Biological therapy has taken a strong position in the treatment of immunoinflammatory diseases. This equally applies to inflammatory bowel diseases (IBD), in particular ulcerative colitis (UC). Among the wide range of biological drugs for the treatment of UC, only one has been registered so far - infliximab (Remicade®). In Russia, Remicade® has been used for UC since 2006, and some experience in its use has already been accumulated, although not as significant as abroad. In real clinical practice, doctors are often afraid to prescribe infliximab, do not have the opportunity to do so, or do not know the indications for its use. Therefore, we considered it appropriate to review in this article a number of fundamental studies assessing the effectiveness of infliximab in UC and share our own experience with the drug.
Goals of treatment for UC: • stopping the attack and inducing remission; • maintaining remission without the use of glucocorticosteroids (GCS); • prevention of complications and operations; • improving the quality of life.
The frequency of steroid-refractory and steroid-dependent forms of UC worldwide is 40–50%; For Russia, exact data is not yet available; for the Moscow region this value is about 40%. Some patients also do not respond to treatment with traditional immunosuppressants (azathioprine and cyclosporine). The most important goals of IBD treatment include overcoming treatment resistance and avoiding corticosteroids in steroid-dependent forms of the disease, maintaining remission without their use. This is what infliximab treatment aims to achieve. Indications for the use of this drug, according to the European Consensus (ECCO), are forms of IBD that are resistant to all types of basic therapy, including steroid dependence and steroid resistance [1]. At the expert council on the development of new standards for the use of infliximab in the EU and the USA, held in October 2005 (UC and CD: Treating to New Standards Expert Round Table), it was proposed to include not only steroid-refractory forms of Crohn's disease and UC in the indications for treatment , but also severe forms of these diseases (as a first-line drug).
Competition "bio/mol/text"-2017
This work was published in the “Biomedicine Today and Tomorrow” category of the “bio/mol/text” competition 2017.
The general sponsor of the competition is: the largest supplier of equipment, reagents and consumables for biological research and production.
The sponsor of the audience award and partner of the “Biomedicine Today and Tomorrow” nomination was.
"Book" sponsor of the competition - "Alpina Non-Fiction"
Systemic rheumatic diseases are pathologies that arise due to the aggressive effects of the immune system on one’s own tissues. Their development is based on an error of the immune system, which incorrectly recognizes the normal components of the human body - autoantigens . Immune cells mistake them for foreign agents, which they see as a threat to the body. The protective function is activated, and healthy cells are “bombarded” by factors of the immune system - autoantibodies (Fig. 1).
The basics of normal immunity and the autoimmune process are presented in an accessible form on “Biomolecule” in the article “Immunity: the fight against strangers and... our own” [1].
Figure 1. Diagram of the structure of antibodies. Antibodies are immunoglobulin proteins that have two H chains (heavy) and two L chains (light). Each protein molecule contains specific Fab fragments . These regions are responsible for binding to the antigen , the “target” that the antibody acts on. The structure of the Fab fragment is very variable, which allows it to adapt to the active centers of the antigen - epitopes . Chemical bonds (ionic, hydrogen, hydrophobic) are formed between the antibody and antigen. The other end of the molecule, the Fc fragment , is responsible for binding the resulting immune complexes to the Fc receptor located on the membranes of immune cells (neutrophils, macrophages, mast cells). Activation of immune components triggers a “killing reaction” against a foreign antigen. Antibody-dependent cytotoxicity occurs in this way.
“Antibodies, structure and functions of immunoglobulins”
The theory of autoimmunity was formulated a century ago by the German researcher Paul Ehrlich. Over the following years, many autoimmune diseases have been described. These include rheumatoid arthritis, systemic lupus erythematosus (SLE), systemic scleroderma, myopathies, vasculitis and other pathologies.
You can read more about the mechanisms of development of some rheumatic diseases in the articles: “Systemic lupus erythematosus: a disease with a thousand faces” [2] and “Rheumatoid arthritis: change the composition of joints” [3].
Diseases associated with an autoimmune component are a serious problem in modern society. Their prevalence in the world population is approximately 5%. Diseases quickly become chronic, which reduces the quality of life of patients. Autoimmune pathologies often lead to disability in patients [1], [4].
In 2021, Biomolecule published a special project dedicated to autoimmune diseases.
