The text is presented for informational purposes only. We strongly urge you not to self-medicate. When the first symptoms appear, consult a doctor. We recommend reading: “Why you can’t self-medicate?” Autoimmune diseases are the most complex and difficult to treat diseases caused by malfunctions of the immune system. They occur when the immune system attacks healthy cells in the body.
general characteristics
The human immune system is a complex of tissues, organs and cells. Its task is to protect the body from pathogens in the form of infections, bacteria, fungi and foreign bodies. But sometimes the system of recognizing “friends” and “strangers” fails. Then the immune system perceives healthy cells of the body as enemies and begins to attack them with the help of autoantibodies, in other words, it produces antibodies against “its own” cells.
Content:
- general characteristics
- Types of autoimmune diseases
- Risk factors for autoimmune diseases
- Diagnostic methods
- Traditional and modern treatments
Today, experts do not have enough knowledge to say exactly why autoimmune diseases occur. In addition, they are quite difficult to diagnose and treat. However, autoimmune diseases are very common. According to preliminary estimates by American experts, in the United States alone there are about 24 million people suffering from at least one disease from this group. These diseases can be localized to one organ or tissue, or systemic - affecting different parts of the body. However, even localized diseases often cause complications, affecting other organs. Interestingly, almost a quarter of people with autoimmune diseases are prone to developing other diseases from this group. If a patient has three or more autoimmune processes, they indicate the development of multiple autoimmune syndrome (MAS). But so far it is difficult for specialists to say why some people develop MAS.
Demyelination. Foci of demyelination
Myelin is the sheath of nerve fibers. Demyelination is the destruction of the nerve sheaths, and then the nerve fibers themselves. Demyelination of the brain, spinal cord, and peripheral nerves can occur for a variety of reasons. The most dangerous demyelination is due to the aggression of the immune system against myelin proteins. Treatment of demyelinating diseases in our clinic (DMD) involves searching for and treating the causes of demyelination and stimulating remyelination processes.
Possible causes of demyelination:
- Immune attack on proteins that make up myelin. This occurs due to an error by the immune system, under the influence of infection, or innate characteristics of the immune system. The immune system perceives myelin proteins as foreign and destroys them. This is typical for multiple sclerosis, multiple encephalomyelitis, chronic inflammatory demyelinating polyneuropathy (CIDP), Guillain-Barré syndrome, rheumatic diseases, and chronic infections.
- Metabolic disorders can lead to malnutrition and loss of myelin. This is typical for diabetes mellitus and thyroid diseases.
- Neuroinfection . Myelin can be a target of attack by certain infections, primarily viral ones.
- Paraneoplastic processes are complications of cancer.
- Intoxication with chemicals or aggressive waste products of the body itself (free radicals, peroxides).
Remyelination is the process of repairing myelin sheaths. The remyelination process can be stimulated in different ways - more details on this page
Types of autoimmune diseases
There are several types of autoimmune diseases that can affect different organs and systems of the body. Today, experts know about almost 80 types of autoimmune diseases. Some of them, such as autoimmune thyroiditis (Hashimoto's thyroiditis), are diagnosed quite often, while others are less common. Below we consider the most famous autoimmune diseases.
Systemic (affect several organs at once)
- Systemic lupus erythematosus. It is a chronic autoinflammatory disease that occurs more often in women. The main triggers for exacerbation of the disease: ultraviolet radiation, viral infections, stress. Against the background of the disease, problems arise with the skin, joints, kidneys, heart, brain, and the process of hematopoiesis is also disrupted.
- Acquired autoimmune disorders caused by the human immunodeficiency virus. HIV infection causes total destruction of the immune system, which leads to damage to most systems, organs and tissues of the body.
Other common types of systemic autoimmune diseases:
- dermatomyositis - affects the skin and muscles;
- rheumatoid arthritis – joints, lungs, skin, eyes suffer;
- scleroderma - damage to the skin, intestines, lungs, kidneys;
- Sjogren's syndrome - affects the salivary and lacrimal glands, joints.
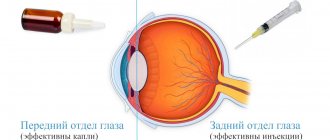
Affecting the apparatus of the eye
Acute anterior uveitis. This is the most common inflammatory disease of the iris. It is usually associated with the presence of the HLA-B27 antigen in the body.- Sjögren's syndrome. This is a disease in which the immune system attacks the exocrine glands (responsible for the production of tears and saliva).
Affecting the gastrointestinal tract
- Autoimmune hepatitis. Affects liver cells. Autoimmune hepatitis occurs in 1-2 people out of 100 thousand, and in women much more often than in men (out of 10 patients, 7 are women). Scientists have proven a genetic predisposition to this disease.
- Celiac disease. A condition in which the intestines react inappropriately to foods containing gluten. In this disorder, the lining of the small intestine becomes inflamed every time after eating food containing a specific protein.
