Antiulcer drugs are a therapeutic group of drugs intended for the treatment of gastric and duodenal ulcers.
Despite the fact that the term antiulcer drugs has firmly entered the medical lexicon, it is more correct to talk not about antiulcer drugs, but about drugs for the treatment of so-called acid-dependent diseases, which are based on the aggressive, damaging effect of hydrochloric acid on the upper parts of the digestive tract.
In addition to peptic ulcers, such diseases include inflammation of the gastric mucosa, called gastritis. Gastritis usually precedes the development of peptic ulcers. If the duodenum is also involved in the inflammatory process, they speak of gastroduodenitis.
Despite the prevalence of such diseases as peptic ulcers of the stomach and duodenum, the causes that cause them remain unknown today.
A number of factors are believed to play a role in the development of these diseases. These include: excessive secretion of hydrochloric acid by the stomach, chronic stress, unhealthy diet, and, finally, genetic predisposition - the presence of these diseases in close relatives.
Relatively recently, the discovery was made that peptic ulcer disease can be of an infectious nature. A microorganism capable of living only in the very acidic environment of the stomach and which is no longer found in other organs was isolated from the stomach of patients with peptic ulcer disease.
It was found that this pathogen is capable of damaging the gastric mucosa, which is subsequently corroded by hydrochloric acid. This microorganism is called Helicobacter pylori, or simply Helicobacter pylori.
At the same time, this pathogen is detected in many people who do not have gastric ulcers. Perhaps several factors must coincide for the development of peptic ulcer disease. But this question, as already mentioned, remains open today.
Classification of antiulcer drugs
- Histamine H2 receptor blockers (ranitidine, famotidine).
- Proton pump inhibitors (omeprazole, pantoprazole, esomeprazole, lansoprazole, rabeprazole).
- Prostaglandins (misoprostol).
- M1 – anticholinergics (pirenzepine).
- Antacids (sodium bicarbonate, magnesium carbonate, calcium carbonate, aluminum phosphate, magnesium hydroxide, aluminum hydroxide).
- Gastroprotectors (sucralfate, bismuth subcitrate, alginic acid).
- Agents for the eradication (destruction) of Helicobacter (amoxicillin, tinidazole, clarithromycin).
Second option for first-line treatment of peptic ulcer
Bismuth tripotassium dicitrate (the international nonproprietary name of the drug, which is more familiar to practitioners under the name colloidal bismuth subcitrate or De-nol) 240 mg in combination with amoxicillin 1000 mg and clarithromycin 250 mg (accordingly, all drugs are prescribed 2 times a day) within 10 days.
Note:
- In the absence of ulcer healing (according to the results of the control endoscopy on days 11-12), treatment of patients is continued for another 3-4 weeks with bismuth tripotassium dicitrate 240 mg 2 times a day.
- If (before treatment) patients have severe pain in the epigastric and/or pyloroduodenal region, it is advisable to add ranitidine or famotidine to this therapy for the first 10 days, respectively, 300 mg or 40 mg at night.
- For large ulcers of the stomach or duodenum (1.5-2 cm or more) - the above-mentioned anti-Helicobacter therapy (one of the options in which one of the proton pump inhibitors is proposed as a basic drug, in the other - bismuth tripotassium dicitrate in combination with two antibiotics) is carried out for 10 days, followed by therapy with one of the basic drugs for 3 weeks; after this, it is advisable to carry out the first control endoscopy; If the ulcer does not heal, treatment of patients should be continued with the basic drug for another 4 weeks.
pharmachologic effect
Drugs belonging to the groups of histamine H2 receptor blockers, proton pump inhibitors and M1 - anticholinergic blockers have the ability to reduce the secretion of hydrochloric acid and are the drugs of choice among themselves. This means that one of the drugs in this group is chosen for treatment.
Antacids do not reduce the secretion of hydrochloric acid, but rather neutralize it. They are rarely used to treat gastric ulcers, and sodium bicarbonate is contraindicated in this disease.
Gastroprotectors and prostaglandins help relieve inflammation and heal the ulcer surface.
The complex prescription of these groups of drugs in combination with antibacterial agents leads to the elimination of the pathological process.
