According to the form of its course, bronchitis is divided into acute and chronic.
Chronic bronchitis
is a chronic inflammation of the bronchial tubes.
Chronic bronchitis is considered if the cough continues for at least three months a year for two years in a row. According to etiology
(causes of occurrence),
viral, bacterial and allergic bronchitis are distinguished.
More than 80% of bronchitis is viral, infection occurs through airborne droplets, and proceeds like a normal acute respiratory viral infection, with the difference that the viruses that cause bronchitis prefer to “settle” in the bronchial tissue.
Symptoms of bronchitis
- Bronchitis has classic symptoms for any ARVI:
- Increased body temperature
- A sore throat
- Runny nose
- Shortness of breath, difficulty breathing, noisy breathing (not always)
- Crepitating (crackling) and quiet whistling rales
- Cough
The main and main symptom of bronchitis is cough.
It can be dry or wet, depending on the form of the disease and the stage of its course. One of the variants of the course of bronchitis in children is obstructive bronchitis - this is a condition in which spasm of the bronchi occurs, the mucous membrane swells, and phlegm becomes difficult to discharge - it accumulates in the bronchi, causing difficulty breathing. Bronchial spasm also contributes to difficulty breathing - this is the main danger of obstructive bronchitis - the baby begins to choke. Obstructive bronchitis is characterized by noisy exhalation with a whistle.
Recurrent bronchitis in a child
However, in some cases, bronchitis in a child becomes recurrent. In such cases, the outpatient tactics of pediatricians, unfortunately, often come down to monthly prescription of antibiotics. I have met parents of children who were given the idea by a certain doctor that their child could not get better without antibiotics. They laughed at the word inhalation and demanded from me another antibiotic for their child, like a dose for a drug addict.
This sad case should alert you if you see that the doctor prefers what he thinks is the easiest way to treat bronchitis in your child, especially if this is not the first bronchitis. In this case, you may need to consult an allergist-immunologist, who will have to collect a very thorough medical history, that is, study the life history of not only the child himself, but also his parents, as well as grandparents at a minimum. Next, it may be necessary to conduct a special allergological examination, since recurrent bronchitis is nothing more than a harbinger of bronchial asthma - already a chronic disease of the bronchi. Let me warn you right away that in a small child we are not always able to carry out the full range of necessary diagnostic procedures, so sometimes the establishment of a final diagnosis is postponed by an allergist-immunologist until an older age, but the doctor can still prescribe preventive anti-relapse treatment, which should help both times to avoid such a diagnosis in the future. In general, based on clinical practice, I can say that even in a child under three years of age, the presence of more than two episodes of obstructive bronchitis is already a reason to consult an allergist-immunologist.
Diagnosis of bronchitis
To diagnose bronchitis, neither an X-ray examination nor additional tests are needed.
To make a diagnosis, the doctor simply needs to perform auscultation - listen to the lungs using a phonendoscope - an experienced pediatrician will immediately “hear bronchitis”. Additional examinations are prescribed
in order to determine the type of bronchitis - viral or bacterial - the purpose of therapy depends on this. As you know, antibiotics have no effect on viruses, so they are prescribed only if the doctor believes that bronchitis is bacterial in nature. A blood test can tell you this. Also, the pediatrician determines the type of bronchitis by collecting an anamnesis (medical history): how long has the child been sick, how the disease progresses, how long ago was it sick last time, how was it treated, etc.
X-ray
for bronchitis, they may be prescribed in order to exclude pneumonia, a possible complication of this disease. Unfortunately, it is difficult to diagnose pneumonia in young children without an x-ray - local changes in some segments of the lungs cannot always be heard.
The best medicine for bronchitis
Research has found that bronchitis most often affects people with weakened immune systems and those exposed to significant risk factors.
The risk of disease is reduced if you follow a balanced diet that provides the body with essential nutrients - proteins, fats, carbohydrates, minerals and vitamins. Their deficiency weakens the body's protective functions. An active, mobile lifestyle also increases resistance to respiratory diseases.
The best cure for bronchitis is exercise
Bronchitis is often caused by viral infections. Vaccination helps to significantly reduce the risk of infection by viruses. Some vaccinations are given during childhood, while others are seasonal, such as the flu vaccine, which is given before the highest flu season. Even if a vaccinated person gets sick, in this case the disease is much milder and does not cause consequences.
Quitting smoking and alcohol abuse, which suppresses the effect of certain vitamins, disrupts metabolism, impairs heat exchange, also has a beneficial effect on the prevention of bronchitis and other respiratory diseases.
School of Doctor Komarovsky. About bronchitis.
How to treat bronchitis
There is no universal treatment regimen for bronchitis.
The choice of therapy depends on many factors: the type of bronchitis (viral or bacterial), duration, characteristics of the course of the disease, cough (it can be dry, wet, only during sleep or after sleep, etc.), the condition of the child.
