General information
Congenital anomalies of the development of the female genital organs, increasingly diagnosed by doctors recently, can become the main cause of the inability to conceive and bear a child.
The saddle shape of the uterus is one of these pathologies, which, according to statistics, is diagnosed in approximately 0.5% of women of childbearing age and can become a serious obstacle to happy motherhood. How to get pregnant with such a diagnosis? Is conception even possible with such a structure of the main female reproductive organ? How to carry a child to term if a saddle uterus is detected already during pregnancy ? We will answer these and other questions on the topic in this material. And to better understand the essence of the problem, we will start with general points regarding the structure of the female genital organs.
Diagnostics
As already noted, it is impossible to make a diagnosis by eye. The following research methods are needed:
- Ultrasound of the uterus and its appendages
Ultrasound does not always detect pathology. Those women who have a strongly pronounced saddle shape of the organ have a greater chance of receiving a correct diagnosis. It is better to do an ultrasound with a vaginal sensor. Visit a specialist in the second half of the cycle, when thickening of the endometrial layer is observed.
- Hysterosalpingography/hysterography
These are methods that use x-rays. Contrast is injected into the uterus, and then pictures are taken with special equipment. The doctor discovers a saddle-shaped depression on them.
- Hysteroscopy
A special optical device is inserted into the uterus, which makes it possible to examine the organ from the inside and understand if there are deviations or not. The method is very accurate in identifying abnormalities of the uterus in girls and women.
- MRI
This method also takes pictures of the uterus at different levels.
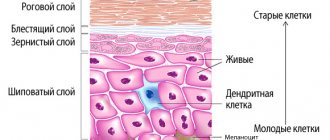
Structure and pathologies of uterine development
The uterus is a hollow organ that is designed for the development and bearing of a fetus. It is located in the middle part of the small pelvis, which also contains the bladder (in front), rectum (behind), cervix, uterine appendages and vagina (below). The shape of the uterus is pear-shaped, its length in women of childbearing age is on average 4-7 cm, thickness 4-5 cm, and width 4 cm.
The smooth muscle elastic uterine walls can significantly increase in volume during pregnancy, which allows the baby to grow normally in the mother's womb. The developed muscles of this organ take an active part in the birth process. We can say that it is the uterus that pushes the fetus out, thus triggering delivery.
Structure
- the uterine fundus is the convex upper part of the organ;
- the body of the uterus is the large cone-shaped part of the organ;
- The cervix is the lower rounded and narrowed part.
Developmental pathologies
- hypoplasia , i.e. underdevelopment of the organ, namely its small size (less than the norm for women who have given birth - 8 cm and for nulliparous women - 7 cm). In this condition, there is a general lag in the girl’s physiological development, as well as a painful menstrual cycle;
- uterine agenesis or aplasia is the absence (extremely rare) of this organ or its extremely small size, the so-called infantile uterus;
- The double uterine body occurs due to non-fusion or incomplete fusion of the “female” Müllerian ducts, which during embryonic development are responsible for the formation of the vagina, uterus and fallopian tubes. With complete nonfusion, a double set of genital organs will be observed, and with partial nonfusion, there will be two uteruses, one vagina, two or one cervix;
- bicornuate uterus , in which, due to the incomplete fusion of the same embryonic rudiments, an intrauterine septum with a vertical depression in the uterine fundus is formed.
In turn, the last of these anomalies is divided into three more types:
- incomplete uterus , i.e. divided into two horns identical in size and shape only in its upper third;
- complete uterus , i.e. divided into two horns, branched at an angle in different directions, at the level of the sacrouterine folds;
- saddle uterus , i.e. having a depression in the bottom, visually resembling a saddle with uterine horns fused together.
Symptoms
The following signs may indicate deviations in the anatomical development of a woman’s reproductive organs:
- menstrual dysfunction of various kinds, most often bleeding, dysmenorrhea;
- early miscarriages due to insufficient horn size and poor blood supply;
- inability to get pregnant for a long period.
Often the pathology does not produce pronounced symptoms; the woman learns about the anomaly during a gynecological examination.