Modern approaches to the treatment of gastric and duodenal ulcers
At the end of the twentieth century. A significant step has been taken towards changes in the principles of treatment of peptic ulcer disease (PU). The success of modern approaches to therapy is associated primarily with the use of new antisecretory drugs and Helicobacter pylori (HP) eradication regimens. Currently, pharmacotherapy for ulcer includes more than 500 different drugs and about 1000 combinations of them. The modern concept of treatment of ulcer provides for active therapeutic tactics, including multicomponent drug regimens and long-term use of medications according to indications.
An important component of modern pharmacotherapy for peptic ulcer disease is the absence of fundamental differences in approaches to the treatment of gastric and duodenal ulcers. The basic principles of therapy for peptic ulcer disease are:
- impact on factors of aggression and/or defense;
- etiological therapy;
- correction of drug treatment taking into account concomitant diseases;
- individual characteristics of the patient (age, body weight, tolerance of medications used, activity, i.e. ability to care for oneself);
- financial capabilities of the patient.
- The main directions in the treatment of peptic ulcer disease during exacerbation include:
- etiological treatment;
- treatment regimen;
- therapeutic nutrition;
- drug treatment;
- herbal medicine;
- use of mineral waters;
- physiotherapeutic treatment;
- local treatment of long-term non-healing ulcers.
Currently, in the pathogenesis of ulcers, especially duodenal ulcers, great importance is attached to the infectious agent - H. pylori. Epidemiological data obtained in various countries indicate that 100% of duodenal ulcers and more than 80% of ulcers localized in the stomach are associated with persistent HP.
Many studies confirm that anti-Helicobacter therapy leads to a decrease in the frequency of relapses of gastric ulcer (GUP) and duodenal ulcer (DU). The strategy for treating ulcer using eradication of HP infection has undeniable advantages over therapy with all groups of antiulcer drugs, as it provides long-term remission of the disease and, possibly, complete cure. Anti-Helicobacter therapy has been well studied in accordance with the standards of evidence-based medicine [8]. Modern approaches to the diagnosis and treatment of H. pylori infection, meeting the requirements of evidence-based medicine, are reflected in the final document of the second Maastricht consensus, adopted in September 2000. The main differences between the current document and the agreement five years ago are several important points [5].
- For the first time, the treatment of H. pylori infection, and therefore the diseases associated with it, is the responsibility of a general practitioner, and not a gastroenterologist, as was previously the case. The competence of a gastroenterologist includes only those cases where treatment of the disease, including using second-line therapy, was unsuccessful, as well as cases that clearly require specialist intervention.
- For the first time, two-stage treatment was introduced: when choosing a first-line regimen, the doctor must simultaneously immediately plan reserve therapy.
- It is recommended to use anti-Helicobacter therapy in patients with functional dyspepsia, as well as in cases where long-term therapy with non-steroidal anti-inflammatory drugs is planned.
- Patients with uncomplicated duodenal ulcer are recommended to be prescribed only recommended courses of anti-Helicobacter therapy, without subsequent use of antisecretory drugs.
The main criterion for choosing anti-Helicobacter therapy is its expected effectiveness, providing a high percentage of eradication (more than 80%).
Rules and recommendations of the Russian Gastroenterological Association for the treatment of HP infection for the use of anti-Helicobacter therapy.
- If the treatment regimen used did not achieve eradication, it should not be repeated according to this regimen.
- If the regimen used does not lead to eradication, this means that the bacterium has acquired resistance to one of the components of the treatment regimen.
- If the use of one and then another treatment regimen does not lead to eradication, then the sensitivity of the HP strain to the entire range of antibiotics used should be determined.
The adoption by the Russian Gastroenterological Association in 1998 of national recommendations for the diagnosis and treatment of Helicobacter pylori infection and mass familiarization of doctors with them have not yet led to a decrease in the number of strategic and tactical errors in determining indications for eradication and choosing adequate anti-Helicobacter pylori regimens (see Table 1) [4 ].
Table 1. Errors in the treatment of HP infection.
| Errors in patient selection | Errors in treatment regimens |
|
|
What does a doctor need to know when starting anti-Helicobacter therapy? Every general practitioner, especially those with more than five years of experience, will most likely have to overcome some psychological barrier before prescribing antibiotics to a patient with a peptic ulcer. Today, gastroenterologists and therapists still have different attitudes towards anti-Helicobacter therapy for ulcerative disease. Strict, strict adherence to the anti-Helicobacter treatment regimen is necessary [10]. Their effectiveness has been proven, they correspond to the characteristics of HP and the pharmacokinetics of the drugs, and the side effects of such therapy are also known.
