What is pemphigus? Symptoms, causes and treatment
Pemphigus is a chronic autoimmune disease characterized by the appearance of a special type of blisters on the surface of previously healthy skin and mucous membranes. Among the types of pemphigus can be distinguished: vulgar, vegetative, erythematous and foliate.
Pemphigus can be diagnosed if acantholytic cells are detected, which are detected in a smear taken or as part of blisters in the epidermis itself (during histological examination). To treat pemphigus, glucocorticosteroids are first used (a whole course of treatment is prescribed). The latter always goes well with extracorporeal hemocorrection (plasmophoresis, cryoapherosis, hemosorption).
Causes
The reasons for the development of pemphigus have not yet been fully studied. One of the main causes of pemphigus is a violation of autoimmune processes, thereby the cells become antibodies to the immune system.
Violation of cell structure is subject to the influence of external factors, as well as aggressive environmental conditions. As a result, the communication between cells is disrupted, which leads to the formation of bubbles. The incidence rate in people with a hereditary predisposition is much higher.
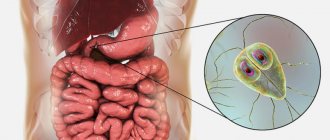
Mechanism of bubble formation
Human skin can be figuratively described as a water-spring “mattress” covered with a kind of “wall”. The “mattress” does not participate in the formation of bubbles - only the top layer, the epidermis, suffers.
The epidermal layer consists of 10-20 cell layers, which look like bricks under a microscope. The “bricks” of the second layer of the epidermis are connected to each other by peculiar “bridges”. On top of the “wall” there are layers of cells that are no longer quite similar to cells, reminiscent of applied cream. These are scales, corneocytes, necessary for protection from mechanical, chemical and physical damage.
If, under the influence of internal or external causes, antibodies are formed that destroy the “bridges” - desmosomes between the cells of the basal layer (this is called acantholysis and can be seen under a microscope), this is true pemphigus. If tissue fluid penetrates between the basal and upper layers of the epidermis without destroying the “bridges,” it is pemphigoid. Viral pemphigus also occurs without destruction of desmosomes.
Spreading
Photo: Pemphigus vulgare
– Advertisement –
The species' range includes the territory of Eurasia and America.
The insectivorous plant bladderwort lives in dark, swampy, tea-colored waters that are rich in tannins.
The ecological criterion for the common bladderwort species is lakes and reservoirs with a low nutrient content.
Botanical description
Utricularia vulgaris or popularly called "water bladder" is a medium-sized perennial aquatic bladder plant with bright yellow summer flowers and no root system. A drawing of Utricularia vulgaris is shown below.
— Advertising —
Pemphigus flower
Depending on the species, they live as epiphytes in a humid atmosphere, moist soil or aquatic environment. The leaves of the bladderwort are up to 16 centimeters in diameter, arranged in a rosette, thinly divided and interspersed with numerous blisters, which darken when eaten by insects. Flowers bloom above the surface of the water in mid-summer. During the transition from autumn to winter, it forms turions (winter buds), which settle to the bottom and help survive the winter.
The diameter of traps on leaves depends on the species and usually reaches 0.6-10 millimeters.
Features of the plant structure
It is a free-floating aquatic plant with “traps” on its leaves formed by membranous sacs or vesicles that are flat, small and pear-shaped. Each vial has a hole covered by a "hanging cap".
The gripping mechanism consists of four stiff bristles located close to the lower free edge of the “lid”. Then, when the insect comes into contact with these bristles, the hairs deform the bottom edge of the lid, causing it to open quickly. The water is “drawn” inside, taking the insect with it, and the lid closes behind it. Subsequently, a number of enzymes secreted by the inner wall of the vesicles and the population of bacteria located in them are digested by the animal.
Pemphigus blooms
Thus, the resulting organic and inorganic compounds are absorbed by the cell walls of the vesicles.
Aside from their strange traps, the common knotweed is also unique in that it has mostly undifferentiated tissue. That is, there is no clear distinction between the leaves, stem and root system.
Classification
Types of non-acantholytic pemphigus:
- Non-acantholytic pemphigus is benign. Pathological elements are formed exclusively in the human oral cavity. Upon examination, inflammation of the mucous membrane, as well as its slight ulceration, can be detected.
- Bullous form of non-acantholytic pemphigus. This is a benign disease that develops in both adults and children. Blisters form on the skin, but there are no signs of acantholysis. These pathological elements can spontaneously disappear without scarring.
- Cicatricial non-acantholytic pemphigus. This pemphigoid is called pemphigus of the eye in the medical literature. Most often it is diagnosed in women who have crossed the 45-year age limit. A characteristic symptom is damage to the visual apparatus, skin and oral mucosa.