Saddle uterus and conception
Let's talk in more detail about what this is a saddle uterus and how this defect in the development of a woman's internal genital organs will affect the possibility of conception. Saddle-shaped is a variant of a bicornuate uterus; the main characteristic feature of this structure is the presence of a split uterine fundus in the shape of a saddle.
The reasons for the appearance of this anomaly are not known for certain. Researchers only speculate, but cannot say with one hundred percent certainty what exactly contributes to its formation. But the mechanism for the development of pathology is known, which is associated with the earliest embryonic period of the intrauterine life of the fetus.
, responsible for the female genital organs, merge Their successful fusion leads to the formation of two vaginal-uterine cavities, separated from each other into left and right parts by a sagittal septum .
Saddle uterus, photo
At the end of intrauterine development, the septum resolves, and the uterus acquires its normal single-cavity structure. When something goes wrong, the merging mechanism fails. As a result, the uterus remains bicornuate or acquires a saddle shape.
Risk factors for the development of uterine pathologies:
- poor nutrition, lack of vitamins and beneficial compounds during pregnancy;
- hereditary predisposition;
- late toxicosis ;
- intoxication of a pregnant woman (harmful production, smoking, alcohol or drug addiction, use of certain medications);
- diseases of the endocrine system, for example , diabetes ;
- gestosis;
- diseases of the central nervous system;
- constant stress ;
- heart defects , which lead to chronic intrauterine hypoxia ;
- infectious diseases suffered during pregnancy ( influenza , rubella , cytomegalovirus , toxoplasmosis etc.).
There are no symptoms or clinical manifestations of this pathology. As a rule, women find out that they have a saddle uterus only at the planning stage (if infertility ) or during pregnancy. Unfortunately, such a deviation in the development of the internal genital organs can negatively affect the ability to have children.
Methods for diagnosing pathology
It is important to note that the saddle uterus is not a disease with obvious symptoms and can occur even in the healthiest women. During a routine examination, the gynecologist will not be able to detect this deviation, because This requires specialized equipment.
The following methods are used in diagnosis:
- Ultrasound examination of the uterine appendages and the uterus itself using a vaginal sensor. This method is effective only if the deformation is significant, and you can see on the device screen an increase in the width of the uterine fundus, as well as the thickness of the myometrium (the muscular lining of the organ). It is advisable to carry out an ultrasound examination of the pelvic organs in the second half of the menstrual cycle, when the endometrium (inner mucous layer) becomes thicker.
- Hysterography or hysterosalpinography is a procedure in which a special radiopaque substance ( Urotravist, Triombrast, Urografin ) or a solution of glucose, furatsilin or saline is injected into the uterine cavity, and then an X-ray or ultrasound . On an x-ray, the specialist will see the condition of the uterine cavity and its shape (for example, whether there are depressions), and will also check the patency of the fallopian tubes. Ultrasound also helps to judge the condition of the uterus, fallopian tubes and their patency by the presence or absence of injected fluid. After the procedure, the contrast agent is eliminated by urination by itself.
- Magnetic resonance imaging makes it possible to assess the condition of not only the poppy, its tubes and appendages, but also to obtain information about all nearby vessels and soft tissues. This diagnostic method helps to identify pathologies in the development of the internal genital organs, the presence of neoplasms, as well as disorders in the circulatory system.
- Hysteroscopy is a procedure in which a specialist examines the uterine cavity, its cervix and the openings of the fallopian tubes using an ultra-thin specialized optical device, a hysteroscope. This method also helps to determine the presence of pathologies in the development of the female genital organs, as well as to identify other painful conditions.
Doctors offer surgical treatment of the saddle uterus (reconstruction) in cases where a woman cannot become pregnant or her chances of carrying a child to term are sharply reduced. After all, after surgery, the chances of conceiving increase approximately tenfold. But such an extreme measure should be resorted to only when it is reliably known that it is the saddle uterus that is the cause of the impossibility of conception.
The thing is that this pathology is not always the only cause of infertility, because... many women were still able to get pregnant and give birth to healthy children. According to statistics, difficulties arise only when the deformation is pronounced and because of this the egg cannot attach to the uterine walls.