- Inflammatory bowel disease. This is a general name for several diseases that cause chronic inflammation in the digestive tract. The most common diseases from this group are Crohn's disease and ulcerative colitis.
- Primary biliary cirrhosis. In this disorder, the immune system slowly destroys the bile ducts of the liver.
Affecting hematopoiesis and blood vessels
- Polyarteritis nodosa. A serious disease in which small and medium-sized arteries become inflamed and damaged. The risk of developing the disease increases against the background of hepatitis B and C.
- Antiphospholipid antibody syndrome. Leads to damage to blood vessels.
- Hemolytic anemia. This type of anemia occurs when immune cells attack blood cells.
- Idiopathic thrombocytopenic purpura. Causes platelet destruction.
Skin damage
- Scleroderma. This autoimmune disorder affects the connective tissues of the skin and blood vessels, as well as muscles and internal organs. The disease is more often diagnosed in women aged 30 to 50 years.
- Dermatomyositis. This condition results in muscle inflammation and is accompanied by a skin rash. Often appears in people with malignant tumors in the lungs or abdominal cavity.
- Psoriasis. A common autoimmune disease that causes scaly, dry, itchy patches on the skin. The disease is often accompanied by joint pain. The main triggers of the disease: stress, poor environment, infectious diseases.
- Vitiligo. In this condition, the cells containing skin pigment are destroyed, causing white spots to appear on the body. It most often affects people with dark skin.
- Alopecia areata. It develops when the immune system attacks hair follicles.
Hormone dependent
Diabetes mellitus type 1. This disease occurs because autoantibodies attack the cells of the pancreas that are responsible for producing insulin. The result is a lack of insulin, which causes glucose levels in the blood and urine to rise.- Autoimmune pancreatitis and hepatitis. This is an inflammation of the pancreas and liver caused by the pathogenic activity of immune cells.
- 21-hydroxylase deficiency. This disease affects the adrenal glands and leads to excessive production of the male sex hormones androgens.
- Autoimmune thyroiditis. During this disorder, the cells of the thyroid gland are destroyed, which leads to its insufficient activity. This disease can appear at any age, but is more common among middle-aged women.
- Basedow's disease (hyperthyroidism, Graves' disease). This autoimmune disorder causes an overactive thyroid gland.
Affecting the nervous system
- Multiple sclerosis. During the course of the disease, the brain cells and nervous system come under attack from the immune system. Autoimmune cells damage myelin sheaths, which serve as a protective covering for nerve cells.
- Myasthenia. In this disorder, the immune system attacks nerve endings and muscles, resulting in severe weakness.
Arthritis
- Ankylosing spondylitis (ankylosing spondylitis). This is a common form of chronic arthritis caused by an autoimmune disorder. The disease damages the joints of the spine and pelvis (sacroiliac joints) and paravertebral soft tissues. Progression of the disease leads to severe pain, skeletal deformation and disability.
- Reiter's syndrome. This is an inflammation that affects the joints, which often develops as a complication of certain infectious diseases (nasopharyngeal, genitourinary, intestinal). The disease, as a rule, affects large joints (knees and lower back), but at the same time it causes inflammation of the eyes (conjunctivitis, uveitis), in men - urethritis (inflammation of the urethra), in women - cervicitis (inflammation of the cervix).
- Rheumatoid arthritis. This is one of the most common autoimmune diseases. As a result of this disease, joint tissues suffer. The disease leads to inflammation and serious damage to cartilage tissue. As the disease progresses, the lungs, pleura, sclera of the eyes may be damaged, or pericarditis may begin.
Intoxication of the body. Removing intoxication. How to relieve intoxication?
Intoxication is a painful condition associated with poisoning by any harmful substance (toxin), which adversely affects the state of the nervous system, liver, etc. Intoxication can be associated with the ingestion of a toxin from the external environment (ingestion, inhalation of vapors, etc.) or its formation within the body during various diseases. Many toxins lead to the death of: peripheral nerves (toxic polyneuropathy); brain substances (toxic encephalopathy); spinal cord (toxic myelopathy). Treatment of toxic lesions (intoxication) of the nervous system in our clinic involves detoxification and treatment aimed at restoring the functioning of the nervous system. Commonly used drugs for detoxification:
- Detoxifiers,
- nootropics,
- Antioxidants,
- vitamins (in case of intoxication with alcohol, lead, manganese, etc., administration of vitamins through a dropper may be indicated),
- restorative treatment after intoxication.
Detoxification - removal from the body of the substance that caused toxic encephalopathy and administration of drugs.
Intoxication with various substances can lead to various symptoms from the central nervous system:
- Alcohol, when consumed regularly, causes damage to the peripheral nerves of the arms and legs (alcoholic polyneuropathy) and the brain (alcoholic encephalopathy). Read more about alcohol intoxication.
- Lead causes mental agitation, impaired memory and intelligence, pain in muscles and joints, damage to nerve cells in the spinal cord with paralysis and other disorders. Poisoning is typical when in contact with certain types of gasoline, vapors containing lead (evaporation from batteries and lead melts).