Classification of true pemphigus:
- Erythematous form. This pathological process combines several diseases. Its symptoms are similar to seborrheic dermatitis, an erythematous variant of systemic lupus, as well as true pemphigus. Erythematous pemphigus in adults and children is very difficult to treat. It is worth noting that the disease is diagnosed not only in people, but also in some animals. A characteristic symptom is the appearance of red spots on the skin of the body and face, covered with crusts on top. Simultaneously with this symptom, seborrheic manifestations appear on the scalp.
- Pemphigus vulgare. This type of pathology is diagnosed in patients more often. Blisters form on the skin, but there are no signs of inflammation. If pemphigus is not treated on time, pathological elements can spread throughout the entire skin. It is worth noting that they can merge and form large lesions.
- Pemphigus foliaceus. This form received its name due to the characteristics of the pathological elements. Blisters form on the human skin, which practically do not rise above the epidermis (not tense). Crusts form on top of them, which tend to layer on top of each other. The effect of sheet material folded in stacks is created.
- Brazilian pemphigus. There are no restrictions regarding gender and age. Cases of its development have been recorded in both young children and elderly people aged 70 to 80 years. It is also possible that it may progress in middle-aged people. It is worth noting that this variety is endemic and is therefore found only in Brazil.
Pemphigus vulgaris is
Utricularia or water bladder or bladderwort is one of the most diverse and bizarre genera of carnivorous plants. Found on every continent except Antarctica, these carnivorous plants capture prey using a clever bladder trap that sucks up tiny insects and nematodes. These insects make up the majority of their diet.
| Domain (Regio) | Eukaryotes _ |
| Kingdom (Regnum) | Plants (Plantae) |
| Type (Phylum) (division) | Flowering plants (Angiospermae) |
| Class (Сlassis) | Dicotyledons (Dicotyledones) |
| Squad (Ordo) (order) | Lamiales _ |
| Family _ | Bladderworts (Lentibulariaceae) |
| Genus _ | Pemphigus (Utricularia) |
| Species _ | Common bladderwort (Utricularia vulgaris) |
Symptoms
Considering that experts have identified several different types of this pathology, the symptoms of each of them will be very specific. Of course, there are a number of general trends and signs inherent in all types of the disease. This may include, for example, the wave-like course of the pathological process.
Periods of exacerbation alternate with the transition of pemphigus to a calmer stage, when the main symptoms subside or completely disappear. An important factor for the patient will be the fact that in the absence of timely diagnosis and prescription of an effective course of treatment, there is a high risk of developing severe conditions aggravated by concomitant diseases.
- The presence of crusts, ranging from pale pink soft to red dense, reminiscent of lichen;
- There is a deterioration in the general condition;
- Decreased immune response of the body;
- Formation of bubbles of varying densities;
- Also, in severe cases, separation of the layers of the epidermis is noted, and it can occur both in the lesion and away from it.
- Damage and ulcers of the mucous membrane of the mouth, nasopharynx or genitals;
- Pain when performing the act of swallowing or when eating;
- Bad breath, indicating damage to the mucous membranes;
- Hypersalivation or, in other words, increased salivation;
- In the seborrheic form, characteristic yellowish or brown-brown crusts appear on the scalp.
- Bubbles vary in appearance, ranging from flat to thin-walled, which burst with a slight touch. In their place, erosions and, subsequently, crusts form.
- In severe cases, an eroded surface of the skin may form in place of the blisters. Their feature is a tendency towards peripheral growth. Over time, such erosions occupy a large surface of the skin, causing pain and inconvenience to the patient.
- In children, manifestations of pemphigus are localized over the entire surface of the skin, including the limbs.
Experts say that with this disease, both a pure form of the pathological process and mixed forms that smoothly transform into one another can be observed. Therefore, the symptoms and signs of pemphigus in a given person may vary and indicate the presence of several types of disease.
Extracorporeal methods of treating pemphigus
Pemphigus is a severe bullous dermatosis characterized by damage to the skin and/or mucous membranes, the leading role in the pathogenesis of which is played by autoimmune reactions leading to acantholysis. The incidence of pemphigus in the Russian Federation in 2014 was 1.9 cases per 100,000 adults. Trigger factors for the development of pemphigus are most often infectious diseases, as well as the use of drugs and vaccines [1].
A pathogenetic role in the development of pemphigus is played by autoantibodies-immunoglobulins of class G (IgG) to the structural components of desmosomes - desmogleins types 1 and 3 (Dsg1 and Dsg3). A number of studies have published data on the relationship between the level of circulating antibodies to Dsg1 and Dsg3 and clinical forms of pemphigus [2–5].
The mechanisms of development of acantholysis in pemphigus are being actively studied. It has been shown that the development of acantholysis can be caused by activation of intracellular (including apoptotic) signaling pathways, which causes changes in the properties of cell keratin fibrils associated with desmosomes and leads to loss of communication between epithelial cells [6–8].
