mg of paracetamol [8].
The authors of a review devoted to the analysis of the use of aceclofenac for the relief of acute pain syndromes (pathology of the ENT organs, dental, gynecological diseases, LBP) noted the high effectiveness of the drug [24]. The results of a double-blind, randomized study of the effectiveness of aceclofenac (200 mg/day) and paracetamol (3000 mg/day) in patients with osteoarthritis of the knee joint (168 patients included, treatment duration - 6 weeks) showed greater effectiveness of aceclofenac with better tolerability [5 ].
A multicenter, randomized, double-blind study was devoted to a comparative study of the effectiveness of aceclofenac (200 patients received 100 mg 2 times a day) and diclofenac (197 patients, 50 mg 3 times a day) for osteoarthritis of the knee joint [42]. As a result of a 12-week course of treatment in both groups, there was significant significant relief of pain and an increase in range of motion in the affected joints. However, a more pronounced effect and early normalization of joint mobility were recorded with the use of aceclofenac. A larger number of patients noted improvement after taking aceclofenac (71 and 59% after taking diclofenac), while the frequency of side effects with its use was significantly lower (1.0 and 6.6%). Similar results were obtained in a comparative multicenter study of aceclofenac and diclofenac in a similar group of patients with osteoarthritis of the knee joint [12]. The differences in the effectiveness of the drugs were not so pronounced, however, the frequency of side effects when taking aceclofenac was 5.9%, diclofenac - 11.5%, and an increase in the level of aminotransferases, which caused drug withdrawal, was observed in 0.6% of patients receiving aceclofenac, and in 3.0% of patients taking diclofenac.
A 12-week randomized, multicenter, double-blind study compared the effectiveness of aceclofenac (100 mg 2 times/day, 190 patients) and naproxen (500 mg 2 times/day, 184 patients) in patients with osteoarthritis of the knee joint [23]. There were no significant differences in the effectiveness of the drugs between the groups, however, the frequency of side effects was lower in the group of patients receiving aceclofenac (34 cases in 24 patients - 12.6%) compared to patients receiving naproxen (43 cases in 30 patients - 16.6%). 3%), and the differences also concerned gastrointestinal complications. A comparison of the effectiveness of aceclofenac (100 mg 2 times / day, 123 patients) and piroxicam (20 mg / day, 117 patients) was carried out in patients with osteoarthritis of the knee joint [31] during an 8-week randomized, multicenter, double-blind study. The effectiveness of the drugs turned out to be comparable, but the effect of using aceclofenac occurred earlier (in the 2nd week) compared to piroxicam (in the 4th week). Side effects were observed in 24 and 33 patients, respectively, despite the fact that detection of occult blood in feces was half as common after taking aceclofenac.
As part of a 6-month multicenter, double-blind study, 170 patients received aceclofenac (100 mg 2 times/day) and diclofenac (50 mg 3 times/day) [29]. Reduction of pain and improvement of movements occurred in both groups, however, motor disorders were relieved to a greater extent in patients receiving aceclofenac (17 and 22%, respectively).
Data from clinical studies (pronounced analgesic effect, good tolerability), as well as the unique effect of the drug on inflammatory mediators, speaks in favor of considering aceclofenac as the drug of choice for long-term therapy of patients with osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and some other chronic degenerative lesions joints [33].
The pronounced anti-inflammatory and analgesic effects of aceclofenac led to the study of its effectiveness in patients with LBP. One of the first such studies was devoted to comparing the effectiveness of aceclofenac (135 patients, 100 mg 2 times a day) and tenoxicam (138 patients, 20 mg once a day) in patients with ankylosing spondylitis [39]. The study was multicenter, double-blind and lasted 12 weeks. Both drugs demonstrated high efficacy and comparable tolerability.
A multicenter, randomized, double-blind study compared the effectiveness of aceclofenac (100 mg 2 times/day) and diclofenac resinate (75 mg 2 times/day) in patients with acute nonspecific LBP [36]. The study included 227 patients; the course of treatment was 10 days. The timing and quality of pain relief were comparable in both groups, however, the use of aceclofenac was characterized by a significantly lower number of side effects.
Portability
Widespread, especially long-term, use of non-selective COX inhibitors is associated with a high risk of gastric bleeding. Due to the relatively low risk of gastrointestinal complications, the possibility of using selective COX-2 inhibitors is of great interest. A number of large randomized clinical trials performed in a double-blind manner have convincingly proven that selective COX-2 inhibitors have a significantly lower risk of gastrointestinal damage compared to non-selective drugs. Convincing results were obtained in the CLASS and VIGOR studies [7,37]. Aceclofenac inhibits the formation of COX-2 to a greater extent, as a result of which the incidence of serious gastrointestinal complications with its use is significantly lower than that of other NSAIDs (piroxicam, indomethacin, tenoxicam and ketoprofen) [19].
The tolerability of aceclofenac was studied in a 12-month prospective, open-label, multicenter study, SAMM [20]. Of 10,142 patients suffering from rheumatoid arthritis, ankylosing spondylitis and osteoarthritis, 2 groups were formed: the first (n=7890) consisted of patients receiving aceclofenac (100 mg 2 times a day), the second (n=2252) - diclofenac (according to 75 mg 2 times/day). The duration of treatment was 168 and 170 days, respectively. The total number of side effects, as well as the number of patients who stopped treatment due to intolerance, turned out to be significantly lower in the group receiving aceclofenac. The incidence of gastrointestinal reactions was 10.6 and 15.2%, respectively. The incidence of nausea, abdominal pain and diarrhea leading to discontinuation of treatment was 46, 65 and 41% lower, respectively, in the group of patients taking aceclofenac.
A slightly later Pan-European study included 23,407 patients with inflammatory and degenerative joint diseases [25]. Significant improvement, according to both patients and treating physicians, occurred in 84% of patients receiving aceclofenac, while 90% of them remained adherent to treatment. The results of the study made it possible to recommend aceclofenac for the relief of both acute and chronic pain syndromes.
Almost at the same time, a review of the results of studying the effectiveness of aceclofenac was published, obtained in the course of studies of different designs with various comparator drugs (diclofenac, naproxen, piroxicam, indomethacin, tenoxicam and ketoprofen) - a total of about 150 thousand patients [13]. The drug was noted to be sufficiently effective for relieving pain or inflammation with a course of treatment lasting from 2 to 6 months. along with a low incidence of side effects.
A large-scale study was carried out in the UK to establish the incidence of gastrointestinal and other complications due to the use of non-steroidal anti-inflammatory drugs [34]. The authors compared the risk of developing various complications due to oral administration of aceclofenac (200 mg/day), meloxicam (7.5 and 15 mg/day) and rofecoxib (25 mg/day). It was found that the frequency of side effects (number of cases/106 daily doses of the drug sold in the country) was 8.7 for aceclofenac (CI 6.1 - 12.0), 24.8 for meloxicam (CI 23.1-26.6) and 52.6 (CI 49.9-55.4) for rofecoxib. The use of aceclofenac was associated with a significantly lower incidence of gastrointestinal bleeding and abdominal pain. When taking aceclofenac, a significantly lower number of gastrointestinal complications, cases of abdominal pain, and hepatotoxicity were observed compared with rofecoxib. In general, it turned out that the best tolerability was observed with aceclofenac.
The use of selective COX-2 inhibitors is associated with an increased risk of cardiovascular complications, primarily acute myocardial infarction and an increase in systemic blood pressure [28,44]. However, this property of the drugs has not been confirmed in all studies. Thus, an observation of more than 30 thousand patients with osteoarthritis and rheumatoid arthritis who received diclofenac (150 mg/day) or eotricoxib (60-90 mg/day) established an almost identical risk of thrombotic complications when taking them [9]. The study cited above [34] recorded a significantly lower incidence of thrombotic complications and cases of increased blood pressure compared to meloxicam and rofecoxib.
Pharmacokinetics of aceclofenac
When administered orally, aceclofenac is quickly and completely adsorbed in the intestine and after 1.5-2 hours reaches its maximum concentration in the blood. The drug does not have cumulative activity, and its pharmacokinetics does not depend on the age of the patients. Prescribed orally 100 mg 2 times/day.
Contraindicated in case of exacerbations of gastric and duodenal ulcers, a history of the “aspirin triad,” or hematopoietic disorders of unknown etiology. The drug should not be used in the third trimester of pregnancy; its use in the first and second trimesters of pregnancy, as well as during lactation, is possible after a careful assessment of the benefit-risk ratio. The use of aceclofenac in children and adolescents under the age of 18 is not recommended.
With the simultaneous use of other drugs with aceclofenac, it is possible to increase the plasma concentrations of digoxin, phenytoin, lithium and reduce the effectiveness of diuretics and antihypertensive drugs. When taking aceclofenac and corticosteroids or other NSAIDs, the risk of developing side effects from the gastrointestinal tract increases. When used with acetylsalicylic acid, a decrease in the concentration of aceclofenac in the blood plasma is possible. With the simultaneous use of indirect anticoagulants, the risk of bleeding increases.
The presented information about the effectiveness and tolerability of aceclofenac (Aertal) allows us to consider it as the drug of choice in patients with acute back pain.