Despite many years of searching for new ways of pharmacotherapy, modern medicine cannot offer treatment methods that directly affect the cause of autoimmunity. Doctors can only slow down the progression of the pathology and reduce the severity of the clinic - carry out pathogenetic and symptomatic treatment. For this purpose, basic therapy has been developed and has been used for many years. However, proven drugs do not always work as they should.
Why is it necessary to look for new treatments?
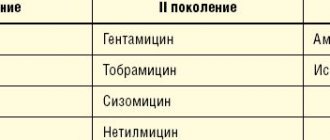
A wide range of antirheumatic drugs are used to treat autoimmune diseases. Classical therapy includes nonsteroidal anti-inflammatory drugs, glucocorticoids, and cytostatics. Depending on the characteristics of the development of the disease, drugs from one or another group are selected [4].
Medicines used for rheumatic diseases
- Major immunosuppressants:
- glucocorticoids (prednisolone, dexamethasone);
- antibiotics (cyclosporine, tacrolimus);
- antimetabolites (methotrexate, azathioprine, mercaptopurine);
- cytostatics (cyclophosphamide).
- Minor immunosuppressants:
- Plaquenil, hingamin;
- cuprenil;
- gold preparations (auronofin);
- heparin;
- non-steroidal anti-inflammatory drugs.
Let's figure out why new drugs are needed. As an example, we can consider the classical therapy of one of the most common autoimmune diseases - rheumatoid arthritis [3]. Modern strategies to combat this pathology must comply with the concept of Treat to target - “treatment until the goal is achieved.” It is aimed at remission (disappearance of symptoms) of the disease or a sharp decrease in the activity of arthritis [5], [6].
The “gold standard” in treating the disease is methotrexate (Fig. 2). The drug belongs to the group of basic anti-inflammatory drugs.
Figure 2. Structural formulas of methotrexate and folic acid. The drug ( a ) is similar in structure to folic acid ( b ). It consists of pteridine groups and para-aminobenzoic acid. The active component of methotrexate differs from the structure of folate in the absence of a hydroxyl group (–OH) and the presence of an additional methyl radical (–CH3).
"Wikipedia"
According to the mechanism of action, methotrexate is an antimetabolite. Drugs in this group inhibit physiological reactions in the body by binding to enzymes and turning off their activity. A substance that normally participates in the reaction can no longer enter the biochemical cycle due to increased competition with the components of the drug. The main target for the action of methotrexate is the enzyme that breaks down folic acid, dihydrofolate reductase ( DHF ). This protein acts on the folate entering the body, converting it into its active form. This produces tetrahydrofolic acid. They are involved in the synthesis of building materials for DNA - purine bases and thymidylate.
Methotrexate enters the chain of reactions due to its structural similarity to the folic acid molecule (Fig. 2). Competition for the enzyme leads to the fact that the content of active folate in the tissue is significantly reduced. There is no building material - there are no new DNA molecules, without which cells cannot reproduce. Those tissues whose structural elements are constantly dividing have increased sensitivity to the effects of the drug. These also include bone marrow components from which future immune cells are formed.
Another important point in the work of methotrexate is related to the activity of its polyglutamated metabolites. These molecules are formed after activation of the drug directly in the cells of the human body. They inhibit other enzymes that interact with folic acid. This group includes thymidyl synthetase and AICAR transamylase. The activity of methotrexate derivatives triggers the production of adenosine. It has a powerful anti-inflammatory effect, which reduces the severity of symptoms of rheumatoid arthritis [7].
Methotrexate is convenient to use - it is easily dosed and can be prescribed in long courses. In addition, an important advantage of this drug is its low price, in comparison with modern drugs from imported pharmaceutical companies [8]. Despite all the advantages, treatment with methotrexate does not always lead to a decrease in disease activity. In many patients, the use of the drug is ineffective even in combination with other classical drugs [5]. This is confirmed by analyzing statistics. Studies have shown that when treated with methotrexate and combinations of disease-modifying drugs, only half of patients achieved remission [9], [10].
The failure of classical therapy forces scientists to look for new ways to treat rheumatoid arthritis. It is worth noting that, despite new developments, the fight against the disease still begins with the prescription of methotrexate and its analogues. Additional drugs are used only when the autoimmune process is highly active. In such patients, the use of one drug is often ineffective [7]. Depending on the characteristics of the pathology, a suitable treatment regimen is selected (Fig. 3).
Figure 3. Management tactics for a patient with rheumatoid arthritis when methotrexate is ineffective.