When treating bronchitis
, it is very important that normal air humidity (40-60%) is maintained in the room where the child is located. It is necessary to protect the patient from tobacco smoke (passive smoking during bronchitis is very dangerous).
Is it possible to use antitussive drugs?
A severe cough exhausts both the baby and family members. Of course, you want to alleviate the child’s condition by giving him a drug that relieves cough. But you should absolutely not do this without a doctor’s recommendation! Why? Firstly
, there are a great variety of antitussive drugs, and it is difficult to choose the right one on your own.
There is no drug that can be used from the beginning to the end of the disease - the active substance is selected depending on the stage. Secondly,
an unreasonable selection of an antitussive drug can provoke complications, for example: you gave a child a medicine that suppresses cough at a time when sputum begins to separate, because of this he cannot get rid of sputum, it stagnates and leads to pneumonia.
Thirdly,
children's medications are produced mainly in the form of syrups containing fragrances, flavors, preservatives, stabilizers, etc. - these components often cause allergies.
What you need to pay special attention to
If your child's condition worsens or new symptoms appear
- Cough does not go away after a month
- Bronchitis recurs (more than three episodes per year)
In these cases, be sure to show the child to the pediatrician!
SEPARATELY Do I need to see a doctor for a common acute respiratory infection? Young children can get sick with acute respiratory infections 8-12 times a year - and this is normal, since their immunity is developing, their body is just getting acquainted and learning to resist many viruses and bacteria. And parents, already accustomed to endless colds, often treat the child themselves - because they do not see the point in visiting a doctor every time the child gets sick. But the problem is that only a doctor can determine whether your child has a truly banal acute respiratory infection that does not require drug treatment and intervention in its course, or a more serious condition. In children, all processes go quickly, not all diseases have an acute onset, and without the control of an experienced doctor, you can very easily miss a complication or a more serious illness: the same bronchitis, tracheitis, pneumonia, etc. In addition, children usually play even with a serious illness , jumping and running, which can mislead parents regarding the actual severity of the disease. Therefore, if your child gets sick, be sure to show him to the pediatrician - after all, only a doctor can objectively assess your baby’s condition!
Inhalations: benefits and harm Now nebulizers, devices for inhalation, are extremely popular among parents. Doctors unanimously agree that inhalations are a good thing. Using this device, we can deliver the medicine directly to the bronchi, which reduces the load on the gastrointestinal tract and circulatory system and ensures the rapid action of the drug. But! A nebulizer can only be used when indicated and when using certain medications prescribed by a doctor. Nebulizers are designed to deliver medication to the middle sections of the respiratory system, that is, they are effective for bronchitis and asthma. They should be used with caution for upper respiratory tract diseases (common acute respiratory infections or acute respiratory viral infections). Why? Firstly, because the drugs used to treat the lower respiratory tract are not effective in the inflammatory process in the nasal cavity and pharynx, and secondly, for using a nebulizer for diseases of the upper respiratory tract there are a number of conditions and rules that only doctor.
Acute bronchitis - symptoms and treatment
Uncomplicated forms of acute bronchitis
Treatment of uncomplicated forms of acute bronchitis is carried out on an outpatient basis.
Patients need to know the “red flags,” i.e., symptoms that require immediate medical attention. Hospitalization for bronchitis will be required in the following cases:
- High fever, chest pain or headaches increase after 2-3 days of treatment.
- Breathing problems such as wheezing or shortness of breath occur.
- Cough with blood discharge. The blood may be bright red, but the sputum may be dark or rusty in color.
- Severe weakness, lethargy.
- The cough lasts longer than 3-4 weeks.
- The child’s young age and social conditions (the family, for some reason, cannot care for the child at home).
- The presence of concomitant serious diseases (congenital malformations of the lungs, heart, diabetes mellitus, bronchial asthma).
These symptoms may indicate a complicated course or development of chronic bronchitis.
It is not recommended to use in therapy:
- Antihistamines (use is justified only when allergies occur in acute bronchitis) and physiotherapeutic treatment due to the lack of evidence of their effectiveness.
- Mustard plasters, pepper plasters, jars. The harm from their use significantly outweighs the possible benefits (there is a possibility of allergic reactions and thermal burns).
- Antibiotics for viral, uncomplicated acute bronchitis [9].
- Medicinal herbs, as there is insufficient evidence of their effectiveness and safety [10].
There is no “quick fix” for a cough due to a viral infection. The main goal of treating bronchitis is to relieve symptoms while the patient's immune system fights off the infection. The most effective methods of treating acute viral bronchitis:
- Prescription of antiviral drugs (only for flu symptoms) [11].
- Taking paracetamol, ibuprofen in age-appropriate dosages to reduce high fever and relieve any pain.
- Drink plenty of fluids to prevent dehydration [12].
- Frequent ventilation of the room, creating optimal humidity levels (40-50%) and temperature 19-22 °C.