Literature
1. Badokin V.V. Efficacy and safety of aceclofenac in patients with osteoarthritis. RMJ. 2007; 13: 392-397. 2. Neverov V.A., Kurbanov S.Kh. Restorative treatment of degenerative-dystrophic diseases of large joints. Vestn. hir. them. I.I. Grekova 2004;163(2):97-108. 3. Nikiforov A.S., Konovalov A.N., Gusev E.I. Clinical neurology. In 3 volumes - Moscow: “Medicine”, 2002. 4. Akimoto H, Yamazaki R, Hashimoto S et al. A major metabolite of aceclofenac 4'hydroxy aceclofenac suppresses the interleukin-1 induced production of promatric metalloproteinases and release of sulfated-glycosaminoglycans from rabbit articular chondrocytes. Eur J Pharmacol 2000; 401(3): 429-436. 5. Batlle-Gualda E., Roman Ivorra J., Martin-Mola E. et al. Aceclofenac vs paracetamol in the management of symptomatic osteoarthritis of the knee: a double-blind 6-week randomized controlled trial. Osteoarthritis Cartilage. 2007; 15(8):900-908. 6. Blot L., Marcelis A., Devogelaer J.-P., Manicourt D.-H. Effects of diclofenac, aceclofenac and meloxicam on the metabolism of proteoglycans and hyaluronan in osteoarthritic human cartilage. British Journal of Pharmacology 2000; 131: 1413 – 1421. 7. Bombardier C., Laine L., Reicin A. et al.. Comparison of upper gastrointestinal toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med 2000; 343:1520-8. 8. Brogden R., Wiseman L. Aceclofenac. A review of its pharmacodynamic properties and therapeutic potential in the treatment of rheumatic disorders and in pain management. Drugs. 1996; 52(1): 113-124. 9. Cannon C., Curtis S., FitzGerald G. et al. Cardiovascular outcomes with etoricoxib and diclofenac in patients with osteoarthritis and rheumatoid arthritis in the Multinational Etoricoxib and Diclofenac Arthritis Long-term (MEDAL) program: a randomized comparison. Lancet. 2006; 18; 368(9549):1771-1781. 10. Carrabba M., Paresce E., Angelini M. et al. A comparison of the local tolerability, safety and efficacy of meloxicam and piroxicam suppositories in patients with osteoarthritis: a single-blind, randomized, multicentre study. Curr Med Res Opin. 1995;13(6):343-55. 11. Clare J., Tate S., Nobbs M., Romanos M. Voltage-gated sodium channels as therapeutic targets. Drug Discov Today 2000; 5:506-520. 12. Diaz C., Rodriquez de la Serna A., Geli C., Gras H. Efficacy and tolerance of aceclofenac versus diclofenac in the treatment of knee osteoarthritis. A multicenter study. Eur J Rheumatol Inflamm 1996; 16: 17-22. 13. Dooley M., Spencer C., Dunn C. Aceclofenac: a reappraisal of its use in the management of pain and rheumatic disease. Drugs. 2001;61(9):1351-1378. 14. Dougados M., Gueguen A., Nakache J.-P. et al. Ankylosing spondylitis: what is the optimal duration of a clinical study? A one year versus a 6 weeks non-steroidal anti-inflammatory drug trial. Rheumatology 1999;38:235-244 15. Gilbert F, Grant A, Gillan M et al. Scottish Back Trial Group. Low back pain: influence of early MR imaging or CT on treatment and outcome-multicenter randomized trial. Radiology. 2004; 231: 343-351. 16. Gonzalez-Alvaro I., Carmona L., Diaz-Gonzalez F. et al. Aceclofenac, a new nonsteroidal antiinflammatory drug, decreases the expression and function of some adhesion molecules on human neutrophils. J Rheumatol. 1996; 23(4): 723-729. 17. Harreby M., Nygaard B., Jessen T. et al. Risk factors for low back pain in a cohort of 1389 Danish school children: an epidemiologic study. Eur Spine J. 1999; 8(6): 444-450. 18. Harris A. Handicapped and Impaired in Great Britain, Part I. London, England: Social Survey Division, Office of Population Census and Surveys. Her Majesty's Stationary Office; 1971. 19. Henrotin Y, De Leval H, Mathy-Hartet M et al. In vitro effects of aceclofenac and its metabolites on the production by chondrocytes of inflammatory mediators. Inflamm Res 2001; 50: 391-399. 20. Huskisson E., Irani M., Murray F. A large prospective open-label, multicentre SAMM study, comparing the safety of aceclofenac in patients with rheumatic disease. Eur J Rheumatol Inflamm 2000; 7:1-7. 21. Koes B., van Tulder W., Thomas S. Diagnosis and treatment of low back pain. BMJ 2006;332;1430-1434. 22. Koleck M. Mazaux, J. Rascle N. et al. Psycho-social factors and coping strategies as predictors of chronic evolution and quality of life in patients with low back pain: A prospective study. European Journal of Pain. 2006; 10:1-11. 23. Korsanoff D., Frerick H., Bowdler J., Montull E. Aceclofenac is a well-tolerated alternative to naproxen in the treatment of osteoarthritis. Clin Rheumatol 1997; 16 (1): 32-8. 24. Legrand E. Aceclofenac in the management of inflammatory pain. Expert Opin Pharmacother. 2004; 5(6): 1347-1357. 25. Lemmel E., Leeb B., De Bast J., Aslanidis S. Patient and physician satisfaction with aceclofenac: results of the European Observational Cohort Study (experience with aceclofenac for inflammatory pain in daily practice). Aceclofenac is the treatment of choice for patients and physicians in the management of inflammatory pain. Curr Med Res Opin. 2002;18(3):146-153. 26. Li Y., Gorassini M., Bennett D. Role of persistent sodium and calcium currents in motoneuron firing and spasticity in chronic spinal rats. Neurophysiology 2004; 91:767-783. 27. Maneiro E., Lopez-Armada M., Fernandez-Sueiro J. et al. Aceclofenac increases the synthesis of interleukin 1 receptor antagonist and decreases the production of nitric oxide in human articular chondrocytes. J Rheumatol. 2001; 28(12): 2692-2699. 28. Mukherjee D., Nissen S., Topol E. Risk of cardiovascular events associated with selective COX-2 inhibitors. JAMA. 2001; 286:954-9. 29. Pasero G., Marcolongo R., Serni U. et al. A multi-centre, double-blind comparative study of the efficacy and safety of aceclofenac and diclofenac in the treatment of rheumatoid arthritis. Curr Med Res Opin. 1995;13(6):305-315. 30. Pengel L., Herbert R., Maher C., Refshauge K. Acute low back pain: systematic review of its prognosis. BMJ. 2003; 327: 323-326. 31. Perez Busquer M., Calero E., Rodriguez M. et al. Comparison of aceclofenac with roxicam in the treatment of osteoarthritis. Clin Rheumatol 1997; 16 (2): 154-59. 32. Pincus T., Burton A., Vogel S., Field A. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine. 2002; 27: 109-120. 33. Reginster J., Paul I., Henrotin Y. What is the role of aceclofenac in the therapeutic arsenal against chronic osteoarthritis pathologies? Rev Med Liege. 2001; 56(7): 484-488. 34. Raber A., Heras J., Costa J. et al. Incidence of spontaneous notifications of adverse reactions with aceclofenac, meloxicam, and rofecoxib during the first year after marketing in the United Kingdom. Therapeutics and Clinical Risk Management 2007:3(2) 225-230 35. Rudwaleit M., Metter A., Listing J., Sieper J. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis Rheum. 2006; 54: 569-78. 36. Schattenkirchner M., Milachowski K. A double-blind, multicentre, randomized clinical trial comparing the efficacy and tolerability of aceclofenac with diclofenac resinate in patients with acute low back pain. Clin Rheumatol. 2003; 22(2): 127-135. 37. Silverstein F., Faich G., Goldstein J. et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: a randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA 2000; 284:1247-55. 38. van Tulder M., Becker A., Bekkering T. et al. European guidelines for the management of acute nonspecific low back pain in primary care. Eur Spine J (2006) 15(Suppl. 2):S169-S191. 39. Villa Alcazar L., de Buergo M., Rico Lenza H., Montull Fruitos E. Aceclofenac is as safe and effective as tenoxicam in the treatment of ankylosing spondylitis: a 3 month multicenter comparative trial. Spanish Study Group on Aceclofenac in Ankylosing Spondylitis. J Rheumatol. 1996; 23(7):1194-1199. 40. Von Korff M., Saunders K. The course of back pain in primary care. Spine. 1996; 21: 2833-7283. 41. Wang G., Russell C., Wang S. State-dependent block of voltage-gated Na-channels by amitriptyline via the local anesthetic receptor and its implication for neuropathic pain. Pain 2004; 110:166-174. 42. Ward D., Veys E., Bowdler JM, Roma J. Comparison of aceclofenac with diclofenac in the treatment of osteoarthris. Clin Rheumatol 1995; 14: 656-62. 43. Yamazaki R., Kawai S., Matsuzaki T. et al. Aceclofenac blocks prostaglandin E2 production following its intracellular conversion into cyclooxygenase inhibitors. Eur J Pharmacol. 1997; 329(2-3): 181-187. 44. Zhao S., Burke T., Whelton A. et al. Comparison of the baseline cardiovascular risk profile among hypertensive patients prescribed COX-2-specific inhibitors or nonspecific NSAIDs: data from real life practice. Am J Manag Care. 2001; 8(15 Suppl): S392-400. Key words of the article: aceclofenac, patients, effectiveness, Application, acute
SOURCE RMJ JANUARY 26, 2010, VOLUME 18, NO. SPECIAL
Aceclofenac in the treatment of osteoarthritis
Osteoarthritis (OA) is a disease that develops as a result of the interaction of various mechanical and biological factors that disrupt the normally existing balance between the processes of degradation and synthesis of all matrix components, especially articular cartilage [1]. Currently, OA is considered an organ disease, since the pathological process involves not only cartilage, but also subchondral bone, synovium, menisci, ligaments and periarticular muscles.
The prevalence of this disease in the population correlates with age, reaching maximum values over the age of 65 years. Women get sick almost 2 times more often than men. The development of the disease leads to a deterioration in the quality of life of patients, limits their physical capabilities, and often social functions, and causes disability. According to the latest data from an epidemiological study in Russia, OA primarily affecting the knee and/or hip joints affects 13.0% of the population [2].