“Pharmacotherapy of rheumatoid arthritis from the perspective of evidence-based medicine: new recommendations”
The ineffectiveness of basic therapy drugs occurs not only in rheumatoid arthritis, but also in other diseases of autoimmune origin (systemic lupus erythematosus, scleroderma, ankylosing spondylitis). This motivates rheumatology specialists to develop other drugs and select new treatment regimens.
Clinical and economic aspects
Early disease onset, hospitalization, and surgery determine the economic costs of UC. The purpose of the study by RD Cohen et al. (2010) conducted a systematic review of the literature on the cost of managing patients with UC in Western countries. Annual medical costs per patient with UC range from $6200–$11,500 in the United States and €8,900–€10,400 in Europe, with hospitalization costs accounting for 40–55% of total direct medical costs. Indirect costs account for 30% of total costs in the United States and 54–68% in Europe [10].
The ACT I and ACT II studies analyzed the frequency of hospitalizations in patients with UC. A total of 728 people were involved in the two studies, of which 484 patients received Remicade® at different doses (5 and 10 mg/kg/day). The overall rate of hospitalizations within 30 weeks, including readmissions, was half as high in the group receiving Remicade® compared to the standard therapy group (9 vs. 18%). The proportion of hospitalized patients was 8 and 14%, respectively [11]. Since inpatient treatment is the most expensive part of the management of patients with UC; it can be concluded that the use of Remicade provides significant economic benefits for national health care systems.
Genetically engineered drugs: addition to basic therapy
monoclonal antibodies has provided new insight into the treatment of autoimmune diseases [11]. A fundamentally new class of drugs has been obtained thanks to the achievements of genetic engineering. To understand the mechanism of action of these drugs, it is worth remembering how immune cells work in health and disease [1], [12].
The immune system is a complex mechanism consisting of many “cogs” - immune cells. Each of them has its own functions and occupies a certain place in the overall structure of the protective system. In response to the arrival of an “enemy” agent (antigen), components of the innate immune system—nonspecific protective factors—are activated. These are neutrophils, eosinophils and basophils, which are the first to stand in the way of harmful effects.
The cogs turn and new components of the immune system are activated. T- and B-lymphocytes enter the fight against the pathogen. They include more subtle defense mechanisms - specific cytotoxicity. Antibodies are produced, T-killers look for their “victim”... Fine regulation of the process with the help of cytokines allows you to quickly achieve your goal. The coordinated action of all components of immunity leads to the implementation of the program - the destruction of the pathological agent.
During the selection of suitable “parts” for the mechanism - during the selection of lymphocytes - errors inevitably arise. The immune system produces autoreactive clones—cells that are specific to body tissue antigens. Normally, they are eliminated in the “workshops” - the thymus and lymph nodes. Those clones of lymphocytes that do not distinguish between self and foreign antigens are immediately destroyed even before they begin to perform their function. But what happens when the cogs fall out of the immune machine? The breakdown occurs in a specific part of the mechanism - in the work of T- and B-lymphocytes. If the selection process is disrupted, autoreactive cells are released into the blood. They look for their “victims” and find them in the normal elements of their own tissues.
Depending on the type of reaction, the pathophysiological process underlying autoimmune aggression differs. T-lymphocytes can kill body cells on their own, or they can work “by proxy” - activating the production of autoantibodies by B-lymphocytes. When B-cell immunity is damaged, autophagy is realized through the complement system, as well as through the formation of cytotoxic immune complexes [13], [14]. You can read more about the mechanisms of normal and altered immune responses on Biomolecule [1], as well as in articles [15], [16].
In autoimmune diseases, it is possible to suppress the entire complex mechanism of immunity at once, which is what classical therapy drugs do. But this leaves a person without protection from enemy agents - bacterial infections, viruses and other pathogens. Therefore, it is preferable to preserve the activity of the immune system as a whole, saving a person from auto-aggression of certain of its components. This is exactly how new drugs—monoclonal antibodies—work.
Biological agents affect individual “cogs” of the immune defense mechanism. Their targets may be cytokines and their receptors, membrane molecules of lymphocytes. Depending on the point of application of the drug, monoclonal antibodies are divided into groups (Fig. 4):
- TNF (tumor necrosis factor) inhibitors - infliximab, etanercept, certolizumab, golimumab, adalimumab.
- Interleukin receptor blockers - tocilizumab (IL-6R), canakinumab (IL-1R), secukinumab (IL-17R).
- Anti-B-cell antibodies (antibodies to membrane molecules CD20) - rituximab, belimumab [17].