- To give up smoking. Cough and serious lung diseases are more common in smokers.
Patients, as a rule, buy a wide variety of cold and cough remedies at the pharmacy. There is little evidence of any effect on infection, but some may be useful in relieving certain symptoms of acute bronchitis. For example, vasoconstrictor drops help relieve symptoms of nasal congestion.
In March 2009, the Medicines and Healthcare Products Regulatory Agency (MHRA, UK) released an important statement stating:
Parents and guardians should no longer use over-the-counter cough and cold medications on children under 6 years of age. There is no evidence that they work, and they may cause side effects such as allergic reactions, sleep disturbances, etc. For adults looking for a cough suppressant (for short-term use only), over-the-counter medications with some evidence of effectiveness include dextromethorphan, guaifenesin, dexbrompheniramine/pseudoephedrine and bromhexine. Codeine is not an effective cough suppressant and should be avoided. Products containing pelargonium (Pelargonium sidoides) extract, such as Umcka ColdCare, may reduce symptoms and speed resolution of acute bronchitis in adults. Significant improvements in cough relief have been observed with Vicks Medinite syrup [13]
Recommendations of the Russian Federation
For dry, painful, painful cough, absence of wheezing in the lungs and other signs of bronchial obstruction, butamirate can be used. For viscous, poorly discharged sputum, it is possible to prescribe ambroxol, and from the age of two - acetylcysteine and carbocysteine.
Acute obstructive bronchitis
Therapy of acute obstructive bronchitis has its own characteristics. Treatment is indicated using a device that sprays drugs directly into the respiratory tract - a compressor inhaler (nebulizer). Children under 5 years old - use a mask, over 5 years old - a mouthpiece.
The following drugs are used:
- Inhaled β2-agonists (salbutamol/Ventolin nebula) or combination drugs (fenoterol + ipratropium bromide - Berodual) are mixed with a solvent (0.9% sodium chloride solution) and are used to dilate the bronchi and relieve their edema [14].
- Inhaled corticosteroids (ICS) - a suspension of budesonide in nebulas. This is an effective anti-inflammatory drug with a high level of safety.
The second method, less preferable, is the administration of the same groups of drugs through a metered dose aerosol inhaler (MDI) with a spacer (special adapter) and an appropriate face mask or mouthpiece. The duration of the course, doses of drugs and the frequency of their use are determined by the doctor.
Syrup forms of bronchospasmolytics, including aminophylline, are not recommended due to possible side effects [15]:
- From the nervous system: headache, dizziness, increased nervous excitability, sleep disturbances, drowsiness, tremor, convulsions.
- From the digestive system: nausea, vomiting, diarrhea, exacerbation of gastric and duodenal ulcers, increased activity of hepatic transaminases (enzymes that reflect the functionality of the liver). It happens extremely rarely.
- From the cardiovascular system: tachycardia, decreased blood pressure, collapse (a life-threatening condition caused by a drop in blood pressure and deterioration of blood supply to vital organs).
- From the urinary system: pink coloration of urine.
- Allergic reactions: skin rash, urticaria, paradoxical bronchospasm.
Treatment of acute bronchiolitis
- Use of general principles for the treatment of acute bronchitis.
- Humidified oxygen therapy is recommended if the amount of oxygen in the blood (SpO2) is less than 92-94% (normal is 95-98%). Most often, oxygen therapy is carried out by insufflating oxygen through nasal catheters (cannulas) or a mask.
- Nebulizer therapy is selected individually and may include bronchodilators (drugs that relax the muscle elements in the wall of the bronchi and thereby increase their lumen), 3% sodium chloride solution, etc. The effect of glucocorticosteroid therapy has no evidence [16].
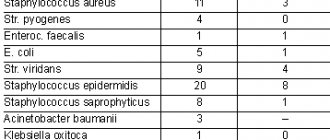
Bacterial bronchitis
For bronchitis caused by mycoplasma, chlamydia or whooping cough, it is recommended to prescribe antibacterial therapy with drugs from the macrolide group (josamycin, azithromycin, clarithromycin) [17]. If necessary, nebulizer therapy is carried out.
Antibacterial therapy is prescribed more actively if we are talking about risk groups:
- patients over 75 years of age with high fever;
- patients with concomitant severe chronic pathology (diabetes mellitus, heart failure, COPD);
- patients receiving immunosuppressive therapy;
- patients with alcohol dependence.
These people have an immunosuppressed state to begin with, so the risk of developing complications is higher than in the general population. If a decision is made about the need for antibiotic therapy, the starting antibiotic is usually amoxicillin [18].
Treatment of bronchitis with folk remedies
Preparations with pelargonium (Pelargonium sidoides) extract, such as Umcka ColdCare, can reduce symptoms and speed up the resolution of acute bronchitis in adults [13]. However, before taking the drug, you should consult your doctor.
Diet
A diet for bronchitis is not required. It is enough to maintain an adequate drinking regime.