The goal of treating patients with pemphigus is to stop the appearance of new rashes and epithelization of erosions, as well as to improve the quality of life of patients. Adequate therapy of patients should be carried out from the moment the blisters or erosions appear, even with a limited number of rashes. Despite numerous complications, an indispensable component of the pharmacotherapy of autoimmune dermatoses are systemic glucocorticosteroid (GCS) drugs prescribed for vital indications. In order to reduce high doses of GCS, as well as in steroid-resistant forms of the disease, systemic GCS drugs are prescribed together with adjuvant drugs (cytostatics, extracorporeal therapies, biological drugs). The effectiveness of combination therapy is comparable to the administration of high doses of corticosteroids [9].
It seems relevant to develop pathogenetically substantiated methods of treating patients with pemphigus, which would allow reducing course doses of GCS and other immunosuppressive drugs and reducing the incidence of adverse events in patients. Currently, there is extensive experience of domestic and foreign researchers in the use of extracorporeal therapy methods (extracorporeal photochemotherapy, plasmapheresis and immunoadsorption) for pemphigus [10–12].
Plasmapheresis
The use of plasmapheresis as an adjuvant therapy for pemphigus was first proposed in 1978. Plasmapheresis is used to remove circulating autoantibodies, and the patient's plasma is replaced with fresh donor plasma. The therapeutic effect of plasmapheresis in pemphigus is due to the elimination of circulating IgG and immune complexes that have the ability to adhere to the surface of cells of the spinous layer of the epidermis [13, 14].
During the plasmapheresis procedure, after collecting a portion of the patient’s blood, it is separated into cellular components and plasma using centrifugal centrifugation or double cascade filtration. When carrying out double filtration plasmapheresis, the first filter ensures continuous production of plasma, while the second allows the simultaneous removal of high molecular weight plasma components. After removing the plasma and adding a replacement component to the cellular elements, the treated blood returns to the vascular bed. The plasmapheresis procedure continues until the amount of processed plasma is 1–2 liters [14–16].
The currently recommended therapeutic regimen for plasmapheresis is a course of 6–12 procedures 3 times a week, removing 800–2000 ml of plasma per session. The advisability of using repeated cycles of procedures is explained by the need for a time interval required for the redistribution of autoantibodies between the intercellular and intravascular spaces [16, 17].
One plasmapheresis procedure eliminates about 15% of IgG. Repeated plasmapheresis procedures lead to a temporary decrease in the titer of autoantibodies and even their disappearance, which makes it possible to reduce the dose of immunosuppressive drugs [14, 17].
The effectiveness of plasmapheresis as adjuvant therapy in combination with systemic corticosteroids has been confirmed by the results of many studies. Thus, in a study by R. Tan-Lim et al. a significant decrease in the titers of autoantibodies, pathogenetically significant in the development of pemphigus, was revealed. In a study by K. Sondergaard et al. (1997) showed that the use of long-term combination therapy of glucocorticosteroids in combination with plasmapheresis makes it possible to reduce drug doses and increase the duration of remission in patients. According to a study by M. Gustavo et al. (2003), the use of plasmapheresis in combination with GCS for the treatment of patients with severe treatment-resistant pemphigus allowed us to achieve complete remission in all patients, as well as reduce the dose of prednisolone to 70% [18–20].
At the same time, M. Turner et al. (2002) note that when performing plasmapheresis in combination with systemic corticosteroids, a “rebound” phenomenon can be observed: when autoantibodies are eliminated by a negative feedback mechanism, B-lymphocytes are activated, followed by hyperproduction of autoantibodies, the titers of which may exceed the initial ones. An increase in autoantibody titers, as a rule, occurs one day after the procedure, which may be due to the release of immunoglobulins into the bloodstream from the intercellular space through passive diffusion, since during plasmapheresis the antibodies located in the intravascular space are removed, while the concentration of antibodies in the intercellular fluid remains unchanged. The administration of immunosuppressive therapy immediately after plasmapheresis procedures prevents the production of new autoantibodies, which allows clinical remission to be achieved. In addition, increased activity of B lymphocytes increases their sensitivity to immunosuppressive drugs [14, 17].
Plasmapheresis is recommended for severe pemphigus, in cases of resistance to steroid therapy, in order to reduce the dose of prescribed immunosuppressive drugs, as well as in the presence of contraindications to the use of immunosuppressive drugs. This limitation of indications for the use of this extracorporeal method is explained by the fact that the plasmapheresis procedure does not provide selective elimination of autoantibodies, and therefore it is possible to remove blood clotting factors, hormones, albumin, as well as unchanged IgA, IgM, IgE and immune complexes, which can cause the occurrence of a number of undesirable side effects, including fever, hypotension, dizziness, nausea, anemia, thrombocytopenia, bleeding diathesis, hypocalcemia, cardiac arrhythmias, allergic reactions, pulmonary edema, lower extremity spasms, pneumonia and sepsis [17, 18, 21].