According to experts, an unexpressed saddle of the uterus cannot be the exclusive cause of infertility. Usually this pathology is observed in conjunction with other problems of the urogenital system. Therefore, in such cases, an integrated approach and a thorough medical examination helps.
4.Treatment
The decision on the need, plan and extent of surgical intervention (obviously, drug treatment in this case is absurd) is made on the basis of the clinical picture and a number of individual characteristics of a particular case. Of greatest importance is the volume of the single uterine cavity (excluding bifurcated “horns”), as well as the history of pregnancy, childbirth, artificial and spontaneous abortions. In some cases, surgical correction is indicated, in others it is recommended to resort to in vitro fertilization or surrogacy, in others the anomaly has virtually no effect on fertility and reproductive function, i.e. It is quite advisable to limit ourselves to observation tactics.
Sign up for a consultation
Poses for conception with a saddle uterus
On the Internet you can find a lot of conflicting information regarding what position you should prefer to get pregnant if you have a saddle uterus. On women's forums and in various groups, thousands of participants share their experiences and are widely mistaken that conception requires some special favorable position.
Doctors say this is complete nonsense. After all, nature created the female and male genital organs in such a way that, no matter the type of physical intimacy, a healthy female body could easily become pregnant. If, no matter how hard you try, nothing comes of it, you definitely need to look for the cause in the state of health of both partners, and not think about the correctness or incorrectness of the position of the bodies during sex.
Features in the structure of the saddle uterus do not prevent sperm from penetrating the fallopian tubes to meet the egg - this is an indisputable fact. The point here is whether the fertilized egg can attach to the uterine walls in a favorable place and survive in order to further develop harmoniously.
Removal of the intrauterine septum
Surgical removal of the septum in the uterus is the main treatment method for this pathology offered in our clinic. The hysteroresectoscopy procedure involves dissection and excision of a septum of sufficiently large thickness and density. Today, more modern methods of treating intrauterine septums are also practiced, which include cutting them with a laser.
With a complete septum reaching the internal os of the cervix, its cervical part is usually not affected during surgical treatment. This is done in order to avoid the development of subsequent isthmic-cervical insufficiency.
Surgical removal of the intrauterine septum is a low-traumatic surgical intervention that does not leave scars. This means that after such treatment nothing will interfere with normal conception, pregnancy and natural delivery.
After surgery, the risks of miscarriage and the development of other obstetric complications are significantly reduced. However, pregnancy management in women after removal of the intrauterine septum requires close attention of obstetricians and gynecologists.
Types of adenomyosis
Depending on the distribution of pathological structures in the affected tissues, the following forms of adenomyosis are distinguished:
- Diffuse manifests itself as a uniform distribution of small inclusions of the endometrium throughout the muscular layer of the uterus;
- With the nodular type of disease, endometrioid nodes filled with blood are formed in the muscle layer;
- The focal form of adenomyosis is characterized by the formation of small accumulations of endometrial cells in various areas of the uterus.
Take the first step
make an appointment with a doctor!
There is also a cystic form, which is a further development of nodular or focal adenomyosis and is formed when the nodes hemorrhage followed by the formation of cysts. These types of this pathology can form separately or in combination with each other. The most common form is a diffuse nodular form, in which endometrial cells form a node and areas with their uniform inclusion.
There are also several stages of development of this disease, characterized by the degree of damage to the uterine tissue:
- stage 1 - at this stage, endometrial tissue penetrates only the thinnest layer of the myometrium (muscular wall) of the uterus;
- stage 2 - the pathological process penetrates deeper into the muscle wall, consisting of 3 layers, affecting 2 of them;
- stage 3 - the endometrium extends to all 3 layers of the myometrium up to the serous membrane of the uterus, which borders the surface of the bladder;
- stage 4 - endometrial tissue penetrates the uterine myometrium and affects adjacent organs, causing external gynecological endometriosis.
The signs of uterine adenomyosis and its damage to the body depend on the stage of the disease. Determining the stage of development of pathology plays an important role in its diagnosis and treatment. The earlier it is detected, the more effective and gentle the therapy will be.