Syncoma or fainting is a temporary loss of consciousness associated with circulatory failure in the brain. The pathology clinic includes precursors of syncope (an attack of dizziness, fog or flashing black dots before the eyes), an unconscious period and a recovery stage in which low blood pressure and weakness are noted.
Sources of development
In a healthy person, from 60 to 100 ml of blood moves through the cerebral arteries for every 100 g of GM substance every minute. A sharp drop in the reading to a level of up to 20 mg leads to short-term fainting. The list of factors influencing the occurrence of syncope is presented:
- decreased cardiac output (severe arrhythmia, heart attack, acute massive blood loss, ventricular tachycardia, slow heartbeat, hypovolemia arising from diarrhea of profuse etiology);
- decrease in the volume of the lumen of the cerebral arteries (atherosclerosis, spasm of blood vessels, occlusion of the carotid artery);
- dilatation of blood vessels;
- orthostatic collapse due to a sudden change in body position.
Neuroreflex changes in vascular tone are considered the main primary source of the formation of fainting. For their appearance, the following factors must be present:
- unstable psycho-emotional status;
- pain syndrome;
- irritation during swallowing, coughing or sneezing of the CS and the 10th pair of cranial nerves (Roemheld syndrome, examination of the eardrums);
- renal colic, exacerbation of inflammation of the gallbladder;
- neuralgia: trigeminal or glossopharyngeal nerve;
- VSD, excess of medication norms.
The second mechanism that causes syncoma is a drop in oxygen content in the blood. Fainting of this type occurs against the background of:
- blood pathologies - iron deficiency or sickle cell anemic condition;
- respiratory lesions, concentrated carbon monoxide poisoning.
A decrease in CO2 contained in the bloodstream during intense breathing also provokes fainting. About 41% of the causes of syncoma cannot be recognized.
Prehospital management of syncope
The word “syncope” is of Greek origin (“syn” - “with, together”; “koptein” - “to interrupt”). Syncope is a condition characterized by spontaneously occurring, transient disturbances of consciousness, usually leading to a fall. In some cases, the development of syncope is preceded by a variety of symptoms (weakness, sweating, headache, dizziness, visual disturbances), but more often syncope develops suddenly, sometimes against the background of complete “well-being”.
The duration of loss of consciousness during syncope, as a rule, is 15–30 s, less often it lasts up to several minutes. Prolonged syncope can cause significant difficulties in differential diagnosis with other conditions characterized by disorders of consciousness.
The cause of syncope is a sudden onset of impaired cerebral perfusion. Normally, minute blood flow through the cerebral arteries is 60-100 ml/100 g. Its rapid decrease (less than 20 ml/100 g per minute), as well as a rapid decrease in blood oxygenation, leads to loss of consciousness.
The reasons for a sharp drop in brain oxygenation may be:
- reflex decrease in arterial tone and/or decrease in cardiac output;
- heart rhythm disturbances (brady- and tachyarrhythmias, episodes of asystole);
- pathological changes in the myocardium, leading to significant disturbances in intracardiac hemodynamics.
The orthostatic mechanism for the development of syncope is based on the fact that the autonomic nervous system is unable to maintain sufficient vascular tone or is a consequence of a decrease in circulating blood volume (CBV). Such phenomena are often observed in Parkinson's disease, diabetic and amyloid neuropathy.
A decrease in blood volume can occur with vomiting, diarrhea, Addison's disease, after bleeding and during pregnancy.
Orthostatic reactions can develop against the background of alcohol intake and the use of a number of antihypertensive drugs, both blocking the sympathetic effect on blood vessels (α-blockers, calcium antagonists, centrally acting drugs), and causing a decrease in blood volume (diuretics) or depositing blood in the venous bed (donors NO groups, including nitrates). In addition, orthostatic reactions are possible when using psychotropic drugs (neuroleptics, tricyclic antidepressants, MAO inhibitors).
The absence of visible causes for the development of orthostatic hypotension may suggest the presence of idiopathic primary autonomic failure, and the combination with tremor and extrapyramidal disorders may suggest Shy-Drager syndrome.
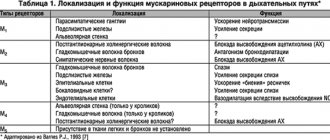
The basis of “neuroreflex syncope syndrome” is the activation of various reflex zones, causing bradycardia and vasodilation.