Extracorporeal photochemotherapy (extracorporeal photopheresis)
Extracorporeal photochemotherapy (extracorporeal photopheresis) is a PUVA therapy method that combines leukapheresis and phototherapy. The effectiveness of photopheresis was first proven in 1987 by RL Edelson et al. in the treatment of T-cell lymphomas. Currently, the technique is used in dermatological practice for the treatment of lymphoproliferative and autoimmune diseases, including as adjuvant therapy for acantholytic pemphigus [22, 23].
The mechanism of action of photochemotherapy is based on the initiation of apoptosis of various cell populations. After exposure to ultraviolet irradiation with spectrum A (UV-A) rays, the photosensitizer forms covalent bonds with the pyrimidine bases of leukocyte DNA, which leads to the implementation of the apoptotic pathway. It is assumed that after returning to the bloodstream, transformed leukocytes interact through macrophages and antigen-presenting cells with unchanged B lymphocytes, suppressing their ability to produce autoantibodies, which play a key role in the pathogenesis of pemphigus [23, 24].
During the procedure of extracorporeal photopheresis, outside the patient’s body, leukocytes previously sensitized with photosensitizers are irradiated with ultraviolet rays of spectrum A. After collecting the patient’s blood through a peripheral or central venous catheter, several cycles of leukopheresis are performed, as a result of which the leukocyte mass is separated from other blood components. At the end of each leukopheresis cycle, red blood cells and plasma are returned to the patient's bloodstream, and saline, heparin, and a photosensitizer (eg, 8-methoxypsoralen) are added to the isolated white blood cells. The resulting composition is subjected to UV-A irradiation with a wavelength of 360–420 nm for 30 minutes with an exposure of 1.5–2 J/cm2, after which it is returned to the patient’s bloodstream. The duration of one procedure is about four hours. As an adjuvant therapy for pemphigus, it is recommended to carry out a course of treatment that includes four procedures of extracorporeal photopheresis [23–26].
Indications for the use of extracorporeal photochemotherapy are: severe pemphigus with widespread damage to the skin and mucous membranes, resistance to systemic glucocorticosteroid therapy. The procedure is contraindicated in case of individual intolerance to drugs containing methoxypsoralen, pregnancy, anemia, a history of heparin-induced thrombocytopenia, as well as severe cardiovascular diseases and mental disorders [11].
The use of extracorporeal photopheresis as part of complex therapy can reduce the time of onset of remission, as well as reduce the prescribed doses of systemic corticosteroids and halve the frequency of unwanted side effects and complications associated with drug therapy. Possible side effects include temporary episodes of low blood pressure, tachycardia, anemia, thrombocytopenia and dysfunction of the digestive system [24, 25].
Extracorporeal photochemotherapy is a promising method of adjuvant therapy for pemphigus and requires further in-depth study.
Immunoadsorption
One of the most effective and safe methods of treating autoimmune diseases is the extracorporeal method of therapy using specific immunosorbents. The clinical effectiveness of immunoadsorption in the treatment of pemphigus has been proven in many studies [21].
Immunoadsorption is a more selective method of extracorporeal therapy that allows selective removal of pathogenetically significant antibodies and circulating immune complexes from plasma through the use of highly specific immunosorbents. The method is based on the binding of blood components to immunosorbents with high affinity for these compounds. The main advantages of immunoadsorption compared to plasmapheresis are: 1) more selective removal of autoantibodies from the bloodstream; 2) no need to use plasma replacement components (for example, albumin) or fresh frozen plasma; 3) the ability to process three times the volume of plasma; 4) the phenomenon of post-sorption increased sensitivity of the body to drug therapy, which contributes to a more rapid achievement of clinical remission and allows reducing the doses of corticosteroid drugs and cytostatics [21, 27, 28].
The immunoadsorption procedure involves the creation of an extracorporeal venovenous circuit, which includes an immunosorption column containing a sorbent. After collecting the patient’s blood through a peripheral or central venous catheter and separating cellular elements from the plasma by filtration or centrifugation, the resulting plasma is passed through a column with an immunosorbent, as a result of which circulating immune complexes and IgG, high-affinity to the components of the sorbent, are deposited in the device. The cellular component is then combined with the purified plasma and returned to the patient's bloodstream. During one immunoadsorption procedure, an average of 5–8 liters of blood is processed at a blood flow rate through columns with a sorbent of 40–50 ml/min. The first course of immunoadsorption is carried out daily for 3 days. In the future, it is recommended to conduct about 4 monthly courses [21, 27, 28].