The leading clinical symptom of OA is pain, which is the immediate reason for the patient to see a doctor. Rheumatic diseases (RD) differ in pathogenesis and clinical picture, but have one common manifestation - pain. Taking into account the pathophysiological mechanisms, it is proposed to distinguish three main groups of pain: nociceptive, neuropathic and psychogenic. The most characteristic feature of OA is nociceptive pain, which occurs when peripheral pain receptors - “nociceptors” are irritated, localized in almost all organs and systems. Neuropathic pain occurs due to damage to various parts (peripheral and central) of the somatosensory nervous system and can also be observed in OA. Nociceptive pain syndromes are most often acute (burn, cut, bruise, abrasion, fracture, sprain), but in OA they are chronic. Joint tissues are abundantly supplied with nociceptors: synovial membrane, joint capsule, ligamentous apparatus, periarticular muscles, subchondral bone, which become sources of chronic pain in OA. One of the features of chronic pain syndromes is the reflex involvement of muscles, first at the segmental level of the lesion, then more diffusely, forming a muscular-tonic syndrome that occurs as a result of nociceptive impulses coming from the affected tissues. With prolonged nociceptive impulses, a tonically tense muscle itself becomes a source of pain and is potentially ready for the formation of myofascial pain syndrome. In addition to excitation by afferent stimuli, muscle nociceptors are activated by endogenous substances that are formed during prolonged tension and cause pain, such as bradykinin, serotonin and high concentrations of potassium ions. Bradykinin and serotonin also affect blood vessels and cause changes in the local state of vascularization. Prolonged muscle tension through the mechanisms of neurogenic inflammation contributes to the appearance of loci of painful muscle compactions, which further enhances the afferent flow of nociceptive impulses into the structures of the central nervous system and, as a consequence of this, a greater number of central nociceptive neurons are sensitized. This vicious circle plays an important role in the chronicity of pain [29]. Its intensity in OA can depend on many factors, and, as recent studies have shown, one of them is the increase in the mineral density of the subchondral tibia [3, 4].
The leading place in the treatment of OA is occupied by non-steroidal anti-inflammatory drugs (NSAIDs), which belong to the class of symptom-modifying drugs. In rheumatology, NSAIDs are considered as a necessary component of complex treatment, which is pathogenetically justified, since the constantly present inflammatory process is the cause of pain and progression of the disease. Possessing anti-inflammatory, analgesic and antipyretic properties, they are widely used to reduce pain, inflammation, stiffness and improve joint function, without affecting the outcome of the disease, but significantly improving the quality of life of patients. As data from a large number of clinical studies have shown, in rheumatic diseases (RD), NSAIDs are significantly more effective than high doses of paracetamol (4 g/day) and are not inferior to opioid analgesics (such as tramadol) [5, 6]. However, even short-term use of NSAIDs in a certain group of patients can lead to the development of serious adverse events.
The multidirectionality of the biological action of NSAIDs explains not only their anti-inflammatory effect, but also a certain range of class-specific complications that arise from their use. The most common side effects of NSAIDs are damage to the gastrointestinal tract (GIT), a negative effect on the circulatory system, and a decrease in platelet aggregation. Nephrotoxicity and hepatotoxicity are also potentially important complications.
The development of NSAID-induced gastropathy is determined primarily by the systemic effect of NSAIDs associated with the suppression of the activity of cyclooxygenase-1 (COX-1), which determines the synthesis of “cytoprotective” prostaglandins (PGs), which leads to a significant decrease in its protective potential and contributes to damage to the mucosa. Reduced platelet aggregation, deterioration of capillary blood flow in the mucosa, blockade of NO synthetase and enzyme systems of epithelial cell mitochondria, increased cellular apoptosis, impact on gastric secretion and disruption of repair processes are associated with blockade of COX-2 and are additional factors associated with systemic exposure to NSAIDs [8 ]. NSAID gastropathy occurs in chronological connection with the use of NSAIDs and is manifested by erosions and ulcers of the upper gastrointestinal tract, against which complications such as gastrointestinal bleeding and perforation are possible. The negative effects of these drugs can be observed in all parts of the gastrointestinal tract, from the oral cavity to the rectum. Liver damage associated with regular use of NSAIDs manifests itself as an asymptomatic increase in transaminases in 1–5% of patients. Clinically pronounced hepatotoxic reactions are much less common - about 1 case per 10,000 patients. Patients who regularly take NSAIDs and have possible risk factors for liver damage require regular monitoring of biochemical blood tests.
Cardiovascular side effects of NSAIDs are especially pronounced in the elderly and in patients suffering from concomitant diseases (coronary heart disease, diabetes mellitus), as well as rheumatic inflammatory diseases (primarily rheumatoid arthritis (RA)). NSAIDs are an independent risk factor for the development of arterial hypertension (AH). The results of randomized clinical trials and meta-analyses indicate that the use of non-selective (nNSAIDs) and selective NSAIDs (sNSAIDs) leads to an increase in blood pressure and is significant in patients with initial hypertension [9]. Particular attention has been drawn to potential cardiovascular complications while taking sNSAIDs, which is associated with the ability of these drugs to reduce COX-2-dependent synthesis of prostacyclin (PGl2) by vascular endothelial cells and the lack of effect on COX-1-dependent synthesis of thromboxane (TxA2) by platelets, which potentially may lead to an imbalance of PGl2/TxA2 and, consequently, to the activation of platelet aggregation and adhesion and an increased risk of thrombosis. It should be noted that NSAIDs, as a class, can increase the risk of developing cardiovascular complications, but this factor is significantly inferior in importance to others, such as smoking, dyslipidemia, and obesity [8, 27].
However, with proper prescribing of NSAIDs, the risk of adverse events can be reduced. When individually selecting NSAIDs, it is necessary to take into account the analgesic effect of the drug, the individual risk of developing adverse events from the gastrointestinal tract and the cardiovascular system. The risk of gastrointestinal complications is reduced with the use of proton pump inhibitors (PPIs), and the cardiovascular risk is reduced with the use of low doses of acetylsalicylic acid [10]. It must be remembered that the main risk factors are old age (over 65 years), a history of peptic ulcer disease, long-term use of high doses of NSAIDs and the simultaneous use of two or more different NSAIDs, as well as the combined use of NSAIDs and hormonal drugs. The latest international recommendations for the treatment of patients with OA state that NSAID therapy should be carried out in minimal effective doses and, if possible, not prescribed for a long time [7].
In Russia there is a wide range of NSAIDs and the question naturally arises about the rational choice of the drug. Undoubtedly, it should be based on an objective comparison of the advantages and disadvantages of various representatives of this group of drugs. It has been proven that in equivalent doses and with sufficient observation time, all NSAIDs (selective and non-selective) demonstrate the same effectiveness [28].
The main principle of action of NSAIDs is to suppress COX, an enzyme that metabolizes arachidonic acid into prostaglandins. Aceclofenac (Aertal) occupies a special place among NSAIDs, which has a multicomponent effect on inflammation. Aceclofenac inhibits both COX-1 (synthesis of physiological PGs) and COX-2 (synthesis of pro-inflammatory PGs), approaching selective NSAIDs, and therefore is safer in relation to the gastrointestinal tract. The drug inhibits the synthesis of the pro-inflammatory cytokine interleukin IL-1-beta, which suppresses the proliferation of chondrocytes and activates the degradation of cartilage. An important ability of aceclofenac is to suppress the synthesis of tumor necrosis factor alpha (TNF-alpha) and nitric oxide. In addition, the drug inhibits the expression of cell adhesion molecules (L-selectin), suppresses the adhesion of neutrophils to the endothelium, which provides a pronounced anti-inflammatory effect [14, 15]. Currently, special attention is paid to the effect of NSAIDs on the metabolism of cartilage tissue. Conventionally, NSAIDs can be divided into three groups: chondronegative, neutral with respect to cartilage tissue and chondroprotective. The issue of the negative impact of some drugs from this group on the progression of OA is widely discussed [11–13]. Thus, in vitro studies have shown that indomethacin and salicylates inhibit the synthesis of cartilage matrix components, promoting the progression of the disease, and indomethacin has a direct negative effect, reducing the content of proteoglycans in hyaline cartilage and increasing the loss of newly formed proteoglycans. At the same time, some NSAIDs increase the synthesis of matrix components and inhibit chondrocyte apoptosis. Aceclofenac experimentally demonstrated the ability to increase the synthesis of proteoglycans and hyaluronic acid in cultured cartilage cells of patients with OA, as well as reduce the production of metalloproteinases that cause destruction of bone and cartilage tissue [14, 15]. Blot L. et al., studying changes in the metabolism of proteoglycans and hyaluronan under the influence of aceclofenac, diclofenac and meloxicam in cartilage explants obtained from patients with moderate and severe gonarthrosis, showed that when treated with diclofenac, the metabolic balance between the content of proteoglycans and hyaluronic acid in the extracellular matrix hyaline cartilage remained unchanged. Aceclofenac and meloxicam, on the contrary, had a dose-dependent effect and increased the synthesis of proteoglycans and hyaluronic acid in moderate OA [15].
The clinical effectiveness of aceclofenac has been proven in 132 published clinical studies. The tolerability and effectiveness of this drug have been studied in comparative studies with various analgesics and NSAIDs. Thus, Battle-Gualda E. et al. in a double-blind, randomized, 6-week study in 168 patients with knee OA showed that aceclofenac at a dose of 200 mg/day was more effective in relieving pain with better tolerability compared to paracetamol 3 g/day [16]. In a longer study (observation period was 12 weeks) in patients with gonarthrosis, aceclofenac 200 mg/day was compared with naproxen 1 g/day. Both drugs had an equal analgesic effect, but aceclofenac had a significantly lower number of adverse events from the gastrointestinal tract [17]. The results of a meta-analysis of 13 randomized, double-blind studies in patients with RD showed that when taking aceclofenac for a long time (3–6 months), adverse reactions developed 1.38 times less often than when taking other NSAIDs [18]. The effectiveness of aceclofenac was assessed in randomized studies in other RDs: in RA, aceclofenac at a dose of 200 mg/day was comparable to diclofenac at a dose of 150 mg/day, ketoprofen at a dose of 150 mg/day, and piroxicam at a dose of 20 mg/day. It was also noted that positive dynamics developed faster in patients receiving aceclofenac. In patients with ankylosing spondylitis (AS), comparative studies of aceclofenac 200 mg/day, tenoxicam 20 mg/day, naproxen 1 g/day and indomethacin 100 mg/day showed similar results [19].