- Anti-T-cell antibodies (antibodies to CD80 and CD86 molecules) - abatacept [18].
Figure 4. Pathophysiological “victims” of monoclonal antibodies - interleukins, TNF, surface proteins of lymphocytes.
“Individualization of treatment for rheumatoid arthritis: a course to achieve optimal results”
TNF inhibitors
Tumor necrosis factor inhibitors are the first monoclonal antibodies introduced into rheumatological practice. This group includes infliximab, etanercept, certolizumab, golimumab, adalimumab.
Tumor necrosis factor ( TNF ) is a pro-inflammatory cytokine (a substance that stimulates the development of an inflammatory response). Normally, when it is released, vascular cell proliferation, macrophage activation, and lysis of tumor agents occur. These effects play an important role in protecting the body from pathogens. Inflammation can be considered a response to damaging factors.
However, the effect of TNF on joints in rheumatic diseases cannot be called positive. Thus, in rheumatoid arthritis, the cytokine stimulates the proliferation of synovial fibroblasts - cells of the joint lining. This leads to the formation of pannus - growths of aggressive tissue. As the disease progresses, the process of inflammation and destruction spreads to the articular cartilage and underlying bones (Fig. 5). The joint tissues are filled with immune cells - macrophages, T- and B-lymphocytes, neutrophils. These mechanisms underlie the development of chronic inflammation. You can refresh your knowledge about the pathogenesis of rheumatoid arthritis in the article “Rheumatoid arthritis: change the composition of the joints” [3].
Figure 5. Pathological changes in the joint in rheumatoid arthritis. The autoimmune process causes erosions, synovitis (inflammation of the synovial membrane), and destruction of articular cartilage.
website krovetvorenie.ru
One of the TNF inhibitors is the drug infliximab. It has "human" and "mouse" areas. Approximately 25% of all amino acids in the monoclonal antibody are derived from mice. This is a Fab fragment - a specific region responsible for binding to TNF. The Fc fragment of the protein is formed from IgG1, a human antibody.
This structure is associated with the mechanism for obtaining the drug. Initially, an antibody to tumor necrosis factor is synthesized in the mouse. The resulting immunoglobulin is specific to TNF and can already neutralize it, but completely foreign proteins, of course, cannot be introduced into the patient’s body. This will cause an active immune reaction - the production of antibodies against therapeutic agents. Therefore, mouse immunoglobulin domains are replaced with similar regions of human proteins. Antibodies that have fragments of different origins are called chimeric. In fact, they take the best qualities of their predecessors. The mouse part provides high sensitivity to TNF, and the human fragments reduce immunogenicity - the likelihood of developing an immune response.
The mechanism of action of infliximab is clear from its structure. The Fab fragment of the molecule binds tumor necrosis factor, forming a stable complex with it. This interaction completely blocks the activity of the cytokine, preventing its connection with the membrane receptors p55 and p57. Infliximab “neutralizes” both soluble and membrane-associated forms of TNF (Fig. 6). The content of other pro-inflammatory factors, such as IL-1, IL-6, and nitrogen monoxide, also decreases in joint cells.
Figure 6. Main effects of TNF and monoclonal antibodies blocking it (infliximab and etanercept). The targets for monoclonal antibodies are free and membrane-associated forms of tumor necrosis factor. The drugs prevent the cytokine from binding to the receptor, thereby reducing the activity of rheumatoid arthritis.
website sportwiki.to
Another effective drug from the group of TNF inhibitors, etanercept, . It contains the extracellular part of the receptor for tumor necrosis factor. It “connects” to human IgG1. The hybrid molecule enters into fierce competition for free TNF and neutralizes it before the cytokine has time to contact receptors and trigger an inflammatory response. An additional effect of etanercept that other TNF inhibitors do not have is the neutralization of lymphotoxin. This substance also belongs to pro-inflammatory cytokines. The production of lymphotoxin stimulates proliferative processes in the joints. Accordingly, blocking its action reduces the activity of inflammation in rheumatological diseases [18].
TNF inhibitors have shown good results not only in the treatment of rheumatoid arthritis, but also in other autoimmune pathologies. For example, new drugs are widely used in patients with ankylosing spondylitis. Slowing the progression of pathology in this case is very important, since auto-aggression is aimed at the joint and bone formations of the spine. Over time, the disease turns the spinal column into a “bamboo stick” - a monolithic, rigid formation. Ankylosis develops gradually, but inevitably. Every year the motor abilities of patients become more and more limited. The use of biological drugs can reduce the activity of inflammation in the spine. This slows down the process of ankylosis formation [19].