Currently used immunosorbents differ in the sorbent substances included in the column, which determine the adsorption characteristics of the procedure, and depend on the ligand included in the sorbent. Thus, a phenylalanine-based sorbent allows the elimination of 18.3% of IgG, columns with dextran sulfate sodium remove 30% of IgG, and a tryptophan-containing sorbent binds 45–65% of IgG. The molecular mechanisms of action of the listed sorbents are based on the formation of hydrophobic and electrostatic interactions between amino acids and plasma proteins. However, the sorbents presented above have the ability to bind not only immunoglobulins, but also many other plasma proteins [28].
Tryptophan pillars consist of polyvinyl beads cross-linked with alcohol gel, which are immobilized with a hydrophobic amino acid and tryptophan as a ligand. In vitro studies have demonstrated that tryptophan pillars are more effective in removing all classes of pemphigus autoantibodies than dextran pillars, which have the advantage of selectively removing affinity proteins. In addition, tryptophan pillars are cheaper. The disadvantage of this method is that tryptophan pillars absorb blood plasma components necessary for life (fibrinogen, albumin, lipids, all classes of immunoglobulins), and the synthesis of tryptophan pillars is a rather complex process [28].
In a study by M. Luftl et al. (2003) found that the use of an immunoadsorption procedure using a tryptophan-containing sorbent after the first session leads to a decrease in titers of autoantibodies to desmoglein types 1 and 3 by 30% and significantly accelerates the healing of lesions on the skin and mucous membranes, which allows reduce the dose of systemic corticosteroids. Positive long-term results of using immunoadsorption as an adjuvant method of therapy have been demonstrated: 4 weeks after the cycle of procedures, there was a significant decrease in autoantibody titers, a pronounced clinical improvement in the patients’ condition, as well as an increase in the duration of remission to 26 months [28].
Another type of sorbent is an immunosorbent using staphylococcal protein A (protein A affinity resin), which is a recombinant protein A of Staphylococcus aureus immobilized on CNBr-activated sepharose. It has greater selectivity and binds predominantly IgG and immunoglobulin-containing immune complexes, which allows reducing autoantibody titers by 80–90%. Protein A acts as an Fc receptor that binds the Fc fragments of IgG. The advantages of this immunosorbent compared to tryptophan columns are that the method does not require replacement of plasma components [27].
Thus, in a study by E. Schmidt et al. (2003) demonstrated that the use of immunoadsorption using a sorbent based on protein A in combination with methylprednisolone can significantly reduce the titers of pathogenetically significant autoantibodies and achieve clinical remission two weeks after the start of therapy [27].
Immunoadsorption is a relatively safe method of adjuvant therapy, however, some authors have noted isolated side effects - dizziness, bradycardia, decreased blood pressure, paresthesia of the upper limbs and lips, as well as deep vein thrombosis. In addition, in the process of non-selective immunoadsorption, along with pathogenetically significant autoantibodies, IgA, IgM, IgE and immune complexes necessary for the normal functioning of the immune system are also excreted, which leads to an increased risk of developing infectious complications [12, 28].
Conclusion
Although extracorporeal methods are among the most effective as adjuvant therapy for pemphigus, there remains a need for multicenter randomized controlled trials to study their effectiveness and safety.
It seems relevant to develop pathogenetically based methods of treating patients with pemphigus, namely the creation of a highly selective immunosorbent that makes it possible to eliminate antibodies to the structural components of desmosomes from the blood of patients while preserving the immunoglobulins and immune complexes necessary for the body, which would reduce course doses of immunosuppressive drugs and reduce the incidence of adverse events .
Literature
- Kubanova A. A., Kubanov A. A., Melekhina L. E., Bogdanova E. V. Dermatovenereology in the Russian Federation. Results of 2014. Successes, achievements. Main paths of development // Bulletin of dermatology and venereology. 2015. No. 4. pp. 13–26.
- Kubanov A. A., Znamenskaya L. F., Abramova T. V., Svishchenko S. I. On the diagnosis of true acantholytic pemphigus // Bulletin of Dermatology and Venereology. 2014. No. 6. pp. 121–130.
- Delva E., Jennings JM, Calkins CC et al. Pemphigus vulgaris IgG-induced desmoglein-3 endocytosis and esmosomal disassembly are mediated by a clathrin- and dynamin-independent mechanism // J. Biol. Chem. 2008. Vol. 283. R. 18303–18313.
- Matushevskaya E. V., Svirshchevskaya E. V., Dzutseva I. R., Togoeva L. T., Lapshina T. P. Changes in the level of antibodies to desmoglein-3 in the blood serum of patients with pemphigus before and after treatment // Bulletin of Dermatology and venereology. 2005. No. 6. pp. 12–16.
- Herrero-González JE, Iranzo P., Benítez D. et al. Correlation of immunological profile with phenotype and disease outcome in pemphigus // Acta Derm. Venereol. 2010. Vol. 90 (4). P. 401–405.