Table 1 provides a list of the most common receptor locations and situations leading to their activation.
Correct collection of complaints and medical history can greatly help in establishing the causes of syncope.
- Determining the position in which syncope developed (standing, lying, sitting).
- Clarification of the nature of the actions that led to syncope (standing, walking, turning the neck, physical stress, defecation, urination, coughing, sneezing, swallowing). For example, an “exclusive” diagnosis such as myxoma cannot be excluded if syncope developed when turning from side to side. In case of syncope, which stereotypically occurs during defecation, urination, coughing or swallowing, we can talk about situational fainting.
- Antecedent events (overeating, emotional reactions).
- Identification of precursors of syncope (headache, dizziness, “aura”, weakness, visual impairment, etc.).
- Clarification of the circumstances of the development of the syncope episode itself - duration, nature of the fall (supine, “sliding” or the patient slowly dropped to his knees), skin color, presence or absence of convulsions and tongue biting, presence of external respiratory disorders.
- Characteristics of syncope resolution include the presence of lethargy or confusion, involuntary urination or defecation, changes in skin color, nausea and vomiting, and palpitations.
- Anamnestic factors - family history of sudden death, heart disease, fainting; a history of heart disease, lung disease, metabolic disorders (primarily diabetes mellitus and adrenal pathology); taking medications; information about previous syncope and examination results (if performed).
At the prehospital stage, all patients are shown an ECG - a study that often allows one to confirm (but not exclude!) the arrhythmic or myocardial origin of syncope.
To exclude/confirm the orthostatic origin of syncope, a simple test can be performed when measuring blood pressure. The first measurement is taken after the patient remains in the supine position for five minutes. The patient then stands up and measurements are repeated after 1 and 3 minutes. In cases where the decrease in systolic pressure is more than 20 mm Hg. Art. (or below 90 mm Hg) is fixed for 1 or 3 minutes, the sample should be considered positive. If the pressure reduction indicators do not reach the specified values, but by the third minute the pressure continues to decrease, measurements should be continued every 2 minutes either until the indicators stabilize or until critical figures are reached.
Blood pressure measurements should be taken on both arms. If the difference exceeds 10 mm Hg. Art., one may suspect the presence of aortoarteritis, subclavian artery syndrome, or aneurysm dissection in the area of the aortic arch.
Auscultation of heart sounds may provide information regarding the presence of valvular disease, and an intermittent murmur depending on body position may suggest myxoma.
Due to the risk of cerebral circulatory disorders, a test with massage of the carotid sinus should not be carried out at the prehospital stage, although during examination in a hospital it can with a high degree of reliability identify the so-called “carotid sinus syndrome” - a disease in which fainting conditions can be provoked by everyday causes (tight collar, tie, irritation of the reflex zone when shaving, etc.).
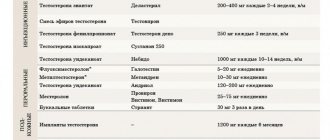
Most syncope conditions do not require specific pharmacotherapy at the prehospital stage. The use of medications is indicated only for the treatment of underlying diseases that are the direct cause of the disorder of consciousness: 40-60 ml of glucose 40% for hypoglycemia; subcutaneous administration of 0.5-1.0 ml of atropine sulfate for severe bradycardia; glucocorticoids for adrenal insufficiency, etc.
Vasovagal fainting and other manifestations of neuroreflex syndrome require measures of an exclusively general nature - the patient should be placed in a place with open access to fresh air (it should not be hot!), unfasten tight clothing (belt, collar, corset, bra, tie), give the legs an elevated position . You can turn your head to the side so that your tongue does not sink in only if you are absolutely sure that there are no lesions of the subclavian, carotid and vertebral arteries.
Painful stimuli, as a rule, are not required - the patient soon regains consciousness on his own. Sometimes a cotton swab with ammonia placed to the nose or sprinkling the face with cold water can help speed up the return of consciousness. The last two effects lead to activation of the vasomotor and respiratory centers.
