- Outpatient department
Outpatient department » - Gastroenterology
Gastroenterology »
- About the direction
About the direction »
- Gastritis: symptoms, diagnosis and treatment
Gastritis is perhaps the most common disease of the gastrointestinal tract. Almost every second resident of our country suffers from it. That is why it is so important to know the first signs and symptoms of this disease in order to start treatment on time and not neglect your health.
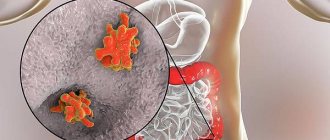
Gastritis (from the Latin gastritis, from the ancient Greek γαστήρ (gaster) - “stomach” + -itis inflammatory or inflammatory-dystrophic changes in the mucous membrane) is a collective concept that is used to refer to various inflammatory and dystrophic changes in the gastric mucosa. Damage to the mucous membrane can be primary, considered as an independent disease, caused by poor nutrition, and secondary, caused by other infectious and non-infectious diseases or intoxication.
Types of gastritis
The largest division of gastritis is acute and chronic. The first occurs immediately after irritating factors come into contact with the gastric mucosa. In case of improper nutrition, it manifests itself in a catarrhal form, in case of poisoning or infection - in a fibrinous form.
Chronic is often caused by the bacterium Helicobacter pylori. The disease is characterized by a sluggish course with periodic exacerbations. Based on the localization of the inflammatory process, the following forms are distinguished:
- antrum - in the lower part of the stomach;
- fundal - in the middle section (sometimes extends to the bottom of the organ);
- reflux gastritis - in the area of the pylorus of the stomach.
The chronic type of the disease is characterized by dysfunction of gastric secretion. Its excessive activity causes increased acidity (this form is called hyperacid). With secretory insufficiency, acidity is reduced (this form is called anacid).
Gastritis is a group of diseases whose common feature is inflammation of the gastric mucosa.
This is most often due to an infection caused by the bacterium Helicobacter pylori, which also causes stomach ulcers. Alcohol abuse or long-term use of painkillers can contribute to the development of gastritis.
Gastritis can occur suddenly and resolve quickly (acute gastritis) or develop gradually and persist for a long time (chronic gastritis). In rare cases, it leads to ulcers and is a factor that increases the risk of stomach cancer. However, it is usually asymptomatic and does not require treatment.
Synonyms Russian
Acute gastritis, chronic gastritis.
English synonyms
Chronic gastritis, acute gastritis.
Symptoms
Chronic gastritis is most often asymptomatic, but sometimes it manifests itself as follows:
- pain or discomfort in the upper abdomen,
- nausea, vomiting,
- burning or aching pain in the upper abdomen, heaviness, bloating,
- feeling of fullness in the abdomen, rapid satiety.
In most cases, these symptoms should be regarded as manifestations of functional dyspepsia in the absence of organic diseases of the gastrointestinal tract.
Acute gastritis is usually accompanied by severe abdominal pain, nausea and vomiting.
General information about the disease
Gastritis is a group of diseases whose common feature is inflammation of the gastric mucosa.
The stomach is an organ in the form of a muscular sac located in the upper abdomen behind the lower ribs. It serves as a “reservoir” for incoming food and produces juice for its digestion.
Gastritis occurs when there is an imbalance between the effects of hydrochloric acid and mucosal protective factors. This occurs due to various reasons: the presence of bacteria and the toxins they produce, alcohol intake, painkillers. As a result, inflammation of the gastric mucosa develops.
Gastritis can be acute or chronic.
1. Acute gastritis is a rapidly developing inflammation that resolves over a short period of time. Most often it is caused by infection with the bacterium Helicobacter pylori and is asymptomatic, sometimes becoming chronic.
Also a common cause of acute gastritis is the consumption of large amounts of alcohol, abuse of painkillers (aspirin, ibuprofen, etc.).