It is better not to carry out anti-Helicobacter therapy at all, rather than to carry it out incorrectly - since in this case, HP resistance to a number of components quickly develops. In this regard, the patient must be told in detail about the upcoming treatment and obtain his consent to cooperate with the doctor. It is also important to assess the patient’s financial capabilities. He should know that, thanks to expensive, one-time treatment, it will be possible to achieve stable remission in patients with duodenal ulcer in 70–80% of cases, and in patients with duodenal ulcer – in 50–60%, which is ultimately cost-effective.
Which eradication scheme to choose? If there is a stomach or duodenal ulcer against the background of increased acid production, then preference should be given to classic three-component regimens based on a proton pump blocker (PPI) (omeprazole, etc.). Then it is possible to switch to a single dose of PPI without antibacterial drugs. You should not use regimens containing nitroimidazoles (metronidazole, tinidazole) if you have a history of drugs from this group being prescribed for other indications.
Currently, in Russia there is a sharp increase in the number of HP strains resistant to nitroimidazoles [2, 9]. Taking this into account, the search for more effective HP eradication regimes seems to be an urgent task today. Therefore, in recent years there has been growing interest in the use of macrolides in the treatment of HP-associated diseases. Numerous studies have shown the effectiveness of using macrolide antibiotics for the treatment of HP. These drugs have a high ability to penetrate cells and are intensively released onto the mucous membranes (MS), which increases their effectiveness against HP. In addition, macrolide antibiotics have fewer contraindications and side effects, and they have a higher eradication rate than tetracyclines, which can also accumulate in cells [11]. The peculiarity of HP infection is that it is accompanied by hyperacidity.
In this regard, most macrolide antibiotics undergo increased hydrolysis and cannot be used. An exception is clarithromycin, which is resistant to hydrochloric acid [11].
Therefore, the purpose of our study was to develop new eradication therapy regimens for duodenal ulcer associated with H. pylori using omeprazole (O), as well as a combination of amoxicillin (A) and clarithromycin (K). We used the following eradication regimen - Ultop (omeprazole) 20 mg twice a day + Fromilid (clarithromycin) 500 mg twice a day + Hiconcil (amoxicillin) 1000 mg twice a day - a course of seven days. Eradication was 90%. The study showed that the use of fromilid (clarithromycin) is effective and advisable in anti-Helicobacter therapy regimens using PPIs.
Data from numerous studies and the results of their meta-analysis allowed us to conclude that the inclusion of antisecretory drugs in HP infection eradication regimens not only improves HP eradication when combined with antibiotics, but also helps accelerate ulcer scarring and allows for faster elimination of the symptoms of ulcerative dyspepsia. As for the specific mechanisms for increasing the effectiveness of eradication due to the use of antisecretory drugs, then, first of all, with an increase in the pH of the gastric contents, the minimum inhibitory concentration of antibiotics (MIC) decreases and their effectiveness accordingly increases. The viscosity of gastric juice and the concentration of the antibiotic in the gastric contents also increase, which increases the exposure time of antibacterial drugs to the bacterium H. pylori [11]. We studied the effectiveness of ultope (omeprazole) - pH > 4 of the gastric contents with a single dose of 20 mg lasted for 12–14 hours (see Figure 1).
However, first-generation PPIs do not fully meet the practical needs of clinicians. They are slowly converted into the active form and create the maximum antisecretory effect for eradication only by the fifth to eighth day of therapy. Drugs in this class also include lansoprazole, pantoprazole, rabeprazole and esomeprazole. They bind to the enzymes of the cell wall of parietal cells - H+, K+ -ATPase, and are the most powerful agents that control gastric acid formation.
Using pH-metry, the effect of a new dosage form of Losek MAPS was studied in HP-negative volunteers. After a course of treatment with this drug, the antisecretory effect
in the daytime was even more pronounced than with the use of pantoprazole [9]. However, pharmaceutical companies, which continued to search for new, more effective antisecretory agents, created a new drug - Nexium. The antisecretory effect of Nexium is superior in severity, speed of onset and duration of action to the similar effect of omeprazole in standard doses of 20 and 40 mg, pantoprazole 40 mg and lansoprazole 30 mg [8].