Patients with RD, as a rule, are forced to take NSAIDs for a long time, so good tolerability of the drug is very important. The results of a prospective, open, multicenter 12-month study SAMM (Safety Assessment of Marketed Medicines), which assessed the safety of aceclofenac and diclofenac in 10,142 patients suffering from RA, OA, and AS, confirmed the good tolerability of aceclofenac [20]. Aceclofenac at a dose of 200 mg/day was received by 7890 people and diclofenac 150 mg/day by 2252 patients. The researchers analyzed the frequency of adverse reactions: adverse events occurred in 22.4% of patients receiving aceclofenac, and in 27.1% of those receiving diclofenac. The most common of them were reactions from the gastrointestinal tract (dyspepsia, pain, diarrhea, nausea) - in 10.6% and 15.2% (p < 0.05), respectively. There were no severe adverse events from the hepatobiliary system. Thus, the use of aceclofenac was accompanied by a lower risk of developing NSAID gastropathy and better tolerability, while aceclofenac was not inferior to standard NSAIDs in effectiveness. The effectiveness of aceclofenac in acute and chronic pain of inflammatory origin and its good tolerability increased the degree of satisfaction of patients and attending physicians with the results of therapy, which is confirmed by a European cohort study conducted in Austria, Belgium, Germany, and Greece [21]. The study included 23,407 patients suffering from OA, RA, AS, pain in the cervical spine and lower back, and pain after injuries. Patients with OA made up the majority (80.2%). The evaluation criteria were satisfaction with the therapy of patients and attending physicians. Patients were transferred to taking aceclofenac due to the lack of effect of the previous NSAID - in 45.5% of patients, poor tolerability - in 35%, and in 19.5% - for a combination of these reasons. Aceclofenac was prescribed to patients at a dose of 200 mg/day, diclofenac at a dose of 150 mg 2 times a day (patient ratio was 3:1, respectively). The duration of therapy was 12 months. The high effectiveness of aceclofenac and overall satisfaction with therapy were confirmed by clinical assessment by 90% of patients and 84% of doctors. The authors also noted high adherence to treatment (94%).
One of the most important indicators for a drug that claims to be of choice in the treatment of chronic RD is safety. A large number of studies conducted in total on several thousand patients provided evidence of the safety of aceclofenac. Thus, taking the drug for 1 month was equivalent in safety to taking placebo; damage from the gastrointestinal tract was similar to damage caused by placebo. Endoscopic evaluation showed that aceclofenac causes less damage to the gastrointestinal mucosa compared to diclofenac. In patients taking aceclofenac, blood loss in feces was significantly less compared to diclofenac. Meta-analysis data confirmed the safety of aceclofenac. Comparative studies have noted high compliance of the drug compared with diclofenac and other NSAIDs [22–26].
In 2010–2011 In Russia, a multicenter open randomized comparative study of the effectiveness and safety of aceclofenac compared with diclofenac in patients with OA of the knee joints was conducted in 5 centers.
Purpose of the study: to evaluate the effectiveness, tolerability, and safety of aceclofenac compared to diclofenac in patients with gonarthrosis.
Materials and methods
Included were 200 outpatients (mean age 62.6 ± 7.1 years) with OA of the knee joints stage 2–3 according to Kelgren (100 patients in each group) with pain when walking > 40 mm according to VAS. The groups were comparable in terms of demographic and clinical parameters (Table 1). The first group took aceclofenac (Aertal) 200 mg/day, the second group took diclofenac 100 mg/day. The duration of the study was 3 months. The following were assessed: WOMAC index, “get up and go” test, EQ-5D questionnaire, general and biochemical blood tests.
Research results and discussion
A significant decrease in pain intensity and improvement in joint function, a decrease in the total WOMAC index was noted after a month of therapy in both groups of patients and persisted throughout the observation period (Table 2). A more rapid decrease in stiffness was observed in patients taking aceclofenac, when statistically significant indicators were obtained already at the second visit; by the end of treatment, a significant decrease in stiffness was noted in both groups of patients. Significant improvements in general health and EQ-5 D scores, as well as a decrease in time spent on the stand-up and walk test, were observed in both groups from the second visit.
After a month, “significant improvement” and “improvement” were more often observed while taking aceclofenac (86.3%) than with diclofenac (66%), after 3 months of therapy - in 95.8% and 76.2%, respectively (p <0.05). The therapy was well tolerated. Adverse events were observed significantly less often in the group of patients receiving aceclofenac (5%) compared with diclofenac (16%), especially from the gastrointestinal tract (Table 3).
Thus, based on the results obtained, we can conclude that aceclofenac is equally effective as diclofenac in terms of its effect on pain and the functional state of joints. A more rapid decrease in stiffness was noted when taking aceclofenac. Aceclofenac has higher safety compared to diclofenac: it causes significantly fewer adverse reactions from the gastrointestinal tract, and is also associated with a lower frequency of treatment interruptions due to other adverse events.
Literature
- Nasonova V. A. The problem of osteoarthritis at the beginning of the 21st century // Consilium medicum. 2000, 2, 6.
- Galushko E. A. Medical and social significance of rheumatic diseases. Author's abstract. dis. Dr. med. Sci. M., 2011.
- Bruyere O., Dardenne C., Lejeune E. et al. Subchondraltibial bone mineral density predicts future joint space narrowing at the medial femoro-tibial compartment in patients with knee osteoarthritis // Bone. 2003, v. 32(5), p. 541–545.
- Zaitseva E. M., Alekseeva L. I., Smirnov A. V. Causes of pain in osteoarthritis and factors of disease progression // Scientific and practical rheumatology. 2011, no. 1, 50–57.
- Boureau F., Schneid H. et al. The IPSO study: ibuprofen, paracetamol study in osteoarthritis. A randomized comparative clinical study comparing the efficacy and safety of ibuprofen and paracetamol analgesic treatment of osteoarthritis of knee or hip // Ann. Rheum. Dis. 2004, 63, 1028–1035.
- Zhang W., Jones A., Doherty M. Does paracetamol (acetaminophen) reduce pain of osteoarthritis? A meta-analysis of randomized controlled trials // Ann. Rheum. Dis. 2004, 63, 901–907.
- OARSI recommendations for the treatment of osteoarthritis of the knee and hip joints. Part III. 2010.
- Nasonov E. L., Karateev A. E. Use of non-steroidal anti-inflammatory drugs. Clinical recommendations // Russian Medical Journal. 2006, vol. 14, no. 25, 3–11.
- Sowers JR, White WB, Pitt B. et al. The effects of cyclooxygenase-2 inhibitors and nonsteroidal anti-inflammatory therapy on 24-hour blood pressure in patients with hypertension, osteoarthritis and type 2 diabetes mellitus // Arch. Intern. Med. 2005, vol. 165, no. 2, p. 161–168.
- Karateev A. E., Yakhno N. N., Lazebnik L. B. et al. The use of non-steroidal anti-inflammatory drugs. Clinical recommendations. M.: IMA-PRESS, 2009, 167 p.
- Ding S. Do NSDIDs affect the progression of osteoarthritis? //Inflammation. 2002; 26: 139–142.
- Dingle JT The effect of nonsteroidal anti-inflammatory drugs on human articular cartilage glycosaminoglycan synthesis // Osteoarthritis Cartilage. 1999; 7: 313–314.
- Mastbergen SC, Jansen NWD, Bijlsma JWJ et al. Differential direct effects of cyclo-oxygenase-1/2 inhibition on proteoglycan turnover of human osteoarthritis cartilage: an in vitro study // Arthritis Research and Therapy. 2006; 8: R2 doi: 1186/ar1846.
- Akimoto H., Yamazaki R. et al. A major metabolite ogaceclofenac 4-hydroxyaceclofenac suppresses the interleukin-1 induced production of promatrixmetalloprpteinases and release of sulfated-glycosaminoglycans from rabbit articular chondrocytes // Eur. J. Pharmacol. 2000, 401(3), 429–436.
- Blot L., Marcelis A., Devogelaer J.-P. et al. Effects of diclofenac, aceclofenac and meloxicam on the metabolism of proteoglycans and hyaluronan in osteoarthritic human cartilage // British J. Pharmacol. 2000, 131, 1413–1421.
- Battle-Gualda E., Rom n Ivona J., Mart n Mola E. et al. Aceclofenacvsparacetamol in the management of systematic osteoarthritis of the knee: a double blind 6 week randomized controlled trial // Osteoarthritis Cartilage. 2007; 15(8), 900–908.
- Korsanoff D., Frericck H., Bowdler J. et al. Aceclofenac is a well-tolerated alternative to naproxen in the treatment of osteoarthritis // Clin. Rheumatol. Inflamm. 1997, 16: 32–38.
- Peris F., Bird H., Semi U. et al. Treatment compliance and safety of aceclofenac versus standard NSAIDs in patients with common arthritic disorders: a meta-analysis // Eur. J. Rheumatol. Inflamm. 1996, 16, 37–45.
- Wsijon-Bahos J., Bernstein R. Efficacy of aceclofenac: indications and analgesicporency // Eur. J. Rheumatol. Inflamm. 1996, 16, 9–12.
- Huskisson E., Irani M., Murray F. A large prospective open-label, multicentre SAMM study, comparing the safety of aceclofenac with diclofenac in patients with rheumatic disease // Europ. J. Rheumatol. Inflamm. 2007, 7 (1), 1–7.
- Lemmel E., Leeb B., De Bast J. Patients and physician satisfaction with aceclofenac: results of the European Observational Cohort Study Aceclofenac is the treatment of choice for patients and physicians in the management of inflammatory pain // Curr. Med. Res. Opin. 2002, 18(3), 146–153.
- ZabalaGamarra M. Efficacy and tolerability of aceclofenac in a 3-month open trial in the treatment of gonarthrosis // Dolor Inflamation. 1993; 1:3–7.
- Diaz C., Rodriguez A., Geli C. et al. Efficacy and tolerance of aceclofenac versus diclofenac in the treatment of knee osteoarthritis. A multicenter study // Eur J Rheumatol. Inflamm. 1996, 16: 17–22.
- Calin A., Murray FE Aceclofenac: side effects and safety // Eur J Rheumatol. Inflamm. 1996, 16: 13–16.
- Korsanoff D., Frerick H., Bowdler J. et al. Aceclofenac is a well-tolerated alternative to naproxen in the treatment of osteoarthritis // Clin Rheumatol. 1997; 16:32–38.
- PereBusquer M., Calero E., Rodriguez M. et al. Comparison of aceclofenac with piroxicam in the treatment of osteoarthritis // Clin Rheumatol. 1997; 16: 154–159.
- Ray W. A. et. al. // Circ. Cardiovasc. Qual. Outcomes. 2009, v. 2, p. 155.
- Karateev A.E. Celecoxib, etoricoxib, meloxicam and nimesulide: advantages and disadvantages // Effective pharmacotherapy. 2011, No. 1, p. 28–36.
- Alekseev V.V. Modern concepts and basic principles of pain therapy // RMJ, 2011, vol. 19, special. issue, p. 6–11.