2. Chronic gastritis develops gradually. It affects about 80-90% of the adult population.
Chronic gastritis is characterized by inflammation of the gastric mucosa at the cellular level, which can only be determined under a microscope. Over time, the mucous membrane becomes thinner (atrophies), as a result of which the production of gastric juice decreases.
There are two main forms of chronic gastritis.
1. Gastritis caused by the bacterium Helicobacter pylori (95% of all cases of chronic gastritis). Once in the stomach, it contributes to the development of chronic inflammation, eventually leading to thinning of the mucous membrane. However, for most people, the Helicobacter bacteria does not cause any symptoms.
2. Autoimmune gastritis. Its development is associated with autoimmune mechanisms. In this case, the body produces antibodies to its own cells of the gastric mucosa, which leads to their damage. As a result, the production of hydrochloric acid decreases and the gastric mucosa becomes thinner.
In a healthy body, the gastric mucosa produces a protein necessary for the absorption of vitamin B12, which plays an important role in the formation of red blood cells. With a lack of B12, B12 deficiency anemia develops.
Autoimmune gastritis develops very slowly and is usually detected in old age.
Who is at risk?
- More than half of the world's population is infected with the bacterium Helicobacter pylori.
It should be noted that this bacterium is only one of the causes of gastritis; additional factors are often decisive: smoking, drinking alcohol, painkillers.
- Those who regularly use painkillers: aspirin, analgin, Nise, ibuprofen, etc.
- Alcohol abusers.
- Those who have suffered severe stress, for example, after operations, injuries, burns and severe infections.
- Patients with autoimmune diseases such as B12 deficiency anemia, inflammatory bowel disease, autoimmune thyroiditis.
Diagnostics
The diagnosis of “chronic gastritis” can only be made based on the results of examining a piece of the gastric mucosa under a microscope.
Since the most common cause of gastritis is the bacterium Helicobacter pylori, its presence in the body is first determined.
Detection of Helicobacter pylori infection
- Helicobacter pylori, IgA, Helicobacter pylori, IgG – detection of antibodies to this bacterium. The results of this study are highly reliable, but it is not used to evaluate the effectiveness of treatment, since antibodies to Helicobacter pylori persist for a long time after getting rid of it.
- Helicobacter pylori, DNA, – determination of bacterial DNA in stool.
- Breath urease test. This test is highly sensitive and specific. Helicobacter pylori produces a lot of urease (a special enzyme) during its life. During the test, the subject drinks a liquid containing radioactive carbon. Helicobacter breaks down the substances contained in the liquid, forming carbon dioxide exhaled by a person. Accordingly, the presence of labeled carbon in exhaled carbon dioxide indicates that a person is infected with the Helicobacter bacterium.
A negative test result for Helicobacter may indicate that the person is not infected. If additional symptoms occur, endoscopy is prescribed.
- Endoscopy (FGDS - fibrogastroduodenoscopy). A hollow tube equipped with a lens is inserted through the esophagus into the stomach. During FGDS, a biopsy is performed - taking pieces of tissue from the gastric mucosa for subsequent study, during which Helicobacter can be identified, in addition, the nature of inflammation and the type of gastritis can be determined.
Tests confirming the diagnosis of autoimmune gastritis
- General blood analysis. For gastritis caused by Helicobacter pylori, changes in the general blood test are not typical. With autoimmune gastritis associated with B12-deficiency anemia, the hemoglobin level may be reduced, the mean erythrocyte volume (MCV) may be increased, and the hemoglobin content in the erythrocyte (MCI) may be increased.
- Pepsinogen I, pepsinogen II. Pepsinogen is produced by cells of the gastric mucosa. A decrease in its level indicates atrophy (thinning) of the gastric mucosa, which is typical for advanced cases of chronic gastritis.
- Gastrin is a hormone produced by stomach cells to stimulate the production of gastric juice by mucosal cells. With autoimmune gastritis, its concentration increases significantly.
- Antibodies to gastric parietal cells. In autoimmune diseases, antibodies to parietal cells damage the gastric mucosa. Their level almost always increases in autoimmune gastritis.