Interleukin receptor blockers
Interleukins play an important role in the development of autoimmune inflammation , which, like TNF, are proinflammatory cytokines (Fig. 7). The main representatives of this group are IL-6, IL-1, IL-17. The function of interleukins is the control of the processes of differentiation, proliferation and death (apoptosis) of immune cells, which is carried out through the corresponding target genes [20].
Figure 7. The mechanism of action of interleukins in autoimmune inflammation (using the example of IL-6). The cytokine affects T- and B-lymphocytes, hematopoietic cells, and hepatocytes. It stimulates the production of autoantibodies by B cells, as well as the formation of autoreactive T clones, which are directly involved in the autoimmune process. The effect on the bone marrow is to stimulate the production of new blood cells - the number of leukocytes and platelets increases. Inflammation is accompanied by a response of liver cells, the appearance of characteristic symptoms of an autoimmune disease.
[21]
The influence of interleukins is one of the “triggers” of the inflammatory process. Therefore, blocking their activity improves the condition of patients with autoimmune diseases. You can stop the work of interleukins by binding their receptors - molecules that transmit a signal to immune cells. This is the basis of the mechanism of action of monoclonal antibodies from the group of interleukin receptor inhibitors.
Tocilizumab is a drug that blocks IL-6. The receptor for this substance consists of two components: membrane IL-6R (α chain) and glycoprotein g130 (β chain). The membrane part of the receptor binds to IL-6, forming a stable complex. Together they activate the g130 component, causing a change in its structure (homodimerization). A receptor complex of two g130 molecules is formed, which in turn activates JAK1 kinase. This enzyme triggers a cascade of reactions in the cell, which leads to the appearance of the biological effect of the cytokine - the development of inflammation. In some cases, IL-6 binds not the membrane, but the soluble form of the α-chain (Fig. 8). The mechanism of action of the receptor does not change in this case [21].
Tocilizumab works by competitive inhibition. Signaling molecules actively bind to the monoclonal antibody. The vacant place is filled - interleukin cannot form a complex with the receptor, which means it is not able to activate the inflammation process.
Figure 8. Mechanism of action of tocilizumab. The drug binds soluble and membrane IL-6 receptors, blocking signal transmission.
"Modern targets for targeted therapy of rheumatoid arthritis: from monoclonal antibodies to signal molecule blockers"
Tocilizumab is considered one of the safest drugs in the group of monoclonal antibodies. This allows it to be used for juvenile idiopathic arthritis, which occurs before the age of 16 years. Children react particularly acutely to toxic effects, so the drugs used in their treatment should have a minimum number of adverse reactions. The use of tocilizumab allows one to achieve the desired treatment effect without causing severe complications.
Anti-B cell therapy
One of the main elements involved in autoimmune inflammation are B lymphocytes . They produce autoantibodies that bind to healthy cells in the body. The resulting complex of antibody and autoantigen attacks the complement system or cytotoxic lymphocytes. This process underlies the inflammatory response in rheumatic diseases such as systemic lupus erythematosus. A separate article on “Biomolecule” is devoted to it: “Systemic lupus erythematosus: a disease with a thousand faces” [2].
Anti-B cell therapy drugs ( rituximab and belimumab ) block the activity of B cells by binding to their membrane CD20 molecules. Only certain categories of B cells have these substances. They are specific for pre-B lymphocytes and mature B lymphocytes. CD20 is not present in stem elements and pro-B cells, from which new lymphocytic elements will be formed. Membrane molecules of this type are not found in plasma cells that produce immunoglobulins [22].
Thanks to this feature, the CD20 protein is an ideal “victim” for biological drugs. When its activity is “turned off,” neither the formation of new lymphocytes nor the production of normal antibodies is disrupted. One drug with this mechanism of action is rituximab. The monoclonal antibody binds to the CD20 molecule. This leads to the launch of immunological reactions in relation to B-lymphocytes, which ensure the destruction (lysis) of these cells (Fig. 9).
Figure 9. Mechanism of action of rituximab. The Fab fragment of the monoclonal antibody binds to CD20 on the surface of the B lymphocyte. This triggers cell lysis, which can occur in several ways: through the complement system, the apoptosis program, or the aggression of natural killer cells and macrophages.