E. P. Sharapova*, Candidate of Medical Sciences E. A. Taskina* T. A. Raskina**, Doctor of Medical Sciences I. B. Vinogradova***, Candidate of Medical Sciences, Associate Professor O. N. Ivanova**** , Candidate of Medical Sciences L. V. Menshikova*****, Doctor of Medical Sciences, Professor L. I. Alekseeva*, Doctor of Medical Sciences, Professor
*FGBU Research Institute of Rheumatology of the Russian Academy of Medical Sciences , Moscow **GBOU VPO Kemerovo State Medical Academy Ministry of Health and Social Development of Russia, Kemerovo ***GUZ OKB, Ulyanovsk ****GUZ OKB No. 1, Voronezh *****GBOU DPO IGMAPO Ministry of Health and Social Development of Russia, Irkutsk
Contact information for authors for correspondence
Instructions for use
Adverse events can be minimized by reducing the duration of treatment required to control symptoms (see Precautions section).
Aceclofenac - MIC is intended for oral administration; The capsule should be swallowed with at least half a glass of water. Aceclofenac-MIC can be taken with meals.
Adults:
The maximum recommended dose is 200 mg per day, given in two separate 100 mg doses (one capsule in the morning and one in the evening).
Children:
There is no data on the effectiveness and safety of taking the drug in children.
Elderly:
There is usually no need to reduce the dose; however, the precautions listed in the Precautions section must be followed.
Liver failure:
The dose of aceclofenac should be reduced in patients with mild or moderate liver disease. The recommended starting dose is 100 mg per day (see Precautions section).
Kidney failure:
There is no data on the need to reduce the dose of aceclofenac in patients with mild renal impairment, but caution should be exercised when using Aceclofenac-MIC (see section "Precautions").
Pregnancy and breastfeeding period
Pregnancy
There is no data on the use of aceclofenac during pregnancy.
Inhibition of prostaglandin synthesis may adversely affect the course of pregnancy and/or embryonic/fetal development.
Data from epidemiological studies indicate an increased risk of miscarriage, heart disease and gastroschisis after the use of prostaglandin synthesis inhibitors in the early stages of pregnancy. The absolute risk of developing heart disease increases from less than 1% to approximately 1.5%. The risk increases with increasing dose and duration of treatment.
In animals, administration of prostaglandin synthesis inhibitors results in pre- and postimplantation fetal death and embryonic and fetal mortality. In addition, the incidence of various defects, including cardiac disease, is increased in animals receiving prostaglandin synthesis inhibitors during organogenesis.
During the first and second trimester of pregnancy, drugs containing aceclofenac are not prescribed unless absolutely necessary. If aceclofenac is taken by a woman planning a pregnancy or in the first or second trimester of pregnancy, the dose should be as low as possible and the duration of treatment should be as short as possible.
During the third trimester of pregnancy, all prostaglandin synthesis inhibitors:
● can affect the fetus, having cardiopulmonary toxicity (with premature closure of the ductus arteriosus and pulmonary hypertension);
● may affect the fetus by causing renal dysfunction, which can lead to renal failure and oligohydramnios.
Mothers and newborns at the end of pregnancy:
● the drug may affect the duration of bleeding due to the antiplatelet effect, which can develop even after using very low doses;
● the drug may inhibit uterine contractions, leading to delayed labor or prolonged labor.
Therefore, the use of aceclofenac is contraindicated in the third trimester of pregnancy (see sections "Contraindications" and "Precautions").
Lactation: There is no information about the penetration of aceclofenac into breast milk. However, there was no significant penetration of the labeled radioisotope (C14) of aceclofenac into the milk of lactating rats. The decision to continue/stop breastfeeding or use aceclofenac is made after assessing the benefits of breastfeeding for the child and the benefits of taking aceclofenac for the mother.
The use of aceclofenac should be avoided during pregnancy and lactation, unless the potential benefit to the mother outweighs the possible risks to the fetus.
Fertility:
The use of aceclofenac, like other cyclooxygenase/prostaglandin synthesis inhibitors, may reduce fertility and is not recommended for women planning children. Women having difficulty conceiving or undergoing fertility research should stop taking aceclofenac.
Impact on the ability to drive a car, work with equipment
Patients who have experienced symptoms such as weakness, dizziness, vertigo, nausea or other symptoms of the central nervous system should not drive vehicles or operate other dangerous machinery while taking NSAIDs.
Interaction with other drugs
No drug interaction studies have been conducted with the exception of warfarin.
Aceclofenac is metabolized by cytochrome P450 2C9, and in vitro data indicate that aceclofenac may be an inhibitor of this enzyme. Thus, the risk of pharmacokinetic interaction is possible when taken concomitantly with phenytoin, cimetidine, tolbutamide, phenylbutazone, amiodarone, miconazole and sulfaphenazole. As with other NSAID drugs, the risk of pharmacokinetic interactions with other drugs that are eliminated from the body by active renal secretion, such as metorexate and lithium preparations, also increases. Aceclofenac is almost completely bound to plasma albumin and, therefore, there is the possibility of displacement interactions with other protein-bound drugs.
Due to the lack of pharmacokinetic interaction studies of aceclofenac, the following information is based on data from other NSAIDs:
Concomitant use should be avoided:
Methotrexate: NSAIDs inhibit tubular secretion of methotrexate; Moreover, a slight metabolic interaction may occur, resulting in decreased methotrexate clearance. Therefore, when using high doses of methotrexate, NSAIDs should be avoided.
Lithium and digoxin: Some NSAIDs inhibit the renal clearance of lithium and digoxin, resulting in increased serum concentrations of both substances. Coadministration should be avoided unless lithium and digoxin concentrations are monitored frequently.
Anticoagulants: NSAIDs inhibit platelet aggregation and damage the gastrointestinal mucosa, which may enhance the effects of anticoagulants and increase the risk of gastrointestinal bleeding in patients taking anticoagulants. The combined use of aceclofenac and oral coumarin anticoagulants, ticlopidine and thrombolytics should be avoided unless the patient is closely monitored.
Antiplatelet agents and selective serotonin reuptake inhibitors (SSRIs) when used together with NSAIDs may increase the risk of gastrointestinal bleeding (see Precautions section).
The following combinations require dose adjustment and use with caution:
Methotrexate: The possible interaction of NSAIDs and methotrexate should be kept in mind, even at low doses of methotrexate, especially in patients with impaired renal function. During concomitant use, renal function should be monitored. Caution should be exercised if both NSAIDs and methotrexate are taken within 24 hours, as the concentration of methotrexate may increase, increasing the toxicity of this drug.
Cyclosporine, tacrolimus: When taking NSAIDs concomitantly with cyclosporine or tacrolimus, the risk of increased nephrotoxicity due to decreased formation of renal prostacyclin should be taken into account. Therefore, renal function should be carefully monitored during concomitant use.
Other NSAIDs: Concomitant use of acetylsalicylic acid or other NSAIDs may increase the incidence of side effects, so caution should be exercised.
Corticosteroids: The risk of ulcers or bleeding from the gastrointestinal tract increases (see section "Precautions").
Diuretics: aceclofenac, like other NSAIDs, can inhibit the activity of diuretics and can reduce the diuretic effect of furosemide and bumetanide and the antihypertensive effect of thiazides. Concomitant use with potassium-sparing diuretics may lead to an increase in potassium levels; therefore, it is necessary to regularly monitor serum potassium levels.
Aceclofenac did not affect blood pressure control when used in combination with bendrofluazide, although interaction with other diuretics cannot be excluded.
Antihypertensive drugs: NSAIDs may also reduce the effect of antihypertensive drugs. Concomitant use of ACE inhibitors or angiotensin II receptor antagonists and NSAIDs may lead to impaired renal function. The risk of acute renal failure, which is usually reversible, may be increased in some patients with impaired renal function, such as elderly or dehydrated patients. Therefore, when used together with NSAIDs, caution should be exercised, especially in elderly patients. Patients should consume the required amount of fluid and be under appropriate monitoring (monitoring of renal function at the beginning of co-administration and periodically during treatment).
Hypoglycemic agents: Clinical studies show that diclofenac can be used in conjunction with oral hypoglycemic agents without affecting their clinical effect. However, there are isolated reports of hypoglycemic and hyperglycemic effects of the drug. Thus, when taking aceclofenac, dosages of drugs that can cause hypoglycemia should be adjusted.
Zidovudine: The risk of hematological toxicity increases when NSAIDs are taken concomitantly with zidovudine. There is evidence of an increased risk of hemarthrosis and hematomas in HIV (+) patients with hemophilia receiving zidovudine and ibuprofen.
Side effect
Gastrointestinal disorders:
Most commonly observed side effects are gastrointestinal disorders. Stomach ulcers, perforation or bleeding from the gastrointestinal tract may occur, sometimes leading to death, especially in elderly patients (see section "Precautions"). Nausea, vomiting, diarrhea, bloating, constipation, dyspepsia, stomach pain, melena, hematemesis, ulcerative stomatitis, exacerbation of colitis and Crohn's disease have been observed when taking NSAIDs (see Precautions). Gastritis is less common.
Edema, hypertension and heart failure have been reported in association with NSAID use.
Clinical studies and epidemiological data indicate that some NSAIDs (especially at high doses and long-term use) may slightly increase the risk of arterial thrombotic events (eg, myocardial infarction or stroke) (see Precautions section).