- Vitamin B12. Reduced levels of vitamin B12 in the blood indicate B12 deficiency anemia associated with autoimmune gastritis.
- Endoscopy (FGDS) with biopsy. When examining cells of the gastric mucosa under a microscope, changes characteristic of chronic autoimmune gastritis are revealed.
Treatment
Treatment for gastritis depends on its cause.
In case of acute gastritis caused by abuse of alcohol or painkillers, you must stop taking them.
Chronic gastritis caused by the Helicobacter bacterium is cured by destroying the bacterium in cases where:
- there are symptoms of the disease that cause discomfort,
- there is a hereditary predisposition to developing stomach cancer,
- the patient is forced to regularly take painkillers and anti-inflammatory drugs.
The bacterium is destroyed by a course of antibiotics within 10-14 days. To assess the success of therapy, a repeat test for the Helicobacter bacterium is necessary.
In most cases, treatment for gastritis also involves taking medications that reduce the production of hydrochloric acid and promote healing of the stomach lining.
Prevention
At the moment, no methods have been developed to prevent gastritis.
Recommended tests
- General blood analysis
- Helicobacter pylori, IgA (quantitative)
- Helicobacter pylori, IgG (quantitative)
- Helicobacter pylori, DNA [real-time PCR] (feces)
- Pepsinogen I
- Pepsinogen II
- Gastrin
- Antibodies to gastric parietal cells
- Vitamin B12 (cyanocobalamin)
Types of damage to the mucous membrane
Gastritis can also be classified according to the degree of change in the gastric mucosa. The mildest form is superficial, when the inflammatory process affects only the upper part of the mucosa. More dangerous forms include the following:
Although hyperplastic gastritis is characterized by the appearance of neoplasms, they are predominantly benign.
The atrophic form often leads to stomach cancer. Each of these types can be focal or diffuse: the first covers a small area of the mucous membrane (although there may be several of them), the second spreads over its entire surface.
Digestive processes in the human body
Our stomach is the most vulnerable organ of the digestive system. The most important and complex digestive processes take place in it:
- Mixing of food occurs in the stomach - this is a mechanical process.
- Next, the breakdown of food occurs there - this is a chemical process.
- And absorption of nutrients. If at least one of these processes goes wrong, the entire digestive system suffers, and all further stages of its work are disrupted.
Most often, the inner wall of the stomach is damaged, its mucous membrane, where the production of the most important components of digestion occurs - gastric juice and protective mucus.
Types of gastritis by etiology
The mucous membrane of the stomach can become inflamed for various reasons. Gastroenterologists, according to this criterion, divide diseases into several groups:
There are also mixed types. Thus, AC inflammation means that reflux is caused by autoimmune factors. It happens that autoimmune effects are combined with Helicobacter pylori infection. Then we are talking about AB gastritis.
Causes of acute gastritis
This disease appears suddenly. In rare cases, the cause may be the bacteria Helicobacter pylori entering the body. But usually it does not make itself felt instantly, but is the causative agent of sluggish chronic gastritis.
It is usually not difficult for an adult to determine the cause. It is enough to analyze what he ate and drank several hours before the attack. Inflammation can be caused by:
Infections can also cause an attack. Among the most likely, gastroenterologists identify cytomegaloverus, syphilis, and staphylococcus infection. People with weakened immune systems are more likely to become infected. Another reason for the development of an acute inflammatory process is exposure to bile. This only applies to type C gastritis.
Forms and stages of gastritis
Inflammatory processes in the mucous tissues of the stomach develop gradually. In the initial stages, gastritis can be practically asymptomatic. But sooner or later the disease makes itself felt and becomes acute.
Acute gastritis is characterized by a sharp deterioration in health, the appearance of acute pain and heaviness in the stomach. Often, an exacerbation can be triggered by some irritant, for example, after taking medications, spicy food, alcohol, etc.