"Modern targets for targeted therapy of rheumatoid arthritis: from monoclonal antibodies to signal molecule blockers"
Anti-T cell therapy
Blocking the action of T-lymphocytes is possible due to the peculiarities of their activation. In order for a T lymphocyte to enter the autoimmune process and bind to an antigen, it must receive two signals from antigen presenting cells (APCs). The first signal ensures recognition of a specific autoantigen by T-cell receptors. The second signal is a nonspecific process of binding of membrane molecules CD80 and CD86 on the surface of APC with the CD28 receptor of the lymphocyte. The combination of these interactions causes activation of T cells, which in turn stimulate the production of proinflammatory cytokines. This is the main contribution of T lymphocytes to the autoimmune process.
Knowledge of the mechanism of T cell activation was used in the development of monoclonal antibodies. The main representative of anti-T-cell agents is abatacept . The drug is a protein consisting of two parts. The specific part is formed by the CTLA-4 molecule (cytotoxic lymphocyte antigen 4). The nonspecific region is the Fc fragment of human immunoglobulin G1 [23].
The effect of abatacept is aimed precisely at a nonspecific (costimulatory) signal. The CTLA-4 component binds the CD80 and CD86 proteins on the surface of antigen-presenting cells. The CD28 lymphocyte receptor can no longer interact with them, which is why the activation of the T cell is not completed (Fig. 10).
Figure 10. Mechanism of action of abatacept. Abatacept modulates the immune response through binding to CD80/CD86 on antigen presenting cells. This prevents CD80/CD86 from binding to CD28 T cells, i.e. T cell activation is abolished through blocking costimulation.
"Modern targets for targeted therapy of rheumatoid arthritis: from monoclonal antibodies to signal molecule blockers"
Own experience of using Remicade for UC
The Department of Gastroenterology of MONIKI has experience in using Remicade in patients with IBD: 20 patients with Crohn's disease, 40 with UC, of which 3 patients after subtotal resection of the colon with activity in the stump of the sigmoid and rectum.
The objectives of this study: • to evaluate the effectiveness of an induction course of therapy with infliximab in patients with UC refractory to other treatment methods; • assessment of the possibility of achieving and maintaining clinical and endoscopic remission of UC during infliximab therapy; • maintaining remission of UC without corticosteroids during infliximab therapy.
The objectives of the study were formulated to compare the effectiveness of biological therapy with infliximab in Russia (using the example of a population of patients in the Moscow region), Europe and other countries.
Not everything is so simple: possible problems when using monoclonal antibodies
Monoclonal antibody preparations have been used in rheumatological practice for quite some time. However, they are not prescribed to everyone - not to every first or even every second patient. The main limitation that doctors and patients face is the truly “exorbitant” cost of drugs in this group. Rheumatic diseases cannot be cured in a week or a month - they require many years (or even lifelong) use of therapy. Therefore, when selecting a drug, not only its effectiveness is important, but also its price.
For example, one pack of methotrexate costs approximately 200 rubles. The price of a package of infliximab is about 43 thousand rubles. The difference is obvious. For a year of treatment with methotrexate, even at the maximum dosage, the patient will spend 1–2 thousand rubles on the medicine (depending on the manufacturer, treatment regimen and the cost of the drug in local pharmacies). The price of annual therapy with infliximab is approximately 700 thousand rubles. It is clear that only a very limited group of patients will be able to provide themselves with this medicine.
Therefore, treatment of rheumatic diseases is carried out according to strict algorithms. If a pathology is detected, the patient is prescribed a basic drug. For example, for rheumatoid arthritis, methotrexate will most likely be the main drug. Doctors will add monoclonal antibodies to the standard treatment regimen only in exceptional cases. In Russia, they are considered reserve drugs—additional drugs that should be “left for later,” even despite their high effectiveness. So, if the severity of symptoms does not decrease for a long time (at least 6 months!), a biological drug can be added to methotrexate. Basic therapy is not canceled.
If the disease is initially highly active, progresses rapidly and is accompanied by extra-articular complications, then the patient can immediately be prescribed a combination treatment with basic drugs and monoclonal antibodies. This is due to the fact that biological drugs work best in the “acute period”, when the severity of symptoms is maximum. In addition, the effect of their use is observed faster. Treatment with infliximab produces results within 2–4 weeks, while methotrexate “starts working” only after several months.
The use of biological drugs is permissible in cases where the patient develops intolerance to basic drugs. Patients experience severe side effects from the medication, which further worsens their condition. The use of drugs with a different mechanism of action, including monoclonal antibodies, allows minimizing side effects [18].