The following table summarizes the adverse events reported from clinical studies and post-marketing surveillance; Adverse events are grouped according to organ system classes and frequency of occurrence. Very common (≥1/10), common (≥1/100 to <1/10), uncommon (≥1/1,000 to <1/100), rare (≥1/10,000 to >1/1000) 1,000), very rare (< 1/10,000).
| Organ system class according to MedDRA (Medical Dictionary Activities, Medical Dictionary of Regulatory Activities) | Frequent (from ≥1/100 to <1/10) | Infrequent (from ≥1/1,000 to <1/100) | Rare (from ≥1/10,000 to <1/1,000) | Very rare (<1/10 000) |
| Blood and lymphatic system disorders | Anemia | Bone marrow suppression, granulocytopenia, thrombocytopenia, hemolytic anemia, neutropenia | ||
| Immune system disorders | Anaphylactic reactions (including shock), hypersensitivity | |||
| Nutritional and metabolic disorders | Hyperkalemia | |||
| Mental disorders | Depression, unusual dreams, insomnia | |||
| Nervous system disorders | Dizziness | Paresthesia, tremor, drowsiness, headache, dysgeusia (taste perversion) | ||
| Visual disorders | Visual impairment | |||
| Disorders of the hearing organ and labyrinth | Vertigo, tinnitus | |||
| Heart disorders | Heart failure | Feeling of heartbeat | ||
| Vascular disorders | AH, worsening AH | Skin hyperemia, hot flashes, vasculitis | ||
| Respiratory, thoracic and mediastinal disorders | Dyspnea | Bronchospasm | ||
| Gastrointestinal disorders | Dyspepsia, abdominal pain, nausea, diarrhea | Bloating, gastritis, constipation, vomiting, ulceration of the oral mucosa | Melena, ulceration of the gastrointestinal mucosa, hemorrhagic diarrhea, hemorrhages in the gastrointestinal tract | Stomatitis, bloody vomiting, intestinal perforation, worsening of Crohn's disease and ulcerative colitis, pancreatitis |
| Disorders of the liver and biliary tract | Increased activity of liver enzymes | Liver damage (including hepatitis), increased alkaline phosphatase activity in the blood | ||
| Skin and subcutaneous tissue disorders | Itching, rash, dermatitis, urticaria | Angioedema | Purpura, eczema, severe reactions of the skin and mucous membranes (bullous reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis). In special cases, serious skin and soft tissue infections have been observed when NSAIDs were taken during chickenpox illnesses. | |
| Renal and urinary tract disorders | Increased concentrations of urea and creatinine in the blood | Nephrotic syndrome, renal failure, interstitial nephritis | ||
| General and administration site disorders | Swelling, fatigue, muscle cramps (legs) | |||
| Influence on the results of laboratory and instrumental studies | Weight gain |
Overdose
There is no data on an overdose of aceclofenac in humans.
Symptoms include headache, nausea, vomiting, epigastric pain, gastrointestinal irritation, gastrointestinal bleeding, rarely diarrhea, confusion, agitation, coma, drowsiness, dizziness, tinnitus, hypotension, respiratory depression, syncope, rarely seizures . In case of severe poisoning, acute renal failure and liver damage are possible.
Treatment of poisoning:
If necessary, symptomatic therapy should be carried out. Activated charcoal should be taken within one hour after taking a toxic amount of the drug. As an alternative, gastric lavage may be considered in adult patients in the first hour after taking a potentially life-threatening dose.
Specific interventions, such as hemodialysis or hemoperfusion, are likely to be ineffective in eliminating NSAIDs due to their high degree of protein binding and extensive metabolism. Good diuresis should be ensured, and renal and liver function should be carefully monitored. The patient should be observed for at least 4 hours after taking a potentially toxic dose. If frequent or prolonged seizures develop, intravenous diazepam should be used. Other measures may be necessary depending on the patient's clinical condition. Treatment of acute NSAID poisoning mainly consists of supportive and symptomatic therapy.
»
Aceclofenac welpharm 100 mg 20 pcs. film-coated tablets
History of liver, kidney and gastrointestinal tract diseases, bronchial asthma, arterial hypertension, decreased circulating blood volume (including after surgery), coronary heart disease, mild to moderate chronic renal failure (CC from 30 to 60 ml/min), mild to moderate liver failure, chronic heart failure, cerebrovascular diseases, dyslipidemia/hyperlipidemia. diabetes mellitus, peripheral arterial disease, smoking, old age, history of long-term use of NSAIDs, presence of Helicobacter pylori infection, frequent alcohol consumption, concomitant therapy with the following drugs:
- anticoagulants (eg warfarin);
antiplatelet agents (for example, acetylsalicylic acid, clopidogrel);
Application of Aceclofenac welpharm 100 mg 20 pcs. film-coated tablets during pregnancy and breastfeeding
The use of the drug during pregnancy and breastfeeding is contraindicated.
special instructions
The severity of adverse reactions can be adjusted by reducing the effective single dose required to control symptoms.
Patients with a history of arterial hypertension and/or chronic heart failure of NYMA functional class I-II require proper monitoring and consultation with a physician, because Fluid retention and edema have been reported during treatment with NSAIDs. Data from clinical and epidemiological studies suggest that the use of some NSAIDs (especially in high doses and long-term use) may increase the risk of arterial thrombosis (eg, myocardial infarction or stroke). There is insufficient data to exclude such a risk for aceclofenac.
Patients with uncontrolled arterial hypertension, congestive heart failure, coronary artery disease, peripheral arterial pathology and/or cerebrovascular disease should take aceclofenac only after a thorough analysis of the clinical situation. The same caution should be taken before initiating long-term treatment in patients at risk of cardiovascular disease (eg, hypertension, hyperlipidemia, diabetes mellitus, and smokers).
Aceclofenac should be taken with caution and under close medical supervision in patients with diseases of the gastrointestinal tract, a history of peptic ulcers, after acute cerebrovascular accident, systemic lupus erythematosus, porphyria, disorders of the hematopoietic system and bleeding disorders.
Aceclofenac may cause reversible inhibition of platelet aggregation.
The drug is not recommended for patients with Crohn's disease or ulcerative colitis. Caution should be exercised in patients with liver, kidney, or heart failure, as well as in patients with other diseases predisposed to the development of edema. Taking NSAIDs in this category of patients can lead to worsening renal excretion and the occurrence of edema.
Patients taking diuretics, or with an increased risk of hypovolemia, also need to exercise caution when taking Aceclofenac Welfarm.
Caution should be exercised in elderly patients, because... they are more likely to experience side effects. Gastrointestinal bleeding and/or perforation may occur during treatment, especially if there is a history of gastrointestinal diseases. In addition, older patients are more likely to have problems with the liver, kidneys, and cardiovascular system.
All patients receiving long-term treatment with NSAIDs require monitoring to reduce the risk of adverse reactions (for example, urinalysis, general and biochemical blood tests).
Concomitant use of Aceclofenac Velpharm with any drug that inhibits cyclooxygenase/prostaglandin synthesis may reduce fertility and is not recommended for women planning pregnancy.
Women with a history of infertility should stop taking Aceclofenac Velpharm.
Impact on the ability to drive vehicles and operate machinery
During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Overdose
Symptoms: dizziness, headache, hyperventilation with increased convulsive readiness, nausea, vomiting, abdominal pain.
Treatment: gastric lavage, administration of activated carbon, symptomatic therapy. There is no specific antidote. Forced diuresis, hemodialysis, and blood transfusion are ineffective.
Side effects Aceclofenac velpharm 100 mg 20 pcs. film-coated tablets
The most frequently identified adverse reactions in clinical studies were from the gastrointestinal tract (dyspepsia - 7.5%; abdominal pain - 6.2%; nausea - 1.5%; diarrhea - 1.5%); sometimes - dizziness. Itching, rash, and changes in the activity of liver enzymes and blood creatinine concentrations were also noted.
The undesirable effects listed below are presented by organ system class according to the MedDRA classification with the following frequency: often: ≥1/100 to
Allergic reactions: skin rash, urticaria, eczema, erythroderma, systemic anaphylactoid reactions, bronchial asthma, in some cases - vasculitis, pneumonitis, polymorphic exudative erythema (including Stevens-Johnson syndrome), toxic epidermal necrolysis (Lyell's syndrome).
From the immune system: rarely - anaphylactic reaction (including shock), hypersensitivity.
From the gastrointestinal tract: often - dyspepsia, abdominal pain, nausea, diarrhea; uncommon - flatulence, gastritis, constipation, vomiting, ulceration of the oral mucosa; rarely - melena, ulceration of the gastrointestinal tract, diarrhea with blood, gastrointestinal bleeding; very rarely - stomatitis, vomiting blood, gastric ulcer, perforation of the small intestine, worsening of Crohn's disease and ulcerative colitis, pancreatitis.
From the cardiovascular system: rarely - heart failure, increased blood pressure; very rarely - tachycardia, hot flashes, vasculitis.
From the liver and biliary tract: often - increased activity of liver enzymes; very rarely - liver damage (including hepatitis), increased blood alkaline phosphatase activity.
From the nervous system: often - dizziness; very rarely - paresthesia, tremor, drowsiness, headache, fatigue, dysgeusia.
Mental disorders: very rarely - depression, atypical dreams, insomnia.
From the skin and subcutaneous tissue: infrequently - itching, rash, dermatitis, urticarial rash; rarely - angioedema; very rarely - purpura, reactions from the skin and mucous membranes, bullous skin reactions.
From the hematopoietic organs: thrombocytopenia, leukopenia, agranulocytosis, hemolytic anemia, aplastic anemia.
From the blood and lymphatic system: rarely - anemia; very rarely - bone marrow suppression, granulocytopenia, neutropenia, hemolytic anemia.
From the kidneys and urinary tract: infrequently - increased blood urea concentration, increased blood creatinine concentration; very rarely - interstitial nephritis, nephrotic syndrome, renal failure.
From the respiratory system, chest and mediastinal organs: rarely - shortness of breath; very rarely - bronchospasm.
From the organ of vision: rarely - visual impairment.
From the organ of hearing and labyrinth: very rarely - vertigo, ringing in the ears.
Metabolism and nutrition: very rarely - hyperkalemia, weight gain.
Systemic disorders: very rarely - muscle spasms of the lower extremities.
Drug interactions
No drug interaction studies have been conducted with the exception of warfarin.
Aceclofenac is metabolized by the cytochrome P450-CYP2C9 system, and in vitro data indicate that aceclofenac may be an inhibitor of this enzyme. Therefore, there is a possible risk of pharmacokinetic interaction with phenytoin, cimetidine, tolbutamide, phenylbutazone, amiodarone, miconazole and sulfaphenazole.
As with other NSAIDs, there is a risk of pharmacokinetic interaction with drugs that are metabolized in the liver, such as methotrexate and lithium preparations.
Aceclofenac is almost completely bound to plasma proteins, and, therefore, it is necessary to consider the possibility of substitution with other drugs that are highly bound to plasma proteins.