The development of orthostatic hypotension may require measures to eliminate its causes - severe hypovolemia is corrected by intravenous administration of plasma-substituting solutions; in case of an overdose of α-adrenergic blocking drugs, midadrin (gutron) 5-20 mg intravenous bolus can be administered with caution. The dose is titrated under blood pressure control, taking into account that administration of 5 mg increases SBP by approximately 10 mmHg. Art. In case of severe drug-induced collapse, it is possible to administer phenylephrine (mesatone) - up to 1 ml of a 1% solution subcutaneously or 0.1-0.5 ml intravenously.
As a rule, syncope is not characterized by long-term breathing disorders, so therapy with respiratory analeptics is practically not indicated.
It should be borne in mind that the undifferentiated use of pressor amines (dopamine, norepinephrine) is not only not indicated, but can also be potentially dangerous: for example, in patients with arrhythmias or cerebral steal syndrome.
Glucocorticoids are used only for primary or secondary Addisonism or if anaphylactoid syncope is suspected.
The following patients are subject to hospitalization in order to clarify the diagnosis: with suspected heart disease; with changes on the ECG; with the development of syncope during exercise; with a family history of sudden death; with sensations of arrhythmia/interruptions in the heart immediately before syncope; with recurrent syncope; with the development of syncope in the supine position.
Patients are subject to hospitalization for treatment: with rhythm and conduction disturbances leading to the development of syncope; with secondary syncope due to heart and lung diseases; in the presence of acute neurological symptoms; with disturbances in the work of a permanent pacemaker; with injuries resulting from a fall during syncope.
The primary cause of arrhythmic syncope may be: dysfunction of the sinus node and atrioventricular conduction, paroxysmal tachyarrhythmias accompanied by a critical decrease in cardiac output, including arrhythmias that occur with congenital syndromes (long QT, Brugard, WPW, etc.), dysfunction of the implanted formerly a pacemaker.
Common cardiac causes of syncope include valvular pathology, hypertrophic cardiomyopathy and subaortic muscular stenosis, myxoma, acute myocardial ischemia, pericardial effusion with acute tamponade, dissecting aortic aneurysm, pulmonary embolism, and pulmonary hypertension.
Cerebrovascular causes of syncope include steal syndrome, which occurs both as a result of partial vasodilatation and increased mosaicity of cerebral blood flow, and as a result of arterial hypotension caused by other reasons. Quite rarely, the cause may be the so-called “subclavian artery syndrome”.
Other causes of short-term disturbances of consciousness should be differentiated from syncope proper (see Table 2).
A. L. Vertkin, Doctor of Medical Sciences, Professor O. B. Talibov, Candidate of Medical Sciences, NNPO Emergency Medical Care MGMSU, Moscow
Symptoms of individual subtypes of pathology
Each subtype of syncope has its own clinical manifestations:
Vasovagal
It is considered one of the most frequently recorded, the pathogenesis of the disease is a sharp increase in the lumens of peripheral vessels. The source of the attack becomes:
- standing for a long time;
- stuffy room;
- overheating under the sun or in a sauna;
- excess of emotions;
- painful sensations.
When the victim manages to leave the place leading to fainting, the problem is limited to loss of strength. This type of disease goes through stages:
- the first 3 minutes patients feel unwell;
- the second stage of unconsciousness lasts up to 2 minutes, with increased sweating, muscle hypotension, pale skin, decreased blood pressure and a thready pulse at a normal heart rate.
The last period lasts 5-60 minutes, the patient feels severe weakness.
Cerebrovascular
It is formed in the presence of neck pathology and is provoked by sudden changes in head position. Clamping of the artery provokes cerebrovascular insufficiency and loss of consciousness. At the pre-fainting stage, extraneous noise in the ears, flashing of black dots before the eyes, and occasionally a headache attack are registered. During and immediately after fainting, a decrease in muscle tone is observed.
Irritative
It develops after a reflex slowing of the heartbeat associated with irritation of the vagus nerve by impulses coming from receptor zones. Pathological deviation is associated with:
- with duodenal ulcer;
- excessive activity of the bile ducts;
- cardiospasm.
Each type of fainting has its own triggers: the process of swallowing, gastroscopy, pain attack. Patients experience stereotypical short-term loss of consciousness up to 2 minutes, without a preliminary phase.
Cardiogenic and arrhythmogenic
The anomaly occurs in 13% of patients with myocardial infarction. Features of symptoms include:
- cardiogenic collapse;
- deep fainting;
- its repetition when trying to get up.