In connection with the above, a new PPI, Pariet (rabeprazole) is of great interest [3]. In the treatment of peptic ulcer and duodenum, it is recommended to take pariet at a dose of 40 mg once a day or 20 mg every 12 hours. The most effective, fast-acting antisecretory and antibacterial drug in eradication regimens is pariet at a dose of 20 mg twice a day. It does not need to be prescribed seven days before starting antibiotic treatment, as is the case with other PPIs, since a reliable antisecretory effect is achieved already on the first day of treatment (from the recommendations of the Russian Gastroenterological Association).
Unfortunately, the presence of HP resistance to antibiotics in some patients is forcing researchers to develop alternative treatment options for patients suffering from H. pylori-associated peptic ulcer disease.
Thus, we have studied the effectiveness of eradication schemes using reserve antibacterial drugs. The best eradication result (90%) was achieved using the regimen: de-nol 240 mg twice a day, 14 days + tetracycline 1 g/day and furazolidone 200 mg twice a day, seven days.
Quite often the question arises about the need for eradication therapy in elderly and senile people. Today, this can be attributed to the fact that with long-term persistence of HP, intestinal metaplasia and atrophy of the gastric mucosa develop, and the risk of developing gastric carcinoma increases. Age-related characteristics of enzymatic activity and atrophic processes in the gastrointestinal tract also change the rate of biotransformation of drugs and disrupt their absorption. It has been noted that the concentration of ranitidine increases in patients over 60 years of age with concomitant pathology of the hepatopancreatobiliary region [1].
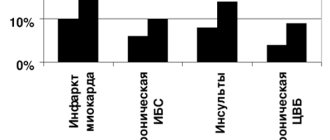
The “Achilles heel” of conservative treatment of peptic ulcer disease is, as is known, the high incidence of complications. It has been proven that HP eradication completely prevents complications of peptic ulcer disease. Thus, in the course of four large studies, the course of peptic ulcer disease was studied in patients in whom it manifested itself with bleeding (see Figure 2). As can be seen from the data presented, any other type of treatment does not exclude the danger of recurrent bleeding - within a year after the previous bleeding, it recurs in approximately every third patient. In the case of HP eradication, bleeding does not recur at all (see Figure 2).
| Figure 2. Rate of recurrent bleeding after a course of eradication therapy. |
Evaluation of the effectiveness of eradication is carried out after completion of treatment and is aimed at identifying vegetative and coccal forms of H. pylori. The “Recommendations” clearly define the scheme for carrying out this diagnostic stage:
- timing - no earlier than four to six weeks after the end of the course of anti-Helicobacter therapy, or after treatment of concomitant diseases with any antibiotics or antisecretory agents;
- diagnosis of eradication is carried out using at least two of these diagnostic methods, and using methods that make it possible to directly detect bacteria in biopsy material (bacteriological, histological, urease). It is necessary to study two biopsy specimens from the body of the stomach and one biopsy specimen from the antrum.
The role of antacid drugs in the treatment of peptic ulcer and duodenal ulcer should not be underestimated. These drugs, known since ancient times, reduce the acidity of gastric juice due to chemical interaction with acid in the stomach cavity. Preference is given to non-absorbable antacids - almagel, maalox, phosphalugel, talcid, rutacid. For exacerbation of peptic ulcer and duodenal ulcer, in complex treatment we used rutacid at a dose of 500 mg three times a day + one tablet before bedtime. While taking this remedy, the symptoms of gastric dyspepsia disappeared
by the end of the first or second day of treatment. Despite the introduction into medical practice of modern inhibitors of gastric secretion, antacids remain important as an effective treatment for patients with gastric ulcers and duodenal ulcers.
As a result of treatment, complete clinical and endoscopic remission should be achieved, with negative results of HP testing.
It should be noted that we very rarely encounter cases where a patient has an isolated ulcer. Treatment of combined pathology is associated with a number of problems.