Due to the lack of pharmacokinetic interaction studies, the following information is based on information obtained with other NSAIDs:
The following combinations should be avoided
NSAIDs inhibit tubular secretion of methotrexate, and a metabolic interaction may also occur leading to decreased clearance of methotrexate. Therefore, during treatment with large doses of methotrexate (more than 20 mg/week), NSAIDs should always be avoided.
Some NSAIDs inhibit the renal excretion of lithium, resulting in increased serum lithium concentrations. This combination should be avoided unless frequent monitoring of serum lithium concentrations is possible.
NSAIDs inhibit platelet aggregation and damage the gastrointestinal mucosa, which may increase the activity of anticoagulants and increase the risk of gastrointestinal bleeding in patients taking anticoagulants.
The combination of aceclofenac with oral anticoagulants of the coumarin group, ticlopidine, thrombolytics and heparin should be avoided unless carefully monitored.
The following combinations may require dose adjustment and precautions:
The possible interaction of NSAIDs and methotrexate must be taken into account, especially in patients with renal failure. When taking both drugs, monitoring of kidney function is necessary.
Precautions should be taken when taking NSAIDs and methotrexate simultaneously within 24 hours, because methotrexate concentrations may increase, resulting in increased methotrexate toxicity. It is believed that taking NSAIDs with cyclosporine or tacrolimus increases the risk of nephrotoxicity due to decreased renal prostacyclin synthesis. Therefore, when taking drugs simultaneously, it is important to monitor renal function.
Concomitant use of acetylsalicylic acid and other NSAIDs may increase the incidence of adverse reactions and, therefore, caution is required when taking them together.
NSAIDs may reduce the diuretic effect of furosemide, bumetanide and the hypotensive effect of thiazide diuretics. Simultaneous treatment with potassium-sparing diuretics may be associated with an increase in the concentration of potassium in the blood serum, therefore monitoring the potassium level in the blood is necessary.
NSAIDs may also reduce the effect of some antihypertensive medications.
Angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists in combination with NSAIDs can lead to renal failure. The risk of developing acute renal failure, which is usually reversible, may be increased in some patients with impaired nocturnal function, such as elderly patients or patients who are fluid-depleted. Therefore, the combination of such drugs with NSAIDs should be used with caution, patients should receive sufficient fluids with food, and renal function should be monitored.
There was no effect of aceclofenac on blood pressure when it was taken concomitantly with bendroflumethiazide, although interaction with other antihypertensive drugs such as beta-blockers cannot be ruled out.
Other possible interactions
Isolated cases of hypoglycemia and hyperglycemia have been reported. Therefore, for aceclofenac it is necessary to adjust the dose of drugs that cause hypoglycemia.
When used simultaneously with the drug Aceclofenac Velpharm:
- digoxin, phenytoin or lithium preparations - the plasma concentration of these drugs may increase;
- diuretics and antihypertensive drugs - the effect of these drugs may be weakened;
- potassium-sparing diuretics - can lead to the development of hyperglycemia and hyperkalemia;
- other NSAIDs or glucocorticosteroids - increases the risk of side effects from the gastrointestinal tract;
- selective serotonin reuptake inhibitors (citalopram, fluoxetine, paroxetine, sertraline) - increases the risk of gastrointestinal bleeding;
- cyclosporine - the toxic effect of the latter on the kidneys may increase;
- hypoglycemic agents - can cause both hypo- and hyperglycemia. With this combination of drugs, blood sugar control is necessary;
- acetylsalicylic acid - the concentration of aceclofenac in the blood decreases;
- antiplatelet agents and anticoagulants - the risk of bleeding increases (regular monitoring of blood clotting indicators is necessary);
- zidovudine - increases the risk of hematological toxicity.
Aceclofenac-MIK capsules 100 mg No. 10x6
Name
Aceclofenac-MIK caps. 100 mg in container pack No. 10x6
Description
Hard gelatin capsules of cylindrical shape with hemispherical ends with a white body and a red cap.
Main active ingredient
Aceclofenac
Release form
capsules
Dosage
100 mg
Indications for use
For osteoarthritis, rheumatoid arthritis and ankylosing spondylitis and other diseases of the musculoskeletal system accompanied by pain (for example, glenohumeral periarthritis and other extra-articular manifestations of rheumatism). To relieve pain (such as lumbar pain, toothache and primary dysmenorrhea).
Directions for use and doses
Adverse events can be minimized by reducing the duration of treatment required to control symptoms (see section "Precautions") Aceclofenac-MIC is intended for oral administration; The capsule should be swallowed with at least half a glass of water. Aceclofenac-MIC can be taken with meals. Adults: The maximum recommended dose is 200 mg per day, given in two separate 100 mg doses (one capsule in the morning and one in the evening). Children: There is no data on the effectiveness and safety of taking the drug in children. Elderly: There is usually no need to reduce the dose; however, the precautions listed in the Precautions section must be observed. Liver impairment: The dose of aceclofenac should be reduced in patients with mild or moderate liver disease. The recommended starting dose is 100 mg per day (see Precautions section). Renal failure: There is no data on the need to reduce the dose of aceclofenac in patients with mild renal impairment, but caution should be exercised when using Aceclofenac-MIC (see section "Precautions").
Use during pregnancy and lactation
Pregnancy There is no data on the use of aceclofenac during pregnancy. Inhibition of prostaglandin synthesis may adversely affect the course of pregnancy and/or embryonic/fetal development. Data from epidemiological studies indicate an increased risk of miscarriage, heart disease and gastroschisis after the use of prostaglandin synthesis inhibitors in the early stages of pregnancy. The absolute risk of developing heart disease increases from less than 1% to approximately 1.5%. The risk increases with increasing dose and duration of treatment. In animals, administration of prostaglandin synthesis inhibitors results in pre- and postimplantation fetal death and embryonic and fetal mortality. In addition, the incidence of various defects, including cardiac disease, is increased in animals receiving prostaglandin synthesis inhibitors during organogenesis. During the first and second trimester of pregnancy, drugs containing aceclofenac are not prescribed unless absolutely necessary. If aceclofenac is taken by a woman planning a pregnancy or in the first or second trimester of pregnancy, the dose should be as low as possible and the duration of treatment as short as possible. During the third trimester of pregnancy, all prostaglandin synthesis inhibitors: may affect the fetus, causing cardiopulmonary toxicity (with premature closure of the ductus arteriosus and pulmonary hypertension); may affect the fetus by causing kidney dysfunction, which can lead to kidney failure and oligohydramnios. Mothers and newborns at the end of pregnancy: the drug may affect the duration of bleeding due to the antiplatelet effect, which can develop even after the use of very low doses; the drug may inhibit uterine contractions, leading to delayed labor or prolonged labor. Therefore, the use of aceclofenac is contraindicated in the third trimester of pregnancy (see sections "Contraindications" and "Precautions"). Lactation: There is no information about the penetration of aceclofenac into breast milk. However, there was no significant penetration of the labeled radioisotope (C14) of aceclofenac into the milk of lactating rats. The decision to continue/stop breastfeeding or use aceclofenac is made after assessing the benefits of breastfeeding for the child and the benefits of taking aceclofenac for the mother. The use of aceclofenac should be avoided during pregnancy and lactation, unless the potential benefit to the mother outweighs the possible risks to the fetus. Fertility: The use of aceclofenac, like other cyclooxygenase/prostaglandin synthesis inhibitors, may reduce fertility and is not recommended for women planning children. Women having difficulty conceiving or undergoing fertility research should stop taking aceclofenac.
Precautionary measures
The simultaneous use of Aceclofenac-MIC and other NSAIDs, including selective cyclooxygenase-2 inhibitors, should be avoided. Adverse events can be minimized by using the lowest effective dose and reducing the duration of treatment necessary to control symptoms (see Dosage and Administration section and description of gastrointestinal and cardiovascular risks below). Effect on the gastrointestinal tract Bleeding, ulceration or perforation of the gastrointestinal tract with a fatal outcome was observed when taking any NSAIDs during any period of treatment, both with and without dangerous symptoms, both with and without a history of serious pathological conditions of the gastrointestinal tract . The risk of bleeding, ulceration and gastrointestinal perforation increases with increasing dose of NSAIDs in patients who have had an ulcer, especially if it was accompanied by hemorrhage or perforation (see section "Contraindications"), and in elderly patients. These patients should take the minimum effective dose of the drug. They require combination therapy with protective drugs (for example, misoprostol, or proton pump inhibitors), and similar therapy is also necessary for patients who take small doses of aspirin or other drugs that negatively affect the gastrointestinal tract (see section “Interactions”) "). Patients with gastrointestinal diseases, including the elderly, should report any unusual gastrointestinal symptoms (especially bleeding), including when initially taking the drug. Particular caution should be exercised in patients concomitantly taking drugs that may increase the risk of bleeding or ulceration, such as systemic corticosteroids, anticoagulants (such as warfarin), selective serotonin reuptake inhibitors, or antiplatelet agents (such as acetylsalicylic acid) (see Interactions section "). If bleeding from a gastrointestinal ulcer occurs in patients taking Aceclofenac-MIC, treatment should be discontinued. Effect on the cardiovascular system For patients with arterial hypertension and/or mild to moderate congestive heart failure, appropriate monitoring and special instructions are required, as fluid retention and edema associated with NSAIDs have been reported. Clinical studies and epidemiological data indicate that the use of some NSAIDs (particularly at high doses and during long-term use) may not significantly increase the risk of arterial thrombotic events (eg, myocardial infarction or stroke). There is no reliable data on the absence of this risk when taking aceclofenac. Patients with uncontrolled hypertension, heart failure (NYHA functional class I), congestive heart failure, cardiovascular risk factors (eg, hypertension, hyperlipidemia, diabetes mellitus and smoking), and a history of cerebral hemorrhage , special care should be taken when taking aceclofenac. Aceclofenac should be taken with caution and under the supervision of a physician in patients with the following conditions, as there is a threat of exacerbation of the disease (see section “Side Effects”): symptoms indicating the presence of a disease of the gastrointestinal tract, including its upper and lower sections, a history of ulcers, bleeding or perforation of the gastrointestinal tract; ulcerative colitis, Crohn's disease, bleeding tendency, SLE (systemic lupus erythematosus), porphyria, and disorders of hematopoiesis and hemostasis. Aceclofenac should be used with caution and under medical supervision in patients with a history of hemorrhagic stroke. Effect on the liver and kidneys Taking NSAIDs can cause a dose-dependent reduction in prostaglandin formation and sudden renal failure. The importance of prostaglandin in maintaining renal blood flow should be considered when taking the drug in patients with impaired cardiac, renal or hepatic function, in those receiving diuretics or in patients after surgery, as well as in elderly patients. Caution should be exercised when taking the drug in patients with mild or moderate hepatic and renal dysfunction, as well as in patients with other conditions that predispose to fluid retention in the body. In these patients, the use of NSAIDs may lead to impaired renal function and fluid retention. Caution should also be exercised when taking aceclofenac in patients taking diuretics or in individuals at increased risk of hypovolemia. A minimum effective dose and regular medical monitoring of renal function are required. Renal effects usually resolve after discontinuation of aceclofenac. Aceclofenac should be discontinued if changes in liver function tests persist or worsen, clinical signs or symptoms of liver disease develop, or other manifestations (eosinophilia, rash) occur. Hepatitis can develop without prodromal symptoms. The use of NSAIDs in patients with hepatic porphyria may precipitate an attack. Hypersensitivity and skin reactions Like other NSAIDs, the drug may cause allergic reactions, including anaphylactic/anaphylactoid reactions, even if the drug is taken for the first time. Severe skin reactions (some of which can be fatal), including exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis, have been very rare after taking NSAIDs (see section "Side effects"). The highest risk of these reactions occurring in patients is observed at the beginning of taking the drug, and the development of these adverse reactions is observed during the first month of taking the drug. If skin rash, lesions on the oral mucosa, or other signs of hypersensitivity occur, stop taking aceclofenac. In special cases, chickenpox can cause complications: serious infections of the skin and soft tissues. At present, the role of NSAIDs in worsening the course of these infections cannot be ruled out. Therefore, you should avoid taking aceclofenac for chickenpox. Hematological disorders Aceclofenac may cause reversible inhibition of platelet aggregation (see section "Interactions"). Respiratory system disorders Caution should be exercised when taking the drug in patients with current or history of bronchial asthma, since taking NSAIDs may trigger the development of sudden bronchospasm in such patients. Elderly Caution should be exercised when taking the drug in elderly patients, as they are more likely to experience side effects (especially bleeding and perforation of the gastrointestinal tract) when taking NSAIDs. Complications can be fatal. In addition, older patients are more likely to suffer from kidney, liver or cardiovascular diseases. Long-term use All patients receiving long-term treatment with nonsteroidal anti-inflammatory drugs should be closely monitored (eg, complete blood count, liver function tests, and renal function tests).