- Karacheva Yu. V., Gaidash A. A., Prokhorenkov V. I. Study of the relationship between acantholysis and apoptosis in the pathogenesis of pemphigus vulgaris // Bulletin of Dermatology and Venereology. 2014. No. 2. pp. 31–37.
- Kubanov A. A., Katunina O. R., Abramova T. V. Expression of proapoptotic protein in patients with pemphigus // Cytokines and inflammation. 2014. T. 13, no. 4. pp. 31–36.
- Grando SA Apoptolysis: a novel mechanism of skin blistering in pemphigus vulgaris linking the apoptotic pathways to basal cell shrinkage and suprabasal acantholysis // Experimental Dermatology. 2009. Vol. 18. 764–770.
- Kubanov A. A., Abramova T. V. Modern methods of therapy for true acantholytic pemphigus // Bulletin of Dermatology and Venereology. 2014. No. 4. pp. 19–27.
- Atzmony L., Hodak E., Leshem YA et al. The role of adjuvant therapy in pemphigus: A systematic review and meta-analysis // J. Am. Acad. Dermatol. 2015 Aug. Vol 73 (2). P. 264–271.
- Kildyushevsky A.V., Molochkov V.A., Karzanov O.V. Dynamics of cellular immunity during extracorporeal photochemotherapy in patients with true pemphigus // Ross. magazine leather and veins bol. 2008. No. 4. P. 71–76.
- Eming R., Rech J., Barth S. et al. Prolonged clinical remission of patients with severe pemphigus upon rapid removal of desmoglein-reactive autoantibodies by immunoadsorption // Dermatology. 2006. Vol. 212. P. 177–187.
- Cotterill JA, Barker DJ, Millard LG Plasma exchange in the treatment of pemphigus vulgaris // Br. J. Dermatol. 1978. Vol. 98. P. 243.
- Nagasaka T., Fujii Y., Ishida A. et al. Evaluating the efficacy of plasmapheresis for patients with pemphigus using desmoglein enzyme-linked immunosorbent assay // Br. J. Dermatol. 2008. Vol. 158(4). P. 685–690.
- Ranugha P., Kumari R., Kartha LB, Parameswaran S., Thappa DM Therapeutic plasma exchange as a crisis option in severe pemphigus vulgaris // Indian J. Dermatol. Venereol. Leprol. 2012. Vol. 78. P. 508–510.
- Yamada H., Yamaguchi H., Takamori K. et al. Plasmapheresis for the treatment of pemphigus and bullous pemphigoid // Ther. Apher. 1997. Vol. 1. P. 178–182.
- Turner MS, Sutton D, Sauder DN The use of plasmapheresis and immunosuppression in the treatment of pemphigus vulgaris // J. Am. Acad. Dermatol. 2000. Vol. 43. P. 1058–1064.
- Tan-Lim R., Bystryn JC Effect of plasmapheresis therapy on circulating levels of pemphigus antibodies // J. Am. Acad. Dermatol. 1990. Vol. 22. P. 35–40.
- Sondergaard K., Carstens J., Zachariae H. The steroid-sparing effect of long-term plasmapheresis in pemphigus: anupdate // Ther. Apher. 1997. Vol. 1. P. 155–158.
- Mazzi G., Raineri A., Zanolli FA, Ponte CD, Guerra R., Orazi BM et al. Plasmapheresis therapy in pemphigus vulgaris and bullous pemphigoid // Transfusion and Apheresis Science. 2003. Vol. 28. P. 13–18.
- Eming R., Hertl M. Immunoadsorption in pemphigus // Autoimmunity. 2006. Vol. 39. P. 609–616.
- Edelson RL Photopheresis: a new therapeutic concept // Yale. J Biol. Med. 1989. Vol. 62. P. 565–577.
- Pérez-Carmona L., Harto-Castaño A., Díez-Recio E., Jaén-Olasolo P. Extracorporeal Photopheresis in Dermatology // Actas Dermosifiliogr. 2009. Vol. 100 (6). P. 459–471.
- Knobler R., Berlin G., Calzavara-Pinton P., Greinix H., Jaksch P., Laroche L. et al. Guidelines on the use of extracorporeal photopheresis // J. Eur. Acad. Dermatol. Venereol. 2014 Jan. Vol. 28 (1). P. 1–37.
- Wollina U., Lange D., Looks A. Short-time extracorporeal photochemotherapy in the treatment of drug-resistant autoimmune bullous diseases // Dermatology. 1999. Vol. 198. P. 140–144.
- Kildyushevsky A.V., Karzanov O.V. // Almanac of Clinical Medicine. M., 2006. T. 9. pp. 39–44.
- Schmidt E., Klinker E., Opitz A. et al. Protein A immunoadsorption: a novel and effective adjuvant treatment of severe pemphigus // Br. J. Dermatol. 2003. Vol. 148. P. 1222–1229.