Sometimes conservative therapy is ineffective. This may be due to two factors: the often recurrent course of peptic ulcer disease and the formation of refractory gastroduodenal ulcers. The analysis revealed the reasons for frequent relapses during ulcerative disease, these are HP infection, taking non-steroidal anti-inflammatory drugs, a history of complications of ulcerative ulcer, as well as low compliance. The factors listed above, as well as the latent Zollinger-Ellison syndrome, may be factors contributing to the formation of refractory gastroduodenal ulcers.
In conclusion, we should once again emphasize the extreme importance of developing domestic standards for the treatment of peptic ulcers and duodenal ulcers and their early implementation in the practice of a general practitioner and gastroenterologist. Important arguments in favor of anti-Helicobacter treatment were obtained when assessing the cost/effectiveness ratio. Peptic ulcer is widespread and characterized by a chronic relapsing course. Eradication of H. pylori reduces both direct and indirect costs of ulcerative disease, eliminating the need for expensive maintenance treatment with antisecretory drugs, reducing the risk of repeated exacerbations, complications and, in some cases, surgical treatment.
Thus, modern drug therapy for duodenal ulcers and gastric ulcers can ensure a relapse-free course of these diseases and relieve patients from complications. In most cases, outpatient treatment is sufficient. The success of therapy depends not only on the prescription of the optimal drug combination, but also, to a large extent, on its implementation with the participation of the patient.
Literature.
- Vertkin A.L., Masharova A.A. Treatment of peptic ulcer disease in a modern clinic // Attending physician, October 2000, No. 8. — P. 14-19.
- Grigoriev P. Ya., Yakovenko E. P., Agafonova A. et al. Pyloric helicobacteriosis: diagnosis, treatment // Attending physician, June 2002, No. 6. — P. 3-8.
- Erashchenko P. P., Snegova E. A., Churilin Yu. Yu. Pharmacoeconomic justification for the use of rabeprazole (Pariet) for peptic ulcer // Clinical pharmacology and therapy, 2001, 10 (1). — P. 42-46.
- Ivashkin V. T. Prevention and treatment of chronic diseases of the upper gastrointestinal tract. - M.: "MEDpress - inform", 2002. - P. 127.
- Isakov V. A, Shcherbakov P. L. Comments on the Maastricht Agreement.” — 2, 2000//V International Symposium “Diagnostics and treatment of diseases associated with H. pylori.”, Pediatrics, No. 2, 2002. — P. 5-7.
- Kokueva O.V., Stepanova L.L., Usova O.A. et al. Pharmacotherapy of peptic ulcer disease taking into account concomitant pathology of the gastrointestinal tract // Experimental and practical gastroenterology, 1/2002. — P. 49-52.
- Koltsov P. A., Zadionchenko V. S. Pharmacotherapy of chronic diseases of the digestive system // Practical guide. - M., 2001. - P. 200.
- Lapina T. L., Ivashkin V. T. Modern approaches to the treatment of gastric and duodenal ulcers // Russian Medical Journal. - T. 3, No. 1, 2001. -
- 10-15.
- Lapina T. L. Modern approaches to the treatment of acid-dependent and H. pylori - associated diseases // Clinical perspectives of gastroenterology and hepatology. 1, 2001. —
- 21-27.
- Pimanov S.I. Esophagitis, gastritis, and peptic ulcer - N. Novgorod, 2000. - 376 p.
- Strachunsky L. S., Kozlov S. N. Macrolides in modern clinical practice. - Smolensk, 1998. - 303 p.
I. V. Mayev , Doctor of Medical Sciences, Professor at MGMSU, Moscow
Basics of therapy and application features
For effective treatment of gastric ulcer it is necessary to adhere to tactics that will allow blocking all known mechanisms of disease development.
The following tactics are usually used:
- Nutrition and diet. Food should be taken 4-5 times a day in small portions. Avoid hot, spicy, overly salty foods. Carbonated drinks and very hot foods are contraindicated.
- Prevention of stress. Relaxation and walks in the fresh air. In some cases, sedatives may be indicated.
- Pharmacotherapy is aimed primarily at reducing the secretion of hydrochloric acid, using healing agents, and destroying Helicobacter pyloricus with antibacterial agents.
The duration of treatment is determined individually by the doctor. The effectiveness of the treatment is assessed by gastroduodenoscopy or x-ray, and the general condition of the patient is also assessed.