The prescription and sale of biological drugs is controlled by the state. Many drugs from the group of monoclonal antibodies (infliximab, etanercept, tocilizumab, golimumab) are included in the “List of Vital and Essential Medicines”. In accordance with it, a list of medications is formed that are supplied to hospitals throughout Russia. Of course, biological drugs are not available in every hospital today. They are usually used in regional centers or specialized hospitals.
If they are unable to provide themselves with medications, patients receive disability and undergo therapy at state expense. This right is enshrined in the current “Program of State Guarantees for the Provision of Free Medical Care.” Treatment with biological drugs is provided for rheumatoid arthritis, ankylosing spondylitis, SLE, dermatopolymyositis, juvenile arthritis and other diseases. At the same time, doctors must determine clear indications for prescribing this or that drug. Getting expensive treatment is quite difficult - you need to undergo a full examination and collect documents. However, the provision of a state quota for many patients is the last chance for a full life.
Another difficulty that can be encountered when using biological drugs is adverse reactions. In parallel with the accumulation of data on the effectiveness of the use of drugs, new undesirable effects from their use are being identified. Most of these reactions are associated with the process of immunosuppression. By suppressing the activity of immune cells, monoclonal antibodies reduce the body's protective function. Anti-infective and anti-tumor immunity are primarily affected [18], [24].
Paradoxically, the use of new drugs against autoimmunity can cause acute autoimmune reactions. All biological drugs are protein molecules that are foreign to the body to one degree or another. Therefore, when therapeutic agents penetrate the patient’s body, the immune system can recognize them as antigens. An active immune response appears - antibodies are produced against the components of the drug.
Autoimmune syndromes provoked by drug administration are usually represented by vasculitis, SLE, antiphospholipid syndrome, and psoriasis [25]. Infliximab, which contains foreign murine fragments, is highly immunogenic. Fully “human” drugs provoke immunity less actively. But even with their use, there is a high risk of developing adverse autoimmune reactions. To eliminate these disorders, it is necessary to adjust the patient’s treatment regimen. It includes additional immunosuppressants that will suppress complications. This may be why combinations of biological drugs with disease-modifying drugs are often more effective than isolated therapy, even with the newest drugs [24].
Despite all possible difficulties, monoclonal antibodies have firmly entered the register of drugs used in rheumatology. The future of biologics and their place in rheumatology will depend on the results of many years of research that remain to be done. But even now we can say that the development of therapeutic monoclonal antibodies is an important step towards defeating autoimmune inflammation.
Material and methods
The open prospective study included 37 unoperated patients with UC who were observed from January 2008 to December 2010. The diagnosis of UC was confirmed endoscopically and histologically. All patients were examined for the presence of latent forms of tuberculosis.
The clinical characteristics of the patients are presented in Table. 2. Steroid resistance developed in 5 patients with the acute form (first attack) of the disease, the remaining 32 patients developed steroid dependence. The initial severity of the UC attack was assessed using the activity index of the Truelove and Witts criteria [12–14]. The effectiveness of therapy was monitored using the Mayo index. Before infliximab therapy, GCS as monotherapy (prednisolone or methylprednisolone) was used in 29 patients. Of these, 5 people with an acute severe form of the disease first received 250–500 mg of methylprednisolone intravenously, followed by a dose reduction and switching to oral prednisolone at the rate of 1 mg/kg body weight per day; 24 patients with another attack of a recurrent form of UC received oral prednisolone at the same dose - 1 mg/kg body weight.
A combination of oral corticosteroids at a dose of 30–40 mg and azathioprine at a dose of 100–150 mg (at least 2 mg/kg) was used in 4 patients with a steroid-dependent continuous form of UC. A combination of azathioprine at the same dose and 5-aminosalicylic acid was administered to 4 patients with a steroid-dependent form of UC and severe side effects of corticosteroids. Thus, before the prescription of Remicade, a total of 33 patients received GCS, and 8 patients received azathioprine AZA.
Patients were prescribed infliximab (Remicade®) according to the DLO program of the Moscow region at the rate of 5 mg/kg body weight per day as an induction course (3 infusions at baseline, 2nd and 6th weeks) and then every 8 weeks. The effectiveness of treatment was monitored using the Mayo index. 35 of 37 patients received an induction course (at least 3 infusions). Its effectiveness was assessed by analogy with AST I and II studies at 8 weeks after the start of treatment (2 weeks after the 3rd infusion). In table Table 3 shows the number of Remicade infusions in the UC patients we observed, up to and including December 2010.