With MES, there are no warning signs, it is impossible to feel the pulse and listen to the heartbeat, the skin is pale with a slight blue tint. The patient's consciousness is restored after the first heartbeat.
Orthostatic
Develops during the transition from a lying to a standing position. Occurs with hypotension, VSD, weakened or elderly organism. This subtype of deviation is not pathological and does not require specific treatment.
Causes
Disorder of the function and regulation of the cardiovascular system:
- arterial hypotension;
- the body’s reaction to different types of physiological changes - urination, coughing, cold air, swallowing reflex, defecation;
- a reflex state when the nervous regulation of blood vessels is disrupted - they expand, the pressure drops;
- increased oxygen supply to the pulmonary system (hyperventilation);
- increased excitability of the vagus nerve, which reflexively leads to a drop in blood pressure.
Mechanical processes leading to obstruction of blood flow in the heart and large vessels:
- arrhythmia;
- difficulty in blood supply to the brain due to ischemia and the formation of blood clots.
Primary diseases:
- hypoglycemia;
- seizures in epilepsy;
- bronchial asthma, pneumonia, carbon monoxide poisoning;
- severe pain syndrome with colic, neuralgia.
Syncope occurs when certain medications are taken without a doctor's approval.
Symptoms
Clinical symptoms of the period before syncope:
- pale, bluish skin;
- cold sweat;
- tachycardia;
- lack of orientation in space;
- numbness of the limbs, lack of sensitivity.
During the period of fainting, the signs change:
- the skin takes on a gray tint;
- weak pulse, muscle tone;
- pupils dilated;
- there is no consciousness.
If the condition is caused by fainting, it takes 5 to 30 seconds for the person to return to consciousness.
Make an appointment with a neurologist
Kinds
There are 2 main forms of syncope. They are associated with neurological disorders or diseases of the cardiovascular system.
Neurogenic syncope
They arise due to a decrease in vascular tone due to the pathology of reflexes under the influence of external stimuli. The following features are characteristic:
- vascular tone reflexively decreases, blood pressure drops;
- a fainting state develops over a short period, muscle weakness, nausea, ringing in the ears, spots and darkness before the eyes appear;
- consciousness is quickly restored;
- after fainting the patient feels well.
Neurogenic syncope falls into several categories.
- Vasodepressor. It is typical for young people under the influence of negative factors - prolonged hunger, acute pain, fear, stress, reduced oxygen concentration in the air. Does not threaten life or health.
- Orthostatic. It is formed due to a rapid change in the position of the body in space (from horizontal to vertical, and vice versa). The condition is formed due to a violation of autonomic neuroregulation. In everyday life, the patient is characterized by weakness, constant fatigue, decreased performance, headache, and dizziness. Orthostatic syncope occurs after a serious illness, surgery, prolonged bed rest, or misuse of antidepressants and antipsychotics.
- Vestibular. Occurs with increased sensitivity of the vestibular apparatus in young children or adolescents. For example, with prolonged swinging on a swing, seasickness, motion sickness in transport.
- Syncope with increased sensitivity of the carotid sinus. This is a neurological disorder of the vagus nerve. The condition is caused by bradycardia, arterial hypotension, and difficulty in cerebral circulation. Pathology occurs in elderly patients. Fainting is provoked by rapid movement, turning the head, squeezing the neck with a pillow, or excessively tightening the tie.
- Situational. Pathology is formed by physiological changes that lead to increased stress on the body. For example, prolonged cough, sports.
Pathology is differentiated by a cardiologist and a neurologist.
Fainting associated with diseases of the cardiovascular system
This form of syncope is not characterized by a pre-syncope state. There are 2 groups of fainting.
- Against the background of arrhythmia, changes in cardiac conductivity. Often observed in patients with paroxysmal tachycardia.
- Caused by difficulty in cardiac output. Formed during heart attack, ischemia or vascular aneurysm, cardiomyopathy.
Diagnosis is carried out by a cardiologist.
Syncope cannot be left unchecked. This is a signal to detect acute or chronic disease. Less commonly, the pathology is provoked by serious infectious diseases (influenza, parainfluenza, typhus, hepatitis, dysentery).