If acute gastritis is not treated in time, the disease may progress to the next stage. Chronic gastritis develops in 85% of cases. Periods of remission are followed by exacerbations of the disease, which in the future can lead to such serious consequences as gastric ulcers or even oncology.
Causes of development of chronic gastritis
The second most important cause of chronic inflammation of the gastric mucosa (after the bacterium Helicobacter pylori) is poor nutrition. This includes not only harmful products. Violation of the eating schedule is also detrimental to the stomach. Inflammation can result from:
The influence of other diseases (endocrine, metabolic, infectious, hypoxic) cannot be excluded. External factors (harmful working conditions, stress) also become causes of gastritis.
What bad habits can cause gastritis?
The most common cause of gastritis is the habit of eating poorly and chewing food poorly. Poor nutrition should be understood as: drinking coffee and sweets on an empty stomach, non-compliance with the diet, abuse of smoked, fatty and spicy foods. Surely you have noticed that if you chew your food poorly and quickly “push it down” (seemingly full), then this is self-deception. Then, of course, there will be a feeling of discomfort in the stomach, pain, etc.
General signs of gastritis
Regardless of the type (acute or chronic), it always manifests itself as pain in the epigastric region (only its nature differs). Pain appears after eating or, conversely, from hunger. Other symptoms from the digestive system are possible:
Symptoms in adults are more severe than in children. In children, attacks are often accompanied by weakness, fever, and bruises under the eyes. Parents may confuse the first signs of gastritis with poisoning.
Another noticeable symptom of many types of this disease is a white (less often yellow) coating on the tongue. It is not cleaned during normal hygiene procedures. In most cases, plaque indicates a decrease in acidity.
When to see a doctor
You should consult a doctor if you feel severe pain with gastritis of the stomach, since exacerbation of gastritis can cause a serious deterioration in health with an increase in the area of mucosal damage and transition to an ulcerative state. Gastritis is especially dangerous if there is increased acidity, since the juice tends to corrode the mucous membrane of the organ, resulting in the formation of ulcers. If, based on a number of signs, the patient has identified an exacerbation of gastritis, the symptoms of which are nausea to vomiting, complete loss of appetite, fever up to 39 degrees Celsius and severe pain, you should make an appointment with a specialist as quickly as possible.
Gastritis, the symptoms and treatment of which may vary in adults, is diagnosed by a gastroenterologist. The Center for Modern Medicine JSC "Medicine" (academician Roitberg's clinic) in Moscow offers diagnostic and treatment services for all types of gastritis using modern medical devices and drugs. More complete information on the topic “gastritis and its treatment in adults” can be obtained by clicking on the link. Our clinic is located at 2nd Tverskoy-Yamskaya Lane, building 10, a 5-minute walk from the Mayakovskaya metro station.
How to treat the disease
Since there are many types of gastritis, and each of them has its own causes, you cannot limit yourself to one treatment method. To combat each provoking factor, appropriate drugs are needed.
The doctor must determine by characteristic signs whether the patient’s acidity is increased or decreased. Depending on this, a suitable treatment regimen is selected.
Treatment of gastritis is usually complex, it is carried out in the following areas:
If the bacterium Helicobacter pylori is detected, it is important to eradicate it (complete destruction) with antibiotics. This is necessary to eliminate ulcerations, accelerate their healing and prevent the development of peptic ulcers and stomach cancer.
Innovation
Scientists have begun searching for substances that are less traumatic for the body and effective in combating Helicobacter.
And in the course of numerous studies, it turned out that a pronounced positive effect is observed when taking certain beneficial bacteria. Among the numerous beneficial bacteria that have a positive effect on the microflora of the stomach and intestines, there are those that also fight “bad” bacteria, in particular Helicobacter. They have also been shown to increase the effectiveness of drug therapy in the treatment of gastritis and reduce the side effects of taking antibiotics.
The search for truly effective and safe remedies against Helicobacter took many years.
How is acidity level determined?