Number of infliximab infusions in patients with UC.
Literature
- Immunity: fight against strangers and... one's own;
- Systemic lupus erythematosus: a disease with a thousand faces;
- Rheumatoid arthritis: change the composition of the joints;
- Nasonov E.L., Alexandrova E.N., Novikov A.A. (2015). Autoimmune rheumatic diseases - problems of immunopathology and personalized therapy. Bulletin of the Russian Academy of Medical Sciences. 2, 169–182;
- Babaeva A.R., Kalinina E.V., Zvonorenko M.S. (2016). New opportunities to improve the effectiveness and safety of treatment of rheumatoid arthritis. Medical alphabet. 22, 5–12;
- Josef S Smolen, Robert Landewé, Ferdinand C Breedveld, Maya Buch, Gerd Burmester, et. al.. (2014). EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis
.
73 , 492-509; - Nasonov E.L. (2015). Methotrexate for rheumatoid arthritis - 2015: new facts and ideas. Scientific and practical rheumatology. 4, 421–433;
- Kanevskaya M.Z. and Gurskaya S.V. (2013). Methotrexate in the treatment of rheumatic diseases. Modern rheumatology. 4, 47–53;
- D. T. Felson, J. S. Smolen, G. Wells, B. Zhang, L. H. D. van Tuyl, et. al.. (2011). American College of Rheumatology/European League Against Rheumatism Provisional Definition of Remission in Rheumatoid Arthritis for Clinical Trials. Annals of the Rheumatic Diseases
.
70 , 404-413; - Patrick Durez, Jacques Malghem, Adrien Nzeusseu Toukap, Geneviève Depresseux, Bernard R. Lauwerys, et. al.. (2007). Treatment of early rheumatoid arthritis: A randomized magnetic resonance imaging study comparing the effects of methotrexate alone, methotrexate in combination with infliximab, and methotrexate in combination with intravenous pulse methylprednisolone. Arthritis Rheum
.
56 , 3919-3927; - Monoclonal antibodies;
- 12 methods in pictures: immunological technologies;
- Autophagy, protophagy and others;
- Nobel Prize in Medicine or Physiology 2021: for self-criticism;
- Zaichik A.M., Poletaev A.B., Churilov L.P. (2013). Recognition of “One’s own” and interaction with “One’s own” as the main form of activity of the adaptive immune system. Bulletin of St. Petersburg State University. Episode 11. Medicine. 1;
- Autoimmunity. Modern views on the physiological and pathological aspects of autoimmunity. NSU Electronic Archive;
- For the first time in half a century, there is a new drug for lupus;
- Nasonov E.L. and Karateev D.E. (2013). The use of genetically engineered biological drugs for the treatment of rheumatoid arthritis: general characteristics (lecture). Scientific and practical rheumatology. 2, 163–169;
- Logvinenko S.I., Shcherban E.A., Pridachina L.S., Pridachina A.N., Maslova Yu.Yu., Kashichkina A.A. (2016). Genetic engineering in the treatment of ankylosing spondylitis (Bechterew's disease). Scientific bulletins of BelSU. Series: Medicine. Pharmacy. 19, 179–182;
- Masahiko Mihara, Misato Hashizume, Hiroto Yoshida, Miho Suzuki, Masashi Shiina. (2012). IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin.
Sci. .
122 , 143-159; - Nasonov E.L., Alexandrova E.N., Avdeeva A.S., Panasyuk E.Yu. (2013). Inhibition of interleukin 6 - new possibilities for pharmacotherapy of immunoinflammatory rheumatic diseases. Scientific and practical rheumatology. 4, 416–427;
- Suponitskaya E.V., Alexandrova E.N., Aleksankin A.P., Nasonov E.L. (2015). The effect of therapy with genetically engineered biological drugs on B-lymphocyte subpopulations in rheumatic diseases: new data. Scientific and practical rheumatology. 1, 78–83;
- Babaeva A.R., Cherevkova E.V., Galchenko O.E., Solodenkova K.S. (2012). Biological agents in the basic therapy of rheumatoid arthritis. Medicinal Bulletin. 7, 3–9;
- Muravyov Yu.V. and Muravyova L.A. (2016). Untimely thoughts on the use of genetically engineered biological drugs for rheumatic diseases. Scientific and practical rheumatology. 3, 361–366;
- Psoriasis: at war with your own skin.