Interaction with other drugs
No drug interaction studies have been conducted with the exception of warfarin. Aceclofenac is metabolized by cytochrome P450 2C9, and in vitro data indicate that aceclofenac may be an inhibitor of this enzyme. Thus, the risk of pharmacokinetic interaction is possible when taken concomitantly with phenytoin, cimetidine, tolbutamide, phenylbutazone, amiodarone, miconazole and sulfaphenazole. As with other NSAID drugs, the risk of pharmacokinetic interactions with other drugs that are eliminated from the body by active renal secretion, such as metorexate and lithium preparations, also increases. Aceclofenac is almost completely bound to plasma albumin and, therefore, there is the possibility of displacement interactions with other protein-bound drugs. Due to the lack of studies on the pharmacokinetic interaction of aceclofenac, the following information is based on data from other NSAIDs: Concomitant use should be avoided: Methotrexate: NSAIDs inhibit the tubular secretion of methotrexate; Moreover, a slight metabolic interaction may occur, resulting in decreased methotrexate clearance. Therefore, when using high doses of methotrexate, NSAIDs should be avoided. Lithium and digoxin: Some NSAIDs inhibit the renal clearance of lithium and digoxin, resulting in increased serum concentrations of both substances. Coadministration should be avoided unless lithium and digoxin concentrations are monitored frequently. Anticoagulants: NSAIDs inhibit platelet aggregation and damage the gastrointestinal mucosa, which may enhance the effects of anticoagulants and increase the risk of gastrointestinal bleeding in patients taking anticoagulants. The combined use of aceclofenac and oral coumarin anticoagulants, ticlopidine and thrombolytics should be avoided unless the patient is closely monitored. Antiplatelet agents and selective serotonin reuptake inhibitors (SSRIs) when used together with NSAIDs may increase the risk of gastrointestinal bleeding (see Precautions section). The following combinations require dose adjustment and use with caution: Methotrexate: the possible interaction of NSAIDs and methotrexate should be kept in mind, even at low doses of methotrexate, especially in patients with impaired renal function. During concomitant use, renal function should be monitored. Caution should be exercised if both NSAIDs and methotrexate are taken within 24 hours, as the concentration of methotrexate may increase, increasing the toxicity of this drug. Cyclosporine, tacrolimus: When taking NSAIDs concomitantly with cyclosporine or tacrolimus, the risk of increased nephrotoxicity due to decreased renal prostacyclin formation should be considered. Therefore, renal function should be carefully monitored during concomitant use. Other NSAIDs: Concomitant use of acetylsalicylic acid or other NSAIDs may increase the incidence of side effects, so caution should be exercised. Corticosteroids: The risk of ulcers or bleeding from the gastrointestinal tract increases (see section "Precautions"). Diuretics: aceclofenac, like other NSAIDs, can inhibit the activity of diuretics and can reduce the diuretic effect of furosemide and bumetanide and the antihypertensive effect of thiazides. Concomitant use with potassium-sparing diuretics may lead to an increase in potassium levels; therefore, it is necessary to regularly monitor serum potassium levels. Aceclofenac did not affect blood pressure control when used in combination with bendrofluazide, although interaction with other diuretics cannot be excluded. Antihypertensive drugs: NSAIDs may also reduce the effect of antihypertensive drugs. Concomitant use of ACE inhibitors or angiotensin II receptor antagonists and NSAIDs may lead to impaired renal function. The risk of acute renal failure, which is usually reversible, may be increased in some patients with impaired renal function, such as elderly or dehydrated patients. Therefore, when used together with NSAIDs, caution should be exercised, especially in elderly patients. Patients should consume the required amount of fluid and be under appropriate monitoring (monitoring of renal function at the beginning of co-administration and periodically during treatment). Hypoglycemic agents: Clinical studies show that diclofenac can be used in conjunction with oral hypoglycemic agents without affecting their clinical effect. However, there are isolated reports of hypoglycemic and hyperglycemic effects of the drug. Thus, when taking aceclofenac, dosages of drugs that can cause hypoglycemia should be adjusted. Zidovudine: The risk of hematological toxicity increases when NSAIDs are taken concomitantly with zidovudine. There is evidence of an increased risk of hemarthrosis and hematomas in HIV (+) patients with hemophilia receiving zidovudine and ibuprofen.
Contraindications
Aceclofenac is contraindicated in the following cases: Hypersensitivity to the active substance or other excipients listed in the “Composition” section; Patients in whom substances with the same effect (for example, acetylsalicylic acid or other NSAIDs) provoked attacks of asthma, bronchospasm, acute rhinitis or urticaria; or if there is hypersensitivity to these substances; Patients who have had cases of bleeding or gastrointestinal perforation due to taking NSAIDs. Patients with a history of acute, recurrent or possible gastric or duodenal ulcer or bleeding (two or more clear and proven episodes of ulcer or bleeding); Patients with acute bleeding or diseases accompanied by bleeding (hemophilia or bleeding disorders); Heart failure (NYHA functional class ll-IV), coronary heart disease, peripheral arterial disease or cerebrovascular disease. Severe dysfunction of the liver and kidneys. During pregnancy, especially in the last trimester, with the exception of serious indications for use. In this case, the minimum effective dose should be used (see section "Pregnancy and lactation").
Compound
One capsule contains: aceclofenac - 100 mg. Excipients: croscarmellose sodium, microcrystalline cellulose, colloidal anhydrous silicon dioxide, magnesium stearate. Composition of the capsule shell: gelatin, glycerin, sodium lauryl sulfate, purified water, titanium dioxide E-171, charming red dye E-129.
Overdose
There is no data on an overdose of aceclofenac in humans. Symptoms include headache, nausea, vomiting, elegastric pain, gastrointestinal irritation, gastrointestinal bleeding, rarely diarrhea, confusion, agitation, coma, drowsiness, dizziness, tinnitus, hypotension, respiratory depression, syncope, rarely seizures . In case of severe poisoning, acute renal failure and liver damage are possible. Treatment of poisoning: If necessary, symptomatic therapy should be carried out. Activated charcoal should be taken within one hour after taking a toxic amount of the drug. As an alternative, gastric lavage may be considered in adult patients in the first hour after taking a potentially life-threatening dose. Specific interventions, such as hemodialysis or hemoperfusion, are likely to be ineffective in eliminating NSAIDs due to their high degree of protein binding and extensive metabolism. Good diuresis should be ensured, and renal and liver function should be carefully monitored. The patient should be observed for at least 4 hours after taking a potentially toxic dose. If frequent or prolonged seizures develop, intravenous diazepam should be used. Other measures may be necessary depending on the patient's clinical condition. Treatment of acute NSAID poisoning mainly consists of supportive and symptomatic therapy.
Side effect
Gastrointestinal Disorders: Most commonly observed side effects are gastrointestinal disturbances. Stomach ulcers, perforation or bleeding from the gastrointestinal tract may occur, sometimes leading to death, especially in elderly patients (see section "Precautions"). Nausea, vomiting, diarrhea, bloating, constipation, dyspepsia, stomach pain, melena, hematemesis, ulcerative stomatitis, exacerbation of colitis and Crohn's disease have been observed when taking NSAIDs (see Precautions). Gastritis is less common. Edema, hypertension and heart failure have been reported in association with NSAID use. Clinical studies and epidemiological data indicate that some NSAIDs (especially at high doses and long-term use) may slightly increase the risk of arterial thrombotic events (eg, myocardial infarction or stroke) (see Precautions section). The following table summarizes the adverse events reported from clinical studies and post-marketing surveillance; Adverse events are grouped according to organ system classes and frequency of occurrence. Very often (? 1/10), often (from ? 1/100 to 1/1,000), very rarely (
Storage conditions
Store in a place protected from moisture and light at a temperature of 15°C to 25°C. Store out of the reach of children.