The main acid found in the stomach and determining its acidity level is hydrochloric acid. It is produced by parietal cells. The alkaline components of gastric juice neutralize hydrochloric acid. They are produced by accessory cells of the mucosa. The two substances interact and the acidity level changes throughout the day.
You can find out its level using intragastric pH-metry. To do this, a thin probe with a measuring electrode is placed into the patient's stomach. It gradually moves deeper and shows the pH in different areas of the organ.
In the part of the stomach where acid is produced, in an adult patient the pH should be from 1.6 to 2.0, and in the zone of alkali production and acid quenching - up to 5.2.
The doctor also pays attention to the symptoms. With high acidity, the patient suffers from heartburn, belching and a burning sensation in the throat; with low acidity, the patient suffers from bloating, flatulence and bad breath.
Diagnostics
Diagnosis of chronic gastritis includes the following stages: -external examination and medical history; -study; -gastroscopy (endoscopic diagnostics); - laboratory tests of blood and gastric juice. When interviewing a patient, the doctor pays special attention to the patient’s lifestyle, eating habits, smoking and alcohol abuse. After identifying complaints, the gastroenterologist determines the dynamics of symptoms. On examination, pale skin and tenderness of the abdominal wall may be observed.
Treatment of acidity disorders
If there are signs of low acidity, replacement therapy with enzyme preparations is prescribed. Its main task is to normalize the production of pepsin. Preparations containing acedin-pepsin help with this. Drug stimulation of gastric juice secretion is also necessary.
If the diagnostic results reveal increased acidity, the patient is prescribed antacids. They neutralize acid, weaken the activity of pepsin, and in some cases have an enveloping effect. To eliminate symptoms, medications are recommended that stimulate gastrointestinal motility and relieve spasms of smooth muscles. Additionally, you can use folk remedies - herbs, flax seeds, potato juice.
Why are gastroprotectors needed?
To prevent complications such as peptic ulcers and malignant tumors, it is important to keep the structure of the mucous membrane intact. Gastroprotectors are used for these purposes:
They should be taken when signs of gastritis appear. The doctor will determine which medications will fit into the selected treatment package. For prevention purposes, you do not need to drink them.
The stomach contains natural gastroprotectors - prostaglandins. They stimulate the formation of mucus, improve microcirculation and protect cells from destruction. If they are not produced enough, the gastroenterologist may prescribe their synthetic analogues. If the patient is being treated with non-steroidal anti-inflammatory drugs, drugs with prostaglandins prevent ulcerative lesions of the mucous membrane.
Complications
The main cause of complications is the chronic form of the disease. If signs of chronic gastritis appear, but the patient does not consult a doctor, the following complications may occur:
- anemia;
- atrophic gastritis;
- leptic ulcers;
- benign or malignant tumors on the mucosa.
The only way to restore health is to promptly consult a qualified doctor who will give recommendations on how to treat gastritis. Taking pills for gastritis on your own is not recommended, so as not to provoke an exacerbation of the disease and its transition to a severe form. The likelihood of complications depends on what patients with chronic gastritis eat.
Preventive measures
Since gastritis is now diagnosed not only in adults, but also in children, prevention should begin as early as possible. First of all, you should normalize your diet:
When the first symptoms of inflammation of the gastric mucosa appear, it is important to minimize (or better yet eliminate) the consumption of chocolate, coffee, spicy and fried foods.
Gastroenterologists recommend regularly checking for parasitic infestations. When they are detected, it is important to carry out timely treatment, because they often attack the digestive system.
How to make an appointment with a gastroenterologist
You can make an appointment with a gastroenterologist at our multidisciplinary medical center at 2nd Tverskoy-Yamskaya Lane, building 10 in the following ways:
- use the form on the website;
- use the phone +7 (495) 775-73-60 around the clock.
JSC "Medicine" (clinic of academician Roitberg) also offers services to call a gastroenterologist at home and by phone +7 (495) 775-73-60 around the clock.
JSC "Medicine" (clinic of academician Roitberg) is located a 5-minute walk from the "Mayakovskaya" metro station.