- Manganese encephalopathy usually develops after consuming ephedrone, a homemade narcotic drug containing large amounts of manganese. Parkinsonism is characteristic, with impaired coordination of movements, tremors of the limbs, difficulties in changing body position, up to complete immobility.
- Long-term exposure to metallic mercury leads to a characteristic combination of cerebellar symptoms with mercury erethism (irritability, memory loss, insomnia, pathological fearfulness and embarrassment). Sometimes psychosis with mental agitation (delirium) develops. It was first described in workers involved in the production of felt hats, and was even called “mad hatter disease.” In individuals with certain immune conditions, low doses of mercury from dental fillings may cause abnormal immune reactions, but data on this issue are not yet sufficient.
- Intoxication in diseases of the kidneys and liver is associated with increased formation and/or insufficient excretion of metabolic products. Accumulated harmful metabolic products can cause damage to peripheral nerves and the brain.
- Intoxication in infectious diseases is caused by the formation of toxins as a result of the activity of pathogenic microbes and the destruction of body cells.
Risk factors for autoimmune diseases
Autoimmune disorders can affect almost anyone. But researchers do acknowledge that some groups of people have a higher risk of getting the disease.
Main risk factors:
- Genetics. Research shows that children whose parents have autoimmune disorders are also at increased risk of developing the disease. For example, multiple sclerosis and lupus are often inherited.
- Floor. Women are generally more susceptible to autoimmune disorders. It may be due to hormones or the fact that women tend to have stronger immune systems than men. In addition, scientists have found that women of childbearing age are more likely to get sick.
- Age. Most often, diseases of this group occur in young and middle age.
- Ethnicity. American experts have found that autoimmune disorders are much more common among Native Americans, Hispanics and blacks than among Europeans and Asians. If we talk about statistics by type of disease, type 1 diabetes is more common in white people, and lupus erythematosus, for example, in representatives of the black race and indigenous people of Spanish-speaking countries (23 countries in Latin America, Africa and the Pacific). Scientists explain the influence of this factor by the presence of common genes among representatives of the same ethnic group, as well as the influence of the environment in which they live, including solar activity.
- Infection. If a person with a genetic predisposition has suffered from specific viral or bacterial infections, the risk that they may develop an autoimmune disease in the future increases even more.
Diagnostic methods
Because many autoimmune diseases have similar symptoms, diagnosing them is often challenging. For example, lupus affects the joints in the same way as rheumatoid arthritis, although the symptoms are less severe. Lyme disease also causes joint stiffness and inflammation, as in RA, although this disease is not an autoimmune disease (its causative agent is a bacterium carried by ticks). Inflammatory bowel disease often has symptoms similar to celiac disease. The only difference is that in the first case, it is not gluten that causes digestive problems. It is much easier to identify thyroid diseases. Typically, to make a diagnosis, it is enough to analyze the level of hormones produced by the gland and do some other specific tests.
Diagnosing autoimmune diseases in each specific case may require its own methods. For example, to make a diagnosis, a patient with rheumatoid arthritis will have to undergo a physical examination, blood tests and x-rays. These tests will help determine the type of arthritis and its severity.
The main test for determining any autoimmune disease is testing for the presence of a specific autoantibody. A complete blood count is also important, because when the immune system is fighting something, the number of red and white blood cells always deviates from the norm. A blood test for erythrocyte sedimentation rate and C-reactive protein will help determine the presence of an inflammatory process in the body, which accompanies all types of autoimmune disorders.
The most dangerous thing is that it can sometimes take years for a patient with autoimmune disorders to receive an accurate diagnosis, since in the early stages many diseases are similar to each other.
Is it possible to get vaccinated?
The vaccine is given only outside periods of exacerbation. The response to the vaccine depends on the type and severity of AIDS, the type of vaccine, the patient’s age, and treatment regimen [2–4].
Types of vaccines [2–4]:
- Live attenuated vaccines are highly effective. However, with reduced immunity, for example, while taking immunosuppressants, a weakened pathogen from a live vaccine can “take root” in the human body. In general, live vaccines are contraindicated in patients undergoing immunotherapy.
- Inactivated vaccines (with a “killed” pathogen) or inert (subunit, split vaccines - with a non-virulent fragment) are weaker than live ones. Adjuvants and revaccination are required. However, they are safer and less demanding on storage conditions than live vaccines.
- Recombinant (vector) vaccines consist of a non-pathogenic viral carrier and a DNA or RNA fragment of the pathogen. Some scientists suggest that the vector may behave like a virus from a live vaccine [11]. This has not been shown in practice. Their effectiveness and safety are comparable to inactivated ones.
- Prior to COVID-19 vaccines, messenger RNA vaccines There is not enough information to talk about the safety of this type of coronavirus vaccine for autoimmune diseases. At the same time, there are no theoretical grounds to assume the opposite.
BE CAREFUL
A patient with reduced immunity can become infected from a household member who has received a live vaccine against rotavirus, polio and some other infections.