- Luftl M., Stauber A., Mainka A. et al. Successful removal of pathogenic autoantibodies in pemphigus by immunoadsorption with a tryptophan-linked polyvinylalcoholadsorber // Br. J. Dermatol. 2003. Vol. 149. P. 598–605.
A. A. Kubanov, Doctor of Medical Sciences, Professor, Corresponding Member of the Russian Academy of Sciences T. V. Abramova1, Candidate of Medical Sciences E. K. Murakhovskaya, Candidate of Medical Sciences A. V. Asoskova
Federal State Budgetary Educational Institution of Further Professional Education RMAPO Ministry of Health of the Russian Federation, Moscow
1 Contact information
Diagnostics
Experts say that a correct diagnosis can be made based on a comprehensive examination of the patient, which includes several important stages:
- Examination of the patient for the presence of a clinical picture. At this point, the doctor establishes the nature of the lesions, their localization, the degree of development of the disease, etc.
- Cytological analysis necessary to establish the presence of acantholic cells in smears of biomaterial.
- Carrying out the Nikolsky test, which allows to differentiate pemphigus from similar pathological processes.
- Method of direct immunofluorescence. This study allows us to detect the presence of immunoglobulin in the intercellular substance of the epidermis.
- A histological study, which is based on a technique for detecting crevices and other damage within the epidermis.
Only the totality of all the results makes it possible to make an accurate diagnosis and prescribe an effective course of treatment, leading to the patient’s recovery.
Treatment of viral pemphigus
Treatment of viral pemphigus involves the use of the following systemic drugs:
- cytostatics stop the division of immune cells: Sandimmune, Azathioprine, Methotrexate;
- antiviral: Viferon, Laferon, Cycloferon;
- glucocorticosteroids: Dexamethasone, Prednisolone;
- antipyretics: Ibuprofen, Paracetamol, Nimesil, Mefenamic acid;
- antihistamines relieve itching: Cetrin, Diazolin, Fenistil.
For external treatment of affected skin areas, the following may be prescribed:
- antimicrobial local anesthetics for irrigating the oral cavity if viral pemphigus has affected the child’s mucous membranes: Forteza, Orasept;
- antiseptics: Chlorhexidine, Methylene blue, Miramistin;
- combination preparations of antiseptics and anesthetics: Oflokain, pharmaceutical talkers;
- antipruritic lotions made from nettle juice, aloe, and walnut oil.
Since children with this diagnosis are usually treated in a hospital setting, to enhance the therapeutic course, therapeutic procedures can be carried out aimed at clearing the blood of antibodies:
- plasmapheresis - replacement of the liquid part of the blood with similar solutions without microbes, immune complexes and antibodies;
- hemosorption using a carbon filter.
Only a doctor can tell how to treat viral pemphigus, because in each individual case it can acquire some special features. As for other forms of pemphigus, the therapeutic course for them is also determined individually.
Treatment
How to treat pemphigus in a child? The main drugs today are hormones from the group of glucosteroids. In this case, systemic therapy is carried out without age restrictions.
Treatment of pemphigus has several main directions:
- preventing the appearance of new blisters and erosions;
- healing of affected areas of the skin.
Glucosteroids are administered in increased dosages. Due to this technique, the intensity of the formation of new foci decreases and the restoration process begins in existing erosions. This process takes about 2 weeks. Subsequently, the patient is transferred to maintenance hormonal therapy. The drug does not change, but the dosage is significantly reduced.
Viral pemphigus in children treatment is aimed at suppressing the virus. Pemphigus vulgaris requires the administration of a larger volume of drugs than foliaceus. The transition to maintenance therapy is carried out gradually. Moreover, the vast majority of patients are forced to take daily injections of maintenance doses of glucosteroid drugs throughout their lives.
Children should take hormonal medications simultaneously with calcium and vitamin D. The effectiveness of treatment increases due to the use of immunosuppressive drugs from the first days of treatment. These drugs have a depressing effect on the activity of the body's immune system.
Early stages of treatment often involve the use of procedures aimed at clearing the blood of aggressive antibodies. Such procedures include hemodialysis and plasmapheresis. The skin must be treated with antiseptics and special ointments to reduce the risk of infection.
Treatment of pathology is daily and lifelong. Sometimes there may be breaks between relapses of the disease.
Baby care
The diagnosis of pemphigus requires special, attentive and daily care for the child. The organization of a baby’s life directly affects his life expectancy. The initial stage of treatment takes place within the walls of the hospital. After discharge, the child should receive all necessary medications in the prescribed volume and time of administration. Parents must learn how to give injections, because the daily services of a hired nurse will negatively affect the family budget.
Every day your child needs to treat blisters and eczema on the skin. Processing is carried out using aniline dyes. This group of agents has the widest spectrum of action on various microbes, including staphylococcus. Erosion and crusts formed are treated with corticosteroid-based ointments.
The presence of infectious signs in the form of pus, inflammation, swelling means the start of using antibiotic ointments. Large affected areas require the use of sterile dressings to help avoid further injury. Dressings are changed at least 2 times a day. For small affected areas, the relevance of bandages is associated with the child’s high motor activity.
The appearance of pain requires taking painkillers and consulting a specialist. The presence of damaged areas in the oral cavity is associated with mandatory rinsing of the mouth with antiseptic agents. A useful and effective means of care is taking baths with antiseptic agents. It is mandatory to take vitamin and mineral complexes consisting of vitamin E, calcium, magnesium and folic acid.
The diet also requires enrichment with vitamins and minerals. Meals are provided on a fractional and frequent basis, at least 6 times a day. This diet plan is especially important when the esophagus and mucous membranes in the mouth are affected. Diet therapy is based on the complete exclusion of salt and increasing the amount of protein. Registration at a dispensary and systematic visits to a dermatologist are required - at least twice a year and urgently in case of relapse. The use of immunosuppressive therapy imposes restrictions on vaccinations.
How to treat other forms of pemphigus?
The treatment process for pemphigus is quite complicated. Therefore, self-medication of this type of disease is under no circumstances acceptable. The disease progresses rapidly, affecting large areas of the skin, which leads to disruption of the internal organs.
Treatment of pemphigus is mandatory in a dermatological hospital. First of all, corticosteroid drugs, cytostatics and other drugs are prescribed to alleviate the course of the disease and the life expectancy of patients.
The drugs must first be taken in large doses. At the same time, pay attention to blood and urine sugar levels, monitor blood pressure and observe personal hygiene rules. With frequent changes of bed linen and underwear, secondary infection is prevented.
Medicines for the treatment of pemphigus
The patient is advised to take glucocorticoids in high doses. The following drugs can be used for this:
- Metipred;
- Prednisolone;
- Dexamethasone;
- Polcortolon.
When symptoms begin to regress, the doses of these drugs are gradually reduced to the minimum effective. Patients with pathologies of the gastrointestinal tract are prescribed long-acting glucocorticoids:
- Metipred-depot;
- Diprospan;
- Depo-Medrol.
Treatment with hormonal drugs can cause a number of complications, but they are not a reason to discontinue corticosteroids. This is explained by the fact that refusal to take them can lead to relapses and progression of pemphigus.
Possible complications during treatment:
- acute psychosis;
- arterial hypertension;
- depressive states;
- insomnia;
- increased excitability of the nervous system;
- steroid diabetes;
- thrombosis;
- obesity;
- angiopathy;
- erosions or ulcers of the stomach and/or intestines.
If the patient’s condition sharply worsens while taking corticosteroids, the following measures may be recommended:
- diet: limiting fats, carbohydrates and table salt, introducing more protein and vitamins into the diet;
- drugs to protect the gastric mucosa: Almagel, etc.
In parallel with glucocorticoids, cytostatics and immunosuppressants are prescribed to increase the effectiveness of therapy and the possibility of reducing doses of hormonal agents.
The following medications can be used for this:
- Sandimmune;
- Methotrexate;
- Azathioprine.
To prevent electrolyte imbalance, the patient is recommended to take calcium and potassium supplements. And for secondary infection of erosions - antibiotics or antifungal agents.
The ultimate goal of drug therapy is to make the rash disappear.
Preventive measures
There are no specific measures to prevent the development of pathology. The higher the level of immune protection, the less chance of dermatological diseases.
Important:
- control the nature of chronic diseases;
- strengthen immunity;
- maintain personal hygiene;
- Healthy food.
Measures to prevent pemphigus in newborns:
- change your underwear more often;
- Caring for newborns with pustular skin lesions is prohibited;
- Take regular care of your child’s skin;
- strengthen the immune system of weakened children;
- daily wet cleaning and ventilation of the room are required.
If you notice any rashes on the skin, the formation of pustules and blisters, immediately contact a dermatologist.
Forecast
The prognosis for acantholytic pemphigus is conditionally unfavorable. On the one hand, in the absence of effective treatment, there is a high probability of complications and death.
On the other hand, patients with pemphigus are forced to take glucocorticosteroids for a long time, and sometimes for life, which is fraught with the development of side effects. But hasty refusal of drugs leads to immediate relapse of the disease. Glucocorticosteroids do not eliminate the cause of the disease, but inhibit the pathological process and prevent its progression.
2. Reasons
As stated above, the etiopathogenesis of acantholytic pemphigus has not yet been precisely established.
Various hypotheses have been put forward and considered in this regard (viral, metabolic, neurogenic, toxic, hormonal, etc.), but convincing evidence has been obtained only that autoimmune mechanisms play a leading role in the development of pemphigus. However, the root causes of such an attack from one's own immunity, trigger factors and risk factors (with the exception of being female or belonging to a certain genetic line) are still unknown.
Visit